|
Get Citation
|
|
|
Chang P, Meaux T. Trichomycosis axillaris. Our Dermatol Online. 2018;9(1):35-37. |
|
|
Download citation file:
|
Trichomycosis axillaris
1Department of Dermatology, Hospital General de Enfermedades IGSS and Hospital Ángeles, Guatemala; 2Student, Hospital General de Enfermedades IGSS and Hospital Ángeles, Guatemala,
Corresponding author: Dr. Patricia Chang, E-mail: pchang2622@gmail.com
Submission: 30.01.2017; Acceptance: 25.05.2017
DOI: 10.7241/ourd.20181.10
ABSTRACT
We report a cases of trichomicosys axillaris in a male patient 48 years old that was an incidental finding on dermatological examination for another dermatological consultation.
Key words: Trichomycosis axillaris; Corynebacterium flavescent; Axillar hair; Whitish concretions
CASE REPORT
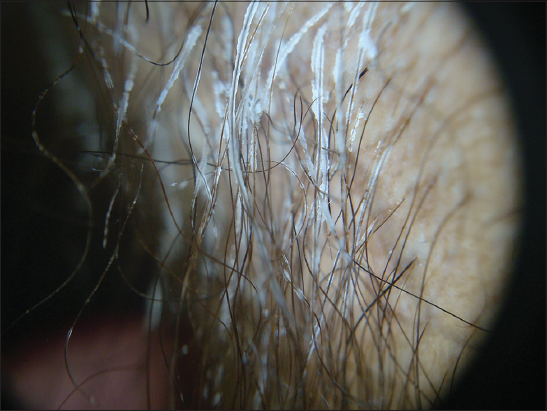
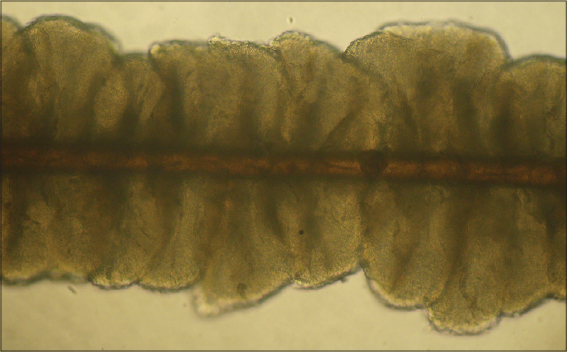
We present a case of a male patient working as a carpenter 48 years old, who visited our emergency room for a contact dermatitis affecting the hands bilaterally. During the physical examination, he was found to have a trichopathy localized at the axillary hair, consisting of multiple whitish concretions and nodules (Figs. 1a and 1b). Dermoscopy showed multiple nodular concretions around the hair Figs. 2a and 2b), direct examination showed concretions around the hairs (Fig. 3), with microscopy, pods seen around the hairs (Fig. 4).
The remainder of the examination was within normal limits. The patient did not have any change in the color of his axillar sweat.
This trichopathy was an incidental finding on dermatological examination for another reason, and the patient reports that he had not noticed it previously. Patient reports an unremarkable personal and family history.
With this clinical data, the diagnosis of trichomycosis axillaris was made. It was recommended to shave the axillary hair and apply 1% fusidic acid three times daily for 8 days.
DISCUSION
Trichomycosis axillaris (TMA), also known as Trichobacteriosis, is a superficial infection of the axillary hair shaft caused by the aerobic gram positive bacterium Corynebacterium flavescens, formerly named Corynebacterium tenuis. This bacterium is present in nature as both bacillus and diphtheroid, and mostly causes disease in humid, tropical climates [1–3]. The mechanism of infection involves physical contact between the bacteria and the hair shaft. C. flavescens is able to adhere to the surface of the shaft due to a substance produced by both the organism and the apocrine glands of the human host [2]. Obesity, poor hygiene, and disturbances in apocrine sweat production contribute to the occurrence of this disease process [1,4]. Patients may have concurrent pitted keratolysis and/or erythrasma (all three present in 13% of patients with pitted keratolysis according to one study) [5,6]. In fact, when a patient has all three of these diseases, it is given a special name, “the Corynebacterium triad” [3]. An adult male with axillary hyperhidrosis and bromhydrosis, stained clothes, and roughened texture of axillary hairs, are the typical historical findings that aid physiciansin the diagnosis of trichomycosis axillaris [2,4,7]. This disease can produce three types of hair discoloration: yellow, which is most common (98% of cases), red, and black [3]. Physical examination demonstrates 1-2mm discrete nodules attached to axillary hair shafts. While the axillae are involved in roughly 97% of cases, it is possible for other areas of the body to also be affected. Those reported include the pubic, inter-gluteal and eyebrow regions [2,5]. Differential diagnosis includes erythrasma, tinea, white and black piedra, pediculosis, and Trichosporonaselie [2,7]. Microscopic examination with 10% KOH shows pods or concretions, which are actually masses of bacteria surrounding the hair shaft. When direct pressure is applied to these structures, microscopic visualization of 5-1µmcoccoids and diptheroids adherent to hair shafts eliminates a fungal etiology, while the absence of coral red fluorescence under woods lamp rules out erythrasma [1–3]. Woods lamp is also useful in determining which parts of the body are affected, as infected hair shafts fluoresce under low-intensity UV light due to the presence of bacterial concretions [2]. Dermoscopy also aids in the diagnosis of trichobacteriosis, revealing waxy and yellowish adherent nodules and concretions along the hair shaft [4]. Culture of Corynebacterium is difficult and not necessary for diagnosis. Treatment options for TMA include shaving the hair in the affected area, topical anti-bacterial or anti-fungal preparations, and other topical treatments containing 3% sulfur, 2% formalin, 1% fusidic acid, mercuric chloride, or 2% sodium hypochlorite [2,5]. Preventative measures include regular and continued use of topical ammonium chloride solution or drying powders to counter perspiration [7]. Regarding topical antibiotic preparations, one study showed no difference in efficacy between benzoyl peroxide and erythromycin. The study also showed that shaving did not lead to a quicker cure, and average time to complete cure was roughly 3 weeks [8].
REFERENCES
1. Ma DL, Vano-Galvan S. Trichomycosis axillaris. N Engl J Med. 2013;369:1735.
2. Bonifaz A, Vaquez-Gonzalez D, Fierro L, Araiza J, Ponce RM. Trichomycosis (Trichobacteriosis):Clinical and Microbiological Experience with 56 Cases. Int J Trichology. 2013;5:12–6.
3. Bonifaz A. Micología Médica Basica. Mc Graw Hill México. 2013:171-3.
4. Salim G, Zahra MF. Trichobacteriosis:contribution of dermoscopy. Dermatol Online J. 2014;16;20.
5. James WD, Berger TG, Elston DM. Diseases of the Skin Appendages in:Andrews’Diseases of the Skin:Clinical Dermatology. Saunders Elsevier. 2006:763.
6. Kim MG, Kim JA, Rho NK, Kim BJ, Kim WS, Lee DY, et al. A Clinical analysis of 133 cases of pitted keratolysis. Korean J Dermatol. 2006;44:1165-70.
Notes
Source of Support: Nil
Conflict of Interest: None declared.




Comments are closed.