Molluscum contagiosum mimicking sebacious hyperplasia
Bobak Hedayati 1, Manuel Valdebran2, Amira Elbendary3, Ruzeng Xue4
1, Manuel Valdebran2, Amira Elbendary3, Ruzeng Xue4
1University of California Irvine, School of Medicine, Irvine, California, USA. 2Department of Dermatology, University of California Irvine, Irvine, California. USA. 3Department of Dermatology, Kasr Alainy Faculty of Medicine, Cairo University, Egypt. 4Department of Dermatology, Dermatology Hospital, Southern Medical University, Guangzhou, China
Corresponding author: Bobak Hedayati, E-mail: BOBAKH@hs.uci.edu
Submission: 05.09.2019; Acceptance: 12.11.2019
DOI: 10.7241/ourd.20202.31
Cite this article: Hedayati B, Valdebran M, Elbendary A, Xue R. Molluscum contagiosum mimicking sebacious hyperplasia. Our Dermatol Online. 2020;11(2):210-211.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
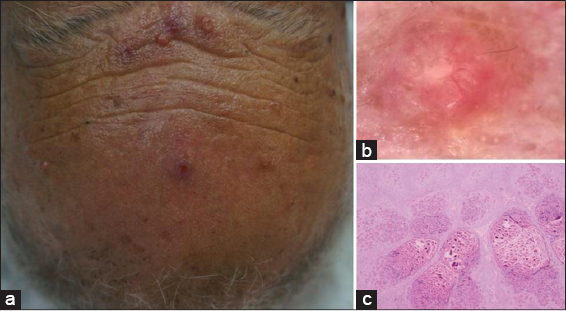
A 61-year-old male presented to our clinic with several papules on the face for 6 months. Past medical history was unremarkable. Upon physical examination 4-7 mm yellowish dome-shape papules were found. Dermoscopy revealed umbilicated pinkish lobular structures at the center of the lesion surrounded by erythema. In addition, small radial vessels were noted. Histopathologic examination revealed dermal amphophilic squamous proliferation containing numerous eosinophilic intracytoplasmic bodies (Fig. 1).
Molluscum Contagiosum (MC) is one of the most common viral skin infections in the world. The molluscum contagiosum virus (MCV) that causes the disease, is a poxvirus that specifically targets the keratinocytes in the epidermis [1]. The virus is thought to evade the immune system, at least temporarily, as it remains superficial to the dermal-epidermal junction leading to hyperplasia of the epidermal layer. On the skin, lesions present as 3-5mm skin-colored papules, each usually with a characteristic central umbilication that can arise anywhere on the body [2]. In adults, a common form of transmission is via sexual contact and as a result, lesions are often found on the genitals. However, MCV can be auto-inoculated onto other areas of the body as well [2].
Presentation in immunocompromised patients, older patients and patients with presentation in the head and neck may be difficult to diagnose clinically [3].
The dermatoscope is a useful tool for identifying the vascular pattern of MC. One study reported that roughly 89% of MC lesions had some type of vascular pattern which could be classified into one of four Sir,groups: crown, punctiform, radial, and mixed [4]. Sebaceous hyperplasia, has its own unique dermoscopic features including a characteristic milky, cloud-like raised globular structure with asymmetric borders and a variable vascular pattern that can be branching or nonbranching [5]. On histopathology, MC most classically presents with a central invagination that is representative of the characteristic umbilication. The keratinocytes within the lesion contain viral inclusions in the cytoplasm, called Molluscum Bodies. These can grow so large that they often displace the nuclei peripherally and can range from eosinophilic to basophilic in color. They initially are found in the keratinocytes near the basal layer then progress toward the more superficial layers of the epidermis [3].
Our patient has a somewhat unique presentation for a few different reasons. First, his lesions ranged from 4-7mm. We observed pinkish lobular structures at the center of the lesion surrounded by erythema.
In conclusion, MC is a self-resolving disease in immunocompetent individuals, however, it can be spread via direct skin contact. Therefore, it is important to properly diagnose these lesions when they present. As with many diseases, MC has classic and non-classic presentations. It is imperative that physicians are aware of the less common clinical, dermatoscopic and histopathologic variations that can manifest from this disease.
REFERENCES
1. Chen X, Anstey A V, Bugert JJ. Molluscum contagiosum virus infection. Lancet Infect Dis. 2013;13:877-8.
2. Nguyen HP, Franz E, Stiegel KR, Hsu S, Tyring SK. Treatment of molluscum contagiosum in adult, pediatric, and immunodeficient populations. J Cutan Med Surg. 2014;18:299-306.
3. Ishikawa MK, Arps DP, Chow C, Hocker TL, Fullen DR. Histopathological features of molluscum contagiosum other than molluscum bodies. Histopathology. 2015;67:836-42.
4. Ianhez M, Cestari S da CP, Enokihara MY, Seize MB de PM. Padrões dermatoscópicos do molusco contagioso:estudo de 211 lesões confirmadas por exame histopatológico. An Bras Dermatol. 2011;86:74-9.
5. Bryden AM, Dawe RS, Fleming C. Dermatoscopic features of benign sebaceous proliferation. Clin Exp Dermatol. 2004;29:676-7.
Notes
Source of Support: Nil.
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|



Comments are closed.