Beta-blocker bisoprolol induced psoriasis
Ramin Mofarrah1,2, Ramina Mofarrah3, Kousar Jahani Amiri4, Mona Mohammadi Tabar4, Birger Kränke 5
5
1Austria Board Certified Dermatologist and Venereologist, Islamic Azad University, Sari, Iran; 2Department of Dermatology, Faculty of Medicine, Islamic Azad University, Sari, Iran; 3Student Research Committee, Shiraz Branch, University of Medical Sciences, Shiraz, Iran; 4Student Research Committee, Sari Branch, Islamic Azad University, Sari, Iran; 5Department of Dermatology, Allergy Division, Medical University of Graz, Austria
Corresponding author: Prof. Birger Kränke, E-mail: birger.kraenke@medunigraz.at
Submission: 24.03.2019; Acceptance: 24.08.2019
DOI: 10.7241/ourd.20201.15
Cite this article: Mofarrah R, Mofarrah R, Amiri KJ, Tabar MM, Kränke B. Beta-blocker bisoprolol induced psoriasis. Our Dermatol Online. 2020;11(1):59-61.
Citation tools:
BibTex | CSV | RIS | Endnote XML
Copyright information
© Our Dermatology Online 2019. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
A number of beta-adrenoceptor blocking drugs have been reported to be upon the most common causative agents for drug-induced psoriatic lesions. Apparently this adverse reaction appears after several months of continuous therapy. In our case psoriasis eruption is associated with bisoprolol (B1-blocker) therapy in a man without previous skin lesions and history of psoriasis. The biopsy demonstrated psoriasiform dermatitis with spongiosis and parakeratosis. The pathogenic mechanisms to be discussed are the pharmacological effects on the epidermal beta-adrenergic adenylate cyclase-cyclic AMP system and on the excessive release of lysosomal enzymes.
Key words: Bisoprolol. Beta-adrenoceptor blocking drugs. Psoriasis eruption. Drug eruption. Drug- induced psoriatic
INTRODUCTION
Adverse drug reactions constitute a significant public health problem, and, therefore, identifying relevant drug interactions is a critical step for prevention. Many reports in the literature outline the more or less prominent role of drugs in initiating, triggering, or aggravating psoriasis lesions [1–4].
Since their introduction, beta-blockers have been increasingly prescribed in the treatment of cardiovascular diseases such as angina pectoris, arrhythmia, hypertension as well as non-cardiovascular indications like essential tremor, migraine headache prophylaxis, and infantile hemangioma [3–5]. Beta-blockers are classified as non-cardioselective and cardioselective, according to their capacity to interact selectively with ß1- and ß2-adrenergic receptors. Side effects are well reported for several organ systems. The integumentary system constitutes one of the rarest areas which may be affected by these agents.
Adverse cutaneous reactions induced by beta-blockers imitate different polymorphic skin disorders which are related to the wide extent of intracellular transduction pathways and signals they influence. The reported clinical cutaneous symptoms include classical dermatoses such as psoriasiform and papulosquamous eruptions, lichenoid, eczematous, exfoliative eruptions, and hyperkeratosis of the distal extremities [6].
Extracutaneous organ manifestations associated with beta-blockers represent characteristic symptom complexes like the oculomucutaneous syndrome and the pseudolupus erythromatosus syndrome [7]. Fibrinous peritonitis may be a lethal side effect. The drug induced LE syndrome is clinically difficult to distinguish from the idiopathic SLE.
Therapy with beta-blockers may result in a de novo induced psoriasiform eruption on clinically uninvolved skin in a known case of psoriasis, aggravation of a pre-existing psoriatic tendency or in precipitation of the disease in persons without family history of psoriasis or in predisposed individuals [8]. Even cases who became resistant to conventional anti-psoriatic therapy are reported [6]. An induction period before the occurrence of clinical manifestation is characteristic, which is usually of an approximately 1 year duration, but may vary [7]. All these facts make it difficult for clinicians to comprehend the causal relation and therefore often lead to a misdiagnosis. The mechanisms by which beta-blockers might induce or exacerbate psoriasis are largely unknown, but there may be two major pathogenetic mechanisms causing the cutaneous reactions: heterogeneous immunological stimulation and the pharmacological effect of adrenergic beta-blockers on the adenylate cyclase AMP system in epidermal cells.
In this context we would like to present a case report highlighting the importance of considering beta-blockers as potential cause of polymorphic cutaneous eruptions.
CASE REPORT
We present a case of a 57- year male farmer referred to the dermatology clinic, Medical University of Graz, Austria, with some patches of eczematous dermatitis over the trunk (Fig. 1). These eruptions were thought to be induced by the anti-gout medication allopurinol, a substance that inhibits the action of xanthine oxidase, which he has been using uneventfully for several years. The skin biopsy showed spongiotic dermatitis. Therefore allopurinol therapy was withdrawn immediately. The patient improved well and the rush subsided. But after 20 days he was hospitalized again due to a sub-erythrodermatic eruption with partial symmetrical papulo-squamous lesions on his face and trunk. In addition, dystrophic hyperkeratosis of the palms, nails and soles were accompanied by severe itching.
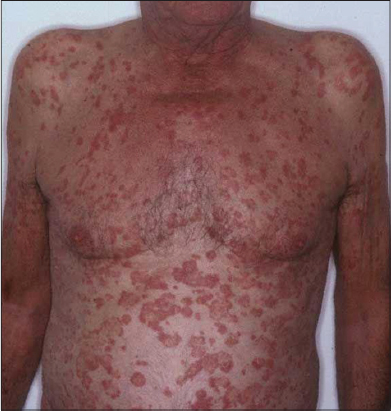 |
Figure 1: Psoriasisform rash with well-demarcated erythematous scaly plaques in the trunk 2 years after beginning of therapy with bisoprolol. |
A diagnosis of sub-erythrodermatic psoriasis was made, and we raised the question of a beta-blocker induced psoriasiform eruption. This suspicion was indorsed by the patient’s history, his clinical presentation and the results of the histological examination. The biopsy specimen of the right thigh demonstrated psoriasiform dermatitis with spongiosis and parakeratosis. His history revealed an approximately two year period consumption of Rivacor® (bisoprolol, ß1 selective) due to arterial hypertension before the onset of cutaneous symptoms. No previous skin lesions and history of psoriasis could be elicited. Laboratory results showed high IgE levels, 21% eosinophils in the differential blood count, positive antinuclear antibodies test and LE cells. The beta-blocker medication was discontinued, and an ACE Inhibitor was prescribed. Topical bethametason therapy was added, and as a result the cutaneous symptoms were ameliorated. The amount of total ANA titer decreased (1:160). At the follow-up control after 4 weeks we saw a partial remission of the suberythrodermatic skin condition and the hyperkeratotic lesions. Rechallenge with bisoprolol was refused by the patient and thus not pursued.
DISCUSSION
Many cases of cutaneous, mucous and dermal appendage side effects of non-selective (alprenolol, carvedilol, nadolol, oxprenolol, pindolol, propranolol) [8] as well as selective beta-blockers (acebutolol, atenolol, cetamolol, metoprolol, practolol) have been published.
Because psoriasis is a very complex disease and its activity is often unpredictable, clinical studies on adverse drug effects in psoriasis have been difficult to conduct [1]. Heng et al. [9] have shown distinct clinical and histopathological features of beta-blocker induced psoriasiform eruptions which differentiate this syndrome from psoriasis. The psoriasiform lesions induced by beta-blockers are characterized as (generalized) erythematous papulosquamous plaques with less erythema and scaling than seen in psoriasis. The trunk and extremities are symmetrically affected without involving the face. The histopathology findings reveal an intradermal and predominantly perivascular mixture of mononuclear cells, neutrophils and eosinophils.
There are two major theories which explain the underlying pathomechanism; Lymphocytes, macrophages and neutrophils expose membrane beta-adrenergic receptors, depressed cAMP levels through blocking these receptors via beta-blockers are associated with enhanced proliferation, motility and activity of lymphocytes, neutrophils and cells of the macrophage Langerhans cell series [9–12]. Released lysosomal enzymes by these cells are responsible for the presence of basal keratinocyte herniations and the related hyperproliferation and psoriasiform eruptions Epidermal cells are mainly ß2 adrenergic receptor carriers. Located on the membrane, adenylate cyclase converts ATP into cAMP. It is generally accepted that cyclic AMP plays a key role in keratinocyte proliferation and differentiation. Decreased intracellular AMP levels lead to a higher proliferation and reduced cell differentiation, whereas AMP reduction results in a decrease of mitotic and metabolic activity [13].
Thus blocking the beta-receptors in the skin leads to a decrease in intracellular calcium and intra-epidermal cyclic AMP. This decrease, in turn, results in an increased epidermal cell proliferation. The reason why beta-blockers of the newer generation (ß1 selective) affect ß2 receptors in epidermal cells is related to cross- reactions between the different beta-blocker subtypes.
Other theories related to beta-blocker induced cutaneous side effects include impaired lymphocyte transformation and delayed hypersensitivity Type (IV hypersensitivity). Immunoreactions are thought to be associated with psoriasiform and lichenoid lesions which histologically show the pattern of a lichenoid drug eruption. This hypothesis is supported by in vivo (positive patch test) and in vitro tests [7].
Beta-blocker induced eruptions can mimic a wide range of cutaneous lesions thus delaying diagnosis. Although the clinical presentation resembles psoriasiform skin lesions microscopic imaging shows in most of the cases a monomorph histology with acanthosis, focal hyperkeratosis, mixed dermal infiltration and lichenoid drug reaction secondary to beta-blockers [14].
Latency periods for beta-blockers vary from several days to 12 months (48 weeks) on average. They are shorter in cases of de novo pustular psoriasis and in the exacerbation of pre-existing psoriasis. The reasons for these variations remain unknown and imply the influence of individual, genetic, and racial background [2]. An induction period of two years as seen in our case was previously reported in the literature [7]. Medication history should always be considered in terms of unexplainable skin eruptions, and an adequate substitution of the offending beta-blocker agent should be initiated. After withdrawal of the beta-blockers the psoriasiform eruptions usually clear up in nearly 50 % of the cases [7].
The exacerbation of a pre-existing psoriasis after bisoprolol initiation was previously reported [15]. With our patient we mention the first case of a de-novo induced psoriasifrom eruption due to bisoprolol in a patient with no history of psoriasis.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Rongioletti F, Fiorucci C, Parodi A. Psoriasis induced or aggravated by drugs. J Rheumatol Suppl. 2009;83:59-61.
2. Basavaraj KH, Ashok NM, Rashmi R, Praveen TK. The role of drugs in the induction and/or exacerbation of psoriasis. Int J Dermatol. 2010;49:1351-61.
3. Wu S, Han J, Li WQ, Qureshi AA. Hypertension, antihypertensive medication use, and risk of psoriasis. JAMA Dermatol. 2014;150:957-63.
4. Baggio R, Le Treut C, Darrieux L, Vareliette A, Safa G. Psoriasiform diaper rash possibly induced by oral propranolol in an 18-Month-old girl with infantile hemangioma. Case Rep Dermatol. 2016;8:369–73.
5. Menezes MD, McCarter R, Greene EA, Bauman NM. Status of propranolol for treatment of infantile hemangioma and description of a randomized clinical trial. Ann Otol Rhinol Laryngol. 2011;120:686–95.
6. Arnold T, Schaarschmidt ML, Herr R, Fischer JE, Goerdt S, Peitsch WK. Drug survival rates and reasons for drug discontinuation in psoriasis. J Dtsch Dermatol. 2016;14:1089-99.
7. Hödl S. [Side effects of beta receptor blockers on the skin. Review and personal observations]. Hautarzt. 1985;36:549-57.
8. Bilewicz-Stebel M, Miziolek B, Bergler-Czop B, Stańkowska A. Drug-induced subacute cutaneous lupus erythematosus caused by a topical beta blocker-timolol. Acta Dermatovenerol Croat. 2018;26:44-7.
9. Heng MC, Heng MK. Beta-adrenoceptor antagonist-induced psoriasiform eruption. Clinical and pathogenetic aspects. Int J Dermatol. 1988;27:619-27.
10. Milave-Puretic V, Mance M, Ceovic R, Lipozencic J. Drug induced psoriasis. Acta Dermatovenerol Croat. 2011;19:39-42.
11. Lowes MA, Suarez-Farinas M, Krueger JG. Palmoplantar pustular psoriasis following initiation of a beta-blocker:disease control with low-dose methotrexate. Cutis. 2014;94:153-5.
12. Balak DM, Hajdarbegovic E. Drug-induced psoriasis:clinical perspectives. Psoriasis (Auckl). 2017;7:87-94.
13. Harris RR, Mackenzie IC. The effects of alpha and beta adrenergic agonists and cyclic adenosine 3′:5′-monophosphate on epidermal metabolism. J Invest Dermatol. 1981;77:337-40.
14. Onnis G, Dreyfus I, Mazereeuw-Hautier J. Factors associated with delayed referral for infantile hemangioma necessitating propranolol. J Eur Acad Dermatol Venereol. 2018;32:1584-8.
15. Waqar S, Sarkar P. Exacerbation of psoriasis with beta blocker therapy. CMAJ. 2009;181:1-2.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-5145-792X http://orcid.org/0000-0002-5145-792X |


Comments are closed.