Botryomycosis or metastatic tuberculous abscess – A clinical dilemma to a dermatologist?
Parul Chojer , B.B. Mahajan, Jyoti Budhwar, Lovleen Kaur
, B.B. Mahajan, Jyoti Budhwar, Lovleen Kaur
Department of Dermatology, Venereology and Leprology, Government Medical College, Amritsar, India
Corresponding author: Dr. Parul Chojer, E-mail: parul199019@gmail.com
Submission: 31.01.2019; Acceptance: 26.04.2019
DOI: 10.7241/ourd.20194.12
Cite this article: Chojer P, Mahajan BB, Budhwar J, Kaur L. Botryomycosis or metastatic tuberculous abscess – A clinical dilemma to a dermatologist? Our Dermatol Online. 2019;10(4):364-366.
Citation tools:
BibTex | CSV | RIS | refer/BiblX | Endnote XML
Copyright information
© Our Dermatology Online 2019. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Cutaneous botryomycosis is a chronic focal infection characterised by a granulomatous inflammatory response to bacterial pathogens such as Staphylococcus aureus and occasionally Pseudomonas, Escherichia coli, Proteus, Streptococcus, etc. Early diagnosis and treatment with specific antibiotics alongwith surgical debridement is recommended. Cutaneous metastatic tuberculous abscess and scrofuloderma also presents as subcutaneous swellings and multiple discharging sinuses. A twenty two year old female patient presented with multiple erythematous subcutaneous lesions over lower back, buttocks and bilateral inguinal region, most of which were discharging purulent material since two years. This case is being reported because of the clinical dilemma it poses to the dermatologists.
Key words: Botryomycosis, Tuberculosis, Amoxy-clavulanic acid, Linezolid
INTRODUCTION
Cutaneous tuberculosis comprises only a small proportion of all cases of tuberculosis. Mycobacterium tuberculosis can cause skin infection by direct inoculation into the skin, by hematogenous spread from internal lesion and by direct contact with tuberculosis in an underlying deeper structure [1]. Pyodermas due to staphylococcus usually present as acute inflammatory skin changes such as impetigo and furunculosis. However, immunodeficiency may change the presentation due to staphylococcus skin infection towards chronic granulomatous condition. Botryomycosis (or bacterial pseudomycosis or pyoderma vegetans) is a rare chronic bacterial granulomatous disease that usually involves skin and rarely viscera [2]. Most common cause is Staphylococcus aureus and occasionally Pseudomonas spp., Escherichia coli, Proteus spp., and Streptococcus spp [3]. Metastatic tuberculous abscess and scrofuloderma has a similar presentation in the form of subcutaneous swellings as in Botryomycosis and posing a clinical dilemma to a dermatologist and hence, being reported.
CASE REPORT
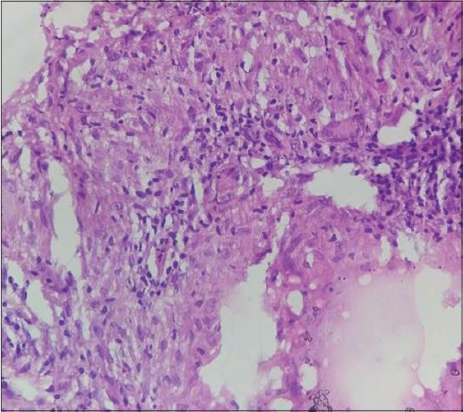
A twenty two year old female patient presented with history of multiple erythematous skin lesions over lower back, buttocks and bilateral inguinal region, most of which were discharging purulent material since two years. She had history of fall over ground 2 years back for which she was treated at a local hospital and got temporary relief only as multiple nodules with discharging sinuses kept on appearing. Local cutaneous examination revealed multiple erythematousnodules over lower back, right buttock and bilateral inguinal region.Some of the lesions were discharging purulent material. On palpation, lesions were indurated, tender and not fixed to underlying structures with purulent discharge on manipulation. Some old healed lesions in the form of multiple hyperpigmented patches of size 1×3 cms to 5×2 cms with well- ill defined irregular margins were present over lower part of back (Fig. 1). Some of the lesions in the form of keloidal scar tracts were present over inguinal region (Fig. 2). Hair, nail and mucosae were normal. All vital signs were normal. Systemic examination did not reveal anything significant to the case. Routine investigations were within normal limits, except ESR, which was 70 (raised). On pus culture and sensitivity, the isolate grew as a golden yellow pigmented, opaque colony that was diagnosed as Staphylococcus aureus by Gram Staining. ZiehlNelssen staining, CBNAAT, KOH preparation and fungal culture were negative. Histopathology report was equivocal and on the basis of pus and culture sensitivity, patient was started on tablet amoxicillin- clavulanic acid 625 mg three times a day and linezolid 600 mg twice daily with only marginal improvement for a period of 4 weeks. Biopsy was repeated and it revealedorthohyperkeratosis, marked acanthosis with irregular elongation of rete ridges. In the dermis, inflammatory infiltrate composed of lymphocytes, plasma cells and histiocytes is seen. Non caseating granulomas was also seen, suggestive of cutaneous tuberculosis and patient was started on antitubercular therapy (Fig. 3). All the lesions improved and have started healing after 2 months of intensive antitubercular therapy (Fig. 4). Patient is still on regular follow up with remarkable improvement and healed up lesions showing keloidal scarring.
DISCUSSION
Cutaneous tuberculosis (CTB) continues to be one of the most difficult diagnoses to make because of the wide variations in its clinical appearance, histopathology, immunology and treatment response [4,5]. The incidence of this disease has increased in the 21st century, due to a high incidence of HIV infection and multidrug-resistant pulmonary tuberculosis [6]. Metastatic tuberculous abscess or tubercular gumma results from disseminated hematogenous spread of mycobacteria and presents as single or multiple dermal subcutaneous nodules which may become fluctuant or break down to form ulcers. Underlying tissue is not involved which is usually involved in scrofuloderma. Although the usual site of involvement is extremities. In our case, trunk was primarily involved [1]. Tuberculin test is usually positive but in our case it was negative and no other tests, namely, ZiehlNelssen, CBNAAT staining was positive. Systemic examination and radiological examination did not reveal any systemic involvement in our case. The differential diagnosis of metastatic tuberculous abscess include botryomycosis, actinomycosis and eumycetoma. Botryomycosis present in two forms: cutaneous and visceral. Chronic form presents as chronic, suppurative and granulomatous skin lesions similar to our patient. It may be preceded by trauma [3]. Most cases present with nodules, abscesses and sinuses with purulent discharge [7,8]. Visceral form is usually with pulmonary involvement [9], which is associated with cystic fibrosis and reaches skin forming sinuses and irregular masses. Rarely, polymicrobial etiology is considered. Most common cause is Staphylococcus aureus and occasionally Pseudomonas spp., Proteus spp., and Streptococcus spp., E.Coli, Actinobacilluslignieressi, etc. It is also associated with immunosuppression [10]. Thus, metastatic tuberculous abscess may be misdiagnosed as cutaneous botryomycosis posing a clinical dilemma to a dermatologist.
CONCLUSION
Metastatic tuberculous abscess and scrofuloderma has a similar presentation in the form of subcutaneous swellings as in Botryomycosis and posing a clinical dilemma to a dermatologist.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Mycobacterial Infections. In:Victoria M. Yates, Stephen l. Walker. Rook’s textbook of Dermatology. 8th edition;2010;p.27.1-27.47.
2. Bacterial infections. In:James WD, Berger TG, Elston DM, editors. Andrews’diseases of the skin:Clinical dermatology, 11th ed. Elsevier;2011. 250.
3. John K, Gunasekaran K, Kodiatte TA, Iyyadurai R. Cutaneous botryomycosis of the foot:A case report and review of literature. Indian J Med Microbiol. 2018;36:447-9
4. Bravo FG, Gotuzzo E. Cutaneous tuberculosis. Clin Dermatol. 2007;25:173–80.
5. Ghosh S, Aggarwal K, Jain VK, Chauduri S, Ghosh E, Arshdeep. Tuberculosis verrucosa cutis presenting as diffuse plantar keratoderma:an unusual sight. Indian J Dermatol. 2014;59:80–1.
6. Barbagallo J, Tager P, Ingleton R, Hirsch RJ, Weinberg JM. Cutaneous tuberculosis. Diagnosis and Treatment. Am J Clin Dermatol. 2002;3:319–28.
7. B Devi, B Behera, ML Dash, MR Puhan, SS Pattnaik, S Patro. Botryomycosis. Indian J Dermatol. 2013;58:406.
8. Chintaginjala A, Harshavardhan K, Senthil Kumar AL. Cutaneous Botryomycosis:A Rare Case Report. Indian J Dermatol. 2016;61:126.
9. Motswaledi H, Makama JZ, Khan N. Botryomycosis:A case report. SA J Radiol. 2006;10:14–5.
10. Rit K, Saha R, Chakrabarty P. A Case Report of Staphylococcus aureus Induced Cutaneous Botryomycosis in a Patient with Acquired Immune Deficiency Syndrome. MAMC J Med Sci. 2015;1:108-10.
Notes
Source of Support: Nil
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|





Comments are closed.