Actinic porokeratosis effectively treated with nivolumab immunotherapy
Siham Belmourida , Brigitte Dreno
, Brigitte Dreno
Department of Dermatology and Venerology, Nantes University Hospital, Nantes, France
Corresponding author: Siham Belmourida, MD
How to cite this article: Belmourida S, Dreno B. Actinic porokeratosis effectively treated with nivolumab immunotherapy. Our Dermatol Online. 2021;12(3):333-334.
Submission: 06.11.2020; Acceptance: 12.02.2021
DOI: 10.7241/ourd.20213.26
Citation tools:
Copyright information
© Our Dermatology Online 2021. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Actinic porokeratoses form a heterogeneous group of dermatological conditions secondary to an epidermal keratinization disorder [1,2].
We report the case of a patient with actinic porokeratoses associated with a locally advanced squamous cell carcinoma of the face treated successfully with nivolumab (anti-PD-1).
A 71-year-old patient, followed for actinic porokeratoses for twenty years and treated with retinoids and vitamin B, was referred to the oncodermatology services of the University Hospital of Nantes for the management of an infiltrating squamous carcinoma of the right cheek.
A clinical examination found a patient, otherwise in good general condition, with an ulcerative mass on the right cheek with several diffuse erythematous scaly lesions throughout the body in relation to the patient’s actinic keratosis. An examination of the areas of the lymph nodes failed to find adenopathy. The rest of the somatic examination was unremarkable. The biological balance was free of anomaly and a radiological examination did not find a metastasis elsewhere.
An anti-PD-1 treatment with nivolumab at a dose of 240 mg every two weeks helped to stabilize the patient’s squamous cell carcinoma and cure his actinic porokeratoses after four months of treatment (Figs. 1a – 1c).
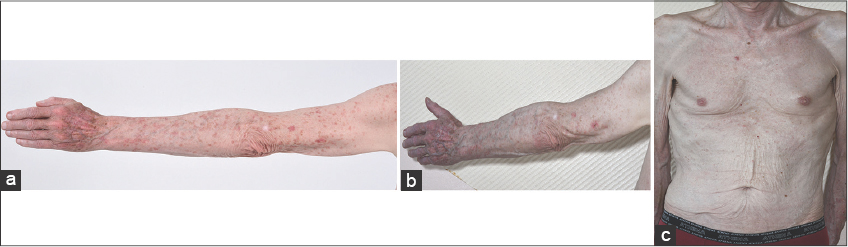 |
Figure 1: The good clinical evolution of the actinic porokeratosis under immunotherapy with nivolumab (anti-PD-1) (a) before and (b-c) after. |
Actinic porokeratoses are generally resistant to usual treatments and pose a difficulty in their therapeutic management. The risk of degeneration varies depending on the clinical form, ranging from 7% to 19% [1]. The efficacy of anti-PD-1 therapy on skin squamous cell carcinomas and xeroderma pigmentosum has already been reported but has not yet been well illustrated in the management of actinic porokeratoses. The first resolved case of actinic porokeratosis under immunotherapy was reported by Salomon et al. in 2017 [1]. The etiopathogenesis of this condition is not yet well understood. Genetic factors have been suspected in familial forms. Other studies found chromosomal instability in fibroblasts in people with porokeratotic lesions after sun exposure. Treatment usually involves keratolytics, destructive agents, local chemotherapy with 5-fluorouracil, or immunosuppressing treatment with imiquimod, which rarely lead to a complete regression. In our case, immunotherapy led to the improvement of the squamous cell carcinoma as well as the healing of the patient’s resistant actinic porokeratoses [2,3].
Further specialized studies would be necessary in order to explore the efficacy and pathophysiological mechanism of this therapeutic option.
Immunotherapy may be an effective therapeutic option for chronic porokeratoses resistant to usual treatments.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Salomon G, Riffaud L, Boulinguez S, Sibaud V, Meyer N. Resolute porokeratosis actinic on immunotherapy:Case report. Ann Dermatol Venereol. 2017;144:S164-5.
2. Yatim A, Bohelay G, Lévy A, Costa C, Maubec E, Caux F. Disseminated superficial actinic porokeratosis with mutation of mevalonate kinase:First case in a Caucasian. Ann Dermatol Venereol. 2017;144:S94-5.
3. Souza PRM, Furtat TM, Reinisch N, Dario PHP. Scratching suspected porokeratosis lesion, simple and quick maneuver that facilitates its diagnosis. Our Dermatol Online. 2019;10:367-8.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-2795-9161 http://orcid.org/0000-0002-2795-9161 |



Comments are closed.