Cutaneous lupus tumidus: An unusual unilateral presentation
Samia Mrabat 1, Hanane Baybay1, Zakia Douhi1, Sara Elloudi1, Fatima Zahra Mernissi1, Mouna Rimani2
1, Hanane Baybay1, Zakia Douhi1, Sara Elloudi1, Fatima Zahra Mernissi1, Mouna Rimani2
1Department of Dermatology, University Hospital Hassan II, Fes, Morocco, 2Hassan Center of Pathology, Rabat, Morocco
Corresponding author: Samia Mrabat, MD
Submission: 26.12.2020; Acceptance: 07.02.2021
DOI: 10.7241/ourd.20212.10
Cite this article: Mrabat S, Baybay H, Douhi Z, Elloudi S, Mernissi FZ, Rimani M. Cutaneous lupus tumidus: An unusual unilateral presentation. Our Dermatol Online. 2021;12(2):151-152.
Citation tools:
Copyright information
© Our Dermatology Online 2021. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Lupus tumidus is a rare subtype of chronic cutaneous lupus erythematosus characterized by erythema and bright urticarial erythematous and violaceous lesions on sun-exposed areas that heal without leaving scars. Lupus tumidus follows a benign and intermittent clinical course and is rarely associated with systemic lupus erythematosus. Treatment involves photoprotection, topical corticosteroids, and antimalarials. We report the case of a 42-year-old patient with an atypical unilateral form of lupus tumidus successfully treated with the administration of hydroxychloroquine in combination with photoprotection and tacrolimus.
Key words: Lupus erythematosus; Autoimmune diseases; Antimalarials
INTRODUCTION
Lupus erythematosus is a multisystemic autoimmune disease characterized by the production of autoantibodies against cellular constituents. The most affected organ is the skin, which may be involved in isolation or accompanied by systemic manifestations [1]. Cutaneous manifestations of lupus may be classified into the following: chronic cutaneous lupus erythematosus (CCLE), subacute cutaneous lupus erythematosus (SCLE), and acute cutaneous lupus erythematosus (ACLE). Lupus tumidus is considered a separate entity, showing a marked response to treatment with antimalarial drugs, extreme photosensitivity, and characteristic histopathologic findings [2].
CASE REPORT
A 52-year-old male with no history of comorbidity and medication presented himself with a slightly itchy lesion on the face persistent for twelve months. The lesion emerged as an erythematous macule, later evolving into an infiltrated erythematous lesion. There were no other systemic signs, such as photosensitivity or arthralgia. The patient reported a lack of improvement after the application of a topical corticosteroid. An examination of the face revealed a well-limited erythematous plaque roughly 4 cm in size on the left malar region (Fig. 1). A skin biopsy revealed deep perivascular and periadnexal lymphocytic infiltration of the skin (Fig. 2) and papillary edema with mucinous dispositions (Fig. 3), thus confirming the diagnosis of cutaneous lupus tumidus. The patient was started on antimalarials, photoprotection measures, and tacrolimus with great improvement.
 |
Figure 1: Well-limited erythematous plaque on the left malar region. |
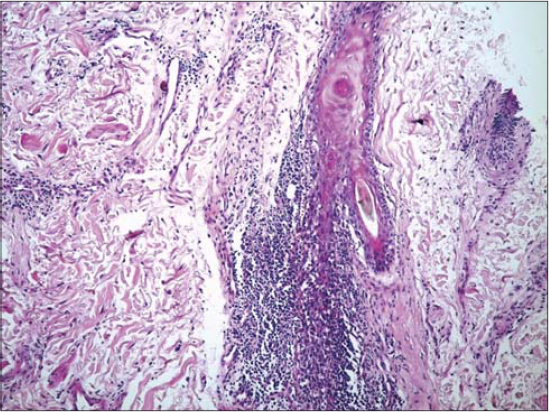 |
Figure 2: Periadnexal lichenoid infiltrate. |
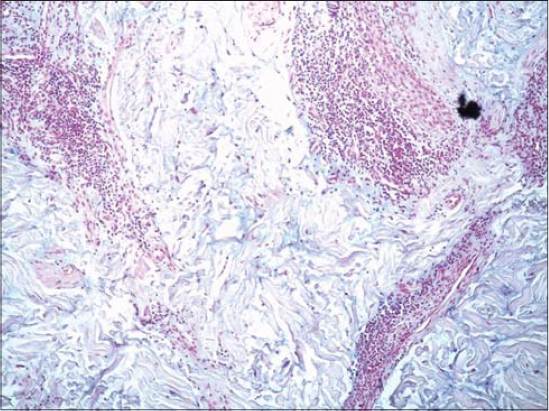 |
Figure 3: Moderate alkaliphilic mucinous deposits in the dermis. |
DISCUSSION
The term lupus erythematosus tumidus (LET) was first used by Gougerot and Burnier in 1930 to describe infiltrated erythematous lesions with no clinical signs of desquamation or other superficial changes [3]. Lupus erythematosus tumidus may begin at any age, including childhood, but, according to one study, the mean age of onset is 36.4 years. The majority of patients with LET are extremely photosensitive [4]. Lupus erythematosus tumidus may clinically mimic other skin disorders, such as polymorphous light eruption, pseudolymphoma, and Jessner lymphocytic infiltration. A histopathological examination of these skin lesions is, therefore, required to confirm the diagnosis. LET differs from the other conditions mainly by dermal mucin deposition and the lack of dermal edema [5]. Most patients with LET successfully respond to antimalarials and sunscreen. Other treatments, including topical or systemic corticosteroids and immunosuppressive agents, have been demonstrated to be effective [6].
CONCLUSION
Our case emphasizes the importance of detailed clinical examination as well as histopathological analysis in the diagnosis of this rare form of cutaneous lupus.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Bousquet Muylaert BP, Braga BB, Esteves EB, Garbelini LE, Michalany AO, Oliveira J Filho. Lupus tumidus:A report of two cases. An Bras Dermatol. 2016;91(5 suppl 1):87-9.
2. Rodriguez-Caruncho C, Bielsa I, Fernández-Figueras MT, Roca J, Carrascosa JM, Ferrándiz C. Lupus erythematosus tumidus:A clinical and histological study of 25 cases. Lupus. 2015;24:751-5.
3. Patsinakidis N, Kautz O, Gibbs BF, Raap U. Lupus erythematosus tumidus:Clinical perspectives. Clin Cosmet Investig Dermatol. 2019;12:707-19.
4. Filotico R, Mastrandrea V. Cutaneous lupus erythematosus:Clinico-pathologic correlation. G Ital Dermatol Venereol. 2018;153:216-29.
5. Bakardzhiev I, Chokoeva AA, Krasnaliev I, Tana C, Wollina U, Lotti T, et al. Unilateral unique Lupus tumidus:Pathogenetic mystery and diagnostic problem. Wien Med Wochenschr. 2016;166:250-3.
6. Gallitano SM, Haskin A. Lupus erythematosus tumidus:A case and discussion of a rare entity in black patients. JAAD Case Rep. 2016;2:488-90.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0002-5942-441X http://orcid.org/0000-0002-5942-441X |



Comments are closed.