Erythema induratum of Bazin: A study of 34 cases in an endemic country
Ibtissam Assenhaji Louizi , Hanane Baybay, Safae Zinoune, Zakia Douhi, Sara Elloudi, Fatima Zahra Mernissi
, Hanane Baybay, Safae Zinoune, Zakia Douhi, Sara Elloudi, Fatima Zahra Mernissi
Dermatology Service, Hospital Hassan II in Fez, Fez, Morocco
Corresponding author: Dr. Ibtissam Assenhaji Louizi
Submission: 21.12.2019; Acceptance: 23.02.2020
DOI: 10.7241/ourd.20204.6
Cite this article: Assenhaji Louizi I, Baybay H, Zinoune S, Douhi Z, Elloudi S, Mernissi FZ. Erythema induratum of Bazin: A study of 34 cases in an endemic country. Our Dermatol Online. 2020;11(4):360-362.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Cutaneous tuberculosis represents 1–2% of cases of tuberculosis. The purpose of this work is to reevaluate the epidemiological and clinical profile and the therapeutic and evolutionary paraclinical understanding of this entity in Fes, Morocco.
Materials and Methods: The following was a descriptive and retrospective study conducted from January 2006 through April 2018 at the Dermatology Department of Hassan II CHU in Fes, Morocco, and Diagnostic Centers for Tuberculosis and Respiratory Diseases.
Results: We identified 34 cases of an average age of 48 years and a sex ratio of 0.03. Chronic nodular hypodermitis of the lower limbs leaving pigmented scars was found in 100% of cases and fistulized in 52.9%. IDR was phlyctenular in 47% of cases. Cutaneous histology revealed an inflammatory granuloma with vasculitis in 32.35% of cases. All the patients received antibacterial treatment for six months. Recidivism was found in 20.5% of cases. Treatment with dapsone was prescribed for these patients with good evolution.
Conclusion: Confronted with chronic nodular hypodermitis of the legs, the clinician must consider the origin of tuberculosis, keeping in mind epidemiological, clinical, histological, and immunological findings.
Key words: Bazin’s indurated erythema, Tuberculous, Epidemiological profile, Clinical profile, Therapeutic
INTRODUCTION
Cutaneous tuberculosis is still common in Morocco, representing 1–2% of cases of tuberculosis and 0.1–1% of skin diseases [1]. Erythema induratum of Bazin (BEI) is a nodular vasculitis but still poses a problem as to its tuberculous origin. Its management remains poorly understood [2]. The purpose of this work is to reevaluate the epidemiological and clinical profile and the therapeutic and evolutionary paraclinical understanding of this entity in the region of Fes, Morocco.
MATERIAL AND METHODS
This is a prospective and retrospective study conducted at the Dermatology Department of Hassan II CHU in Fes, Morocco, and Diagnostic Centers for Tuberculosis and Respiratory Diseases (DCTRD) on cases of cutaneous tuberculosis hospitalized from January 2006 through April 2018. Selected files were analyzed according to a grid with epidemiological, clinical, paraclinical, and therapeutic data.
RESULTS
We identified thirty-four cases of IBS. The average age was 48 years, with extremes ranging from 21 to 70 years. The sex ratio was 0.03, with a high female predominance of 30 females per male. The majority of the patients came from rural areas and were of low socioeconomic status.
Tuberculous contagion was present in the patients’ history. One patient had a history of pulmonary tuberculosis but no family history. No cases of HIV infection were identified. The average duration of evolution was two years.
Clinically, all patients had chronic nodular hypodermitis of the lower limbs, fistulized in eighteen cases (Fig. 1), leaving pigmented scars in all patients (Fig. 2).
 |
Figure 1: Chronic nodular hypodermitis of the lower limbs. |
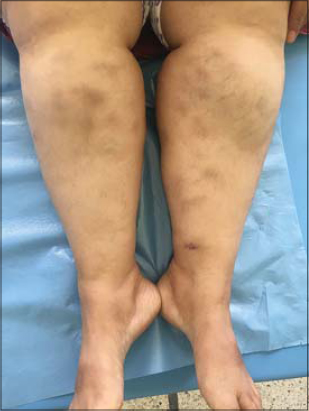 |
Figure 2: Pigmented scars after BEI lesions on the lower limbs. |
The intradermal tuberculin reaction was phlyctenular in sixteen patients (Fig. 3). Cutaneous histology revealed an inflammatory granuloma of the lipophagic type associated with vasculitis in eleven cases.
 |
Figure 3: The phlyctenular reaction of intradermal tuberculin. |
A search for Koch’s bacillus in skin lesions by PCR (polymerase chain reaction) was not conducted
All patients received antibacterial treatment for six months, with complete healing in 29 patients and recidivism in seven. Treatment with dapsone was prescribed for these patients with good evolution and without recurrence after six months.
DISCUSSION
Cutaneous tuberculosis has a protean clinical presentation, representing 1% of cases of extrapulmonary tuberculosis in endemic areas [3].
Erythema induratum of Bazin (BEI) was first described by Ernest Bazin in 1861 and, thereafter, in 1900, BEI was considered a manifestation of tuberculin hypersensitivity [1]. Currently, the term nodular vasculitis (NV) is often synonymous. The number of cases of BEI reported is on the decrease in most developed countries while the incidence of tuberculosis is decreasing [1].
The pathogenesis of BEI remains poorly understood and its link to tuberculosis remains controversial. Most authors consider BEI a multifactorial disorder with multiple different causes, tuberculosis essentially being a hypersensitive immune response to M. tuberculosis [4,5].
EIB is a recurrent chronic eruption occurring in young and middle-aged females in good health and with no systemic signs. EIB manifests itself by the presence of purple nodules or deep plaques on the posterior and anterolateral legs, feet, thighs, and arms, with the face rarely affected [1]. The lesions are not warm and not especially painful and tend to ulcerate centrally. Most of the lesions resolve spontaneously within several months, leaving postinflammatory hyperpigmentation and pigmented scars, which were found in all our patients [1].
Histologically, the epidermis may be intact or ulcerated. Lobular panniculitis with granulomatous inflammation with focal necrosis, sometimes with tuberculoid granulomas, and with central caseous necrosis [1] and a superficial or deep, perivascular or periadnexal, inflammatory lymphohistiocytic infiltrate is often present. Vasculitis of small and medium-sized vessels with fibrinoid necrosis and purpura may appear [1]. Special stains demonstrate no presence of acid-fast bacilli, but detection of M. tuberculosis by PCR suggests the presence of tuberculous DNA in the lesions [6].
However, because assessments conducted often do not provide sufficient evidence for the origin of tuberculous cutaneous lesions, it is necessary to employ the notions of endemic countries, recent tuberculosis contagion, positivity of IDR to tuberculin, and association with extracutaneous tuberculosis [7].
The management of BEI is poorly documented [8], but involves standard WHO anti-TB drugs (four-drug therapy, then dual therapy for six months), Generally, cutaneous TB must be treated with the same regimen as systemic TB, and there is no role for single anti-TB drugs [1]. However, with the high risk of recidivism and in the case of the failure of antibacterial treatment, dapsone may be a good therapeutic alternative, as in our study [7].
CONCLUSION
Confronted with chronic nodular hypodermitis of the legs, the clinician must consider the origin of tuberculosis, keeping in mind epidemiological, clinical, histological, and immunological findings, especially after good evolution with anti-tuberculosis drugs. Nevertheless, a study with larger sampling is desirable.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Merza A, Adham DK, Yaqo RT. Unusual recurrent skin lesions:Bazin’s disease Muayad. Int J Community Med Public Health. 2019;6:879-82.
2. Nakouri I, Litaiem N, Jones M, Raboudi A, Hariz A, Jaziri F, et al. Erythème induréde Bazin dans un pays d’endémie tuberculeuse. Rev Méd Inter. 2017;38S:A109–A248.
3. Tafani C, Lecoules S, Carmoi T, Tuleja E, Algayres J-P. Hypodermite nodulaire chronique des jambes d’origine tuberculeuse. Rev Méd Inter. 2012;33:141.
4. Xu H, Li YM, Ma H, Gu WT, Chen ZQ. Mycobacterium tuberculosis found at both skin lesions and Mantoux testing site in a patient with erythema induratum of Bazin. J Dermatol. 2017;44:1145-7.
5. Posada Garc?a C, Pena A, Anibarro L, Pardavila RM, De La Torre C, Gonzalez-Fernandez A. Erythemainduratum of Bazin induced by tuberculin skin test. Int J Dermatol. 2015;54:1297–9.
6. Biman P, Sin C, Wann A-R, Grossin M, Courdavault L, Sigal M-L, et al. Tuberculose cutanée et érythème induréde bazin:étude rétroscpectivede 13 cas. Elsevier Masson. 2015:0151-9638.
7. Labbardi W, Hali F, Chiheb S. Érythème induréde Bazin:étude anatomoclinique de 32cas. J Ann Dermatol. 2015;10:316.
8. Ben Salem T, Khedher M, Lamloum M, Ben Ghorbel I, Houman MH. Aspects cliniques, anatomopathologiques et thérapeutiques de l’érythème induréde Bazin dans un pays d’endémie tuberculeuse. Revmed. 2018;03:073.
Notes
Source of Support: Nil.
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/000-0003-3455-3810 http://orcid.org/000-0003-3455-3810 |



Comments are closed.