Herpes simplex mastitis: A rare complication of paediatric orolabial herpes
Radhika Varma , Rony Mathew, Amitha Abraham
, Rony Mathew, Amitha Abraham
Department of Dermatology Venereology and Leprosy, Government Medical College, Alappuzha, India
Corresponding author: Dr. Radhika Varma, e-mail: drradhikavarma@gmail.com
Submission: 30.08.2019; Acceptance: 12.11.2019
DOI: 10.7241/ourd.20202.17
Cite this article: Varma R, Mathew R, Abraham A. Herpes simplex mastitis: A rare complication of paediatric orolabial herpes. Our Dermatol Online. 2020;11(2):177-179.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Herpes simplex virus is a highly contagious virus belonging to the Herpesviridae family. The infection is primarily transmitted through direct mucocutaneous contact with either oral or genital lesions of an infected individual. The transmission of virus from mother to child is well known and mostly occur during the delivery when the neonate’s skin is exposed to either mother’s vaginal secretions or to the active herpetic lesions on the genital tract. The transmission of infection in the reverse order (i.e. from the child to mother) has been rarely reported in literature. Herein, we report the bilateral occurrence of herpetic breast infection in a lactating mother who acquired it from oro-labial herpes infection in her daughter.
Key words: Herpes mastitis; Orolabial herpes; Herpes simplex
INTRODUCTION
Herpes simplex virus (HSV) infection is very common worldwide [1]. Generally, HSV type-1 affects the head and neck area, whereas the HSV type-2 tends to be associated with genital disease [2]. The viral inoculation occurs through micro abrasions of skin or mucosa during close contact with an infected person and causes a myriad of clinical presentations with varying severity [3]. The characteristic feature of herpes virus is their ability to establish latency following primary infection and the potential to reactivate upon triggers [4]. Not all patients exposed to the virus develop clinical disease and also majority of HSV-1 infection remain subclinical [3,4]. Herpes simplex is a rare cause of breast infection and published reports are extremely limited [2,3,5,6]. The mostly highlighted cause of herpes simplex mastitis is the infant to maternal transmission during breastfeeding [2]. We report a similar case of mammary infection with herpes simplex from oro-labial herpes in baby.
CASE REPORT
A 24 year old lactating mother presented with history of multiple painful erosions in areola and fissuring of both nipples since one week. Lesions first appeared on right side accompanied by mild serous nipple discharge and that on the left side developed two days later. There was no history of any lesions in other body parts. She did not have any constitutional symptoms. She was on oral antibiotics, analgesics and topical zinc oxide based dressings with a diagnosis of nipple eczema in spite of which the symptoms were progressing. On examination, the erosions on nipple areolar region were tender, shallow, mostly coalesced in areola and had a striking polycyclic border. There were three vesicles in the periphery of erosions on right areola with turbid fluid (Figs. 1 and 2). There was no palpable mass in the breasts or regional lymphadenopathy. Her general condition was good and the systemic examination did not reveal any abnormality.
 |
Figure 1: Coalesced and discrete erosions on areola and nipple of right breast. Polycyclic border is obvious. |
 |
Figure 2: Closer view of vesicles on periphery of erosion on right breast. |
On further enquiry, a history of painful erosions in oral cavity of her 18 month old baby which interfered with breast feeding two weeks back could be elicited. It was diagnosed as hand foot and mouth disease by a physician but no medical records were available. She reported complete clearance of lesions in one week with ayurvedic treatment. Physical examination of the child revealed a partially healed oval erosion just above the vermilion border of upper lip on left side reminiscent of a possible healed oro-labial herpes to our suspicion (Fig. 3). Hence, in correlation, a diagnosis of maternal herpes simplex mastitis was suspected in mother.
 |
Figure 3: Partially healed oval shaped erosion above vermilion border of upper lip on left side. |
The air dried preparation of scrapings from the vesicle base and the erosions on areola stained with Leishman stain showed multinucleated giant cell with ground glass nucleus and a few acantholytic keratinocytes suggestive of herpetic etiology (Fig. 4). Biopsy of the lesion and culture of herpes simplex virus could not be done. The patient was treated with oral acyclovir for seven days with complete resolution of her symptoms and there was good re-epithelization.
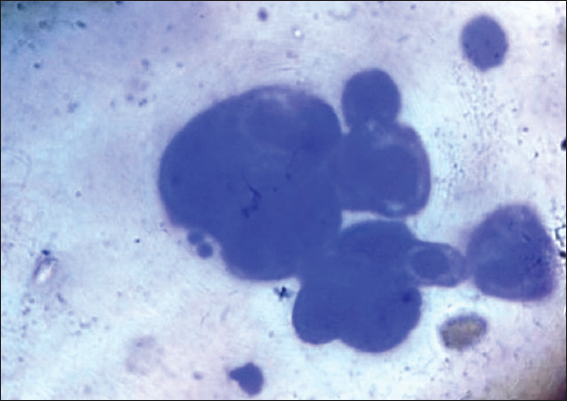 |
Figure 4: Smear from erosions showing a multinucleated giant cell with several acantholytic keratinocytes. Leishman stain, 100x magnification. |
DISCUSSION
Herpes mastitis is a little-known disease. Only 2% of all extragenital herpetic lesions have involved the breast [7]. Trauma facilitates the transmission of herpes and skin lesions commonly develop at the sites of erosions or break in the continuity of the skin [3].
Three main modes of transmission of herpetic infection to breast include: (i) infant-maternal transmission during breastfeeding, (ii) autoinoculation, and (iii) by sexual contact [2]. There is little information regarding transmission of HSV to the breast except in cases associated with neonatal breast feeding [7].
The transmission of the HSV by contact with an asymptomatic HSV carrier is also described as the partner can carry the virus in the saliva without any obvious clinical manifestation [7].
Herpes simplex virus infection is common in neonatal and pediatric populations [3,4]. In immunocompetent children, the primary mucocutanoeous infection is typically self limiting in about 10 to 21 days. The virus remain latent in nerve or the ganglion cells and causes lifelong infection with episodic clinical symptoms [4]. It is possible that frequent antigenic stimulation occurs in at least some cases of recurrent herpetic infections [5]. Viral shedding may continue even after resolution of clinical symptoms.
The diagnosis of isolated herpes simplex mastitis is very difficult as it can mimic others pathologies of breast like paget’s disease, contact dermatitis, inflammatory carcinoma, or other bacterial or varicella zoster mastitis [2,7].
In the present case, probably the trauma induced by the sucking of the nipples by the baby might have facilitated the development of lesions during the period of viral shedding. A few cases of maternal breast infection following breastfeeding have been documented in literature [2,6–10]. Usually, lesions are restricted to areola although cases with entire mammary involvement have been described. The majority of mastitis are due to HSV type-1 and those with HSV type-2 remain exceptional [2]. Various methods for diagnosis of herpes infections which are available include the cytodiagnosis by Tzanck test, immunohistochemistry of tissue specimen, serology for HSV, in-situ hybridisation, PCR and viral culture. Viral isolation by culture remains the gold standard procedure. However, Tzanck test prove to be a method with good sensitivity and specificity for diagnosing herpetic infection [2,7].
As this infection is uncommon, no therapeutic guidelines exists. Acyclovir, a guanosine analogue is an approved agent which reduces the viral replication by inhibiting the viral DNA synthesis [2]. In the background of our case, we highlight the need for a high index of suspicion of this entity in all cases of non healing erosive breast disease in both lactating and non-lactating females. Also, all breast-feeding mothers whose children are suffering from herpetic gingivostomatitis should be cautioned of this complication well in advance to limit the morbidity of herpes mastitis. Factors other than trauma which influences this unusual mode of transmission need to be studied so that appropriate preventive measures can be suggested as refraining from breast feeding may not be practically possible in all scenarios. Future directions for safe feeding practices and vaccination strategies in high risk lactating women need to be explored to limit the substantial morbidity of herpes simplex mastitis.
We also recommend a routine analysis of suspicious lesions by a Tzanck test as it remains a fairly reliable, easy, quick, and inexpensive diagnostic test in clinical settings.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Xu F, Lee FK, Morrow RA, Stenberg MR, Luther KE, Dubin G, et al. Seroprevalence of herpes simplex virus type 1 in children in United states. J Pediatr. 2007;151:374-77.
2. Toussaint A, Simonson C, Valla C. Herpes mastitis:diagnosis and management. Breast J. 2016;22:335–38.
3. Gupta S, Malhotra AK, Dash SS. Child to mother transmission of herpes simplex virus-1 infection at an unusual site. JEADV. 2008;22,:875–903.
4. James SH, Whitley RJ. Treatment of herpes simplex virus infections in pediatric patients:current status and future needs. Clin Pharmacol Ther. 2010;88:720-4.
5. Nahmias AJ, Roizman B. Infection with herpes-simplex viruses 1 and 2. N Engl J Med. 1973;289:719–25.
6. Soo MS, Ghate S. Herpes simplex virus mastitis:clinical and imaging findings. AJR Am J Roentgenol. 2000;174:1087–88.
7. Mardi K. Gupta N, Sharma S, Gupta S. Cytodiagnosis of herpes simplex mastitis. Report of a rare case. J Cytol. 2009;26:149-50.
8. Quinn PT, Lofberg JV. Maternal herpetic breast infection:another hazard of neonatal herpes simplex. Med J Aust. 1978;2:411–12.
9. Sealander JY, Kerr CP. Herpes simplex of the nipple:infant-to-mother transmission. Am Fam Physician. 1989;39:111-13.
10. Dekio S, Kawasaki Y, Jidoi J. Herpes simplex on nipples inoculated from herpetic gingivostomatitis of a baby. Clin Exp Dermatol. 1986;11:664-6.
Notes
Source of Support: Nil.
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|



Comments are closed.