Bacterial dermohypodermitis at the Thies Regional Hospital, Senegal (West Africa): A retrospective study of 425 cases
Pauline Dioussé1, Maodo Ndiaye2, Haby Dione1, Mariama Bammo3, Ousmane Sow1, Fatou Seck1, Ndiaga Gueye3, Assane Diop2, Boubacar Ahy Diatta2, Mame Thierno Dieng2, Bernard Marcel Diop1, Mamadou Mourtalla Ka1
1Faculty of Health Sciences, University of Thies, Thiès, Senegal; 2Department of Dermatology, Cheikh Anta Diop University, Dakar, Senegal; 3Department of Dermatology, Thies Regional Hospital, Thiès, Senegal
Corresponding author: Dr. Pauline Dioussé, E-mail: paudiousse@yahoo.fr
Submission: 09.02.2017; Acceptance: 02.03.2017
DOI: 10.7241/ourd.20173.70
ABSTRACT
Introduction: Bacterial dermohypodermitis (BDH) risk factors identified in the literature on series of national hospitals are: obesity, diabetes, lymphedema, venous insufficiency. We report a series in a regional hospital.
Material and Methods: This was a retrospective study, conducted over a period of 9 years from 1 January 2007 to 31 December 2015. All data of patients received for BDH including. Socio-demographic, clinical, para-clinical and evolution variables was collected and analyzed using the Statistical Package for Social Sciences (SPSS) Version 20 software.
Results: Of the 35,692 patients received in consultation, 425 had BDH (1.19%) and 33.7% were hospitalized. The mean age was 40.6 ± 17.02 years. The age groups 16-59 years were 81% of the cases. There was a female predominance (74%) with a sex ratio H/F = 0.35. The average time to consultation was 8.1 ± 9.5 days for BDH. The lesion were located in the lower limbs in 90.4% cases. The average hospital stay was 8.6 ± 4.7 days. Artificial skin bleaching (p = 0.003), non-steroidal anti-inflammatory drugs (p = 0.001), high blood pressure (p = 0.013), obesity (p = 0.028) were the risk factors identified in our series.
Conclusions: Our series shows that the emergence of BDH also affects regional hospitals in West Africa. It also confirms that artificial skin bleaching, Non-steroidal anti-inflammatory drug, high blood pressure, obesity are aggravating factors.
Key words: Bacterial dermohypodermitis, Erysipelas, Necrotizing fasciitis, Risk factors, Senegal
INTRODUCTION
Bacterial dermohypodermitis (BDH) is dermal and hypodermis bacterial infections, often streptococcal for most of the times and has two anatomo-clinical forms: non-necrotizing and necrotizing BDH [1–3]. Their incidence rate is estimated at 9 cases per 100000 inhabitants per year in Europe [4]. In black Africa, numerous series of national hospitals have reported cases [1,5–7]. Obesity, diabetes, artificial skin bleaching, lymphedema and HIV infection are the identified risk factors. In Senegal, studies on BDH were carried out in some hospitals around the capital [8–10]. We report a series of 425 cases observed at the regional hospital of Thies in order to study their epidemiological, clinical and evolutional characteristics.
MATERIALS AND METHODS
This was a retrospective descriptive and analytical study carried out in the dermatology department of the regional hospital of Thies over a period of 9 years (1 January 2007 to 31 December 2015). Patient records received for BDH from both outpatient and inpatient care were included. Records of patients with confounding conditions were not included: phlebitis, myositis, lymphangitis, phlegmon, gangrene.
The data were collected on a standard form comprising the following variables:
- Sociodemographic: age, gender, date of consultation, profession
- Risk factors: self-medication, phytotherapy, artificial skin bleaching, use of non-steroidal anti-inflammatory, chronic Ulcer, high blood pressure, lymphedema, eczema, pregnancy, diabetes, cardiopathy, obesity, varicose veins, venous insufficiency, fractures, burns, ethylic, smoking.
- Clinical aspects: consultating period, traumatic wounds, topography and the clinical forms. Clinical aspects classified according to the French Society of Dermatology (SFD) [2] in two anatomical-clinical forms:
- Acute non-necrotizing dermo-hypodermitis: Inflammatory, localized, infectious, skin and subcutaneous tissue damage without necrosis of superficial fascia;
- Acute necrotizing dermo-hypodermitis: localized inflammatory disease of infectious origin of the skin and subcutaneous cellular tissue with necrosis not reaching deep into the superficial aponeurosis; the involvement of the latter becomes fasciitis.
- Para clinical aspects: retroviral serology, venous doppler echocardiography.
- The treatment, the progression and duration of hospitalization were noted.
The data was compiled and analyzed using Statistical Package for Social Sciences (SPSS) Version 20. The proportions of the qualitative variables were compared using the Chi-square, and quantitative with respect to group variables by the ANOVA test or the Kruskal-Wallis depending on the heterogeneity of the variance and distribution of data. The threshold of significance was p < 0.05.
Ethics Statement
This study was performed on records of patients.
RESULTS
Of a total of 35,692 patients received in consultation, 425 had BDH (1.19%). Of the 804 hospitalized dermatoses, 271 were BDH (33.7%). Most of them were received in consultation between June (13%), July (16%) and August (15%). The mean age was 40.6 ± 17.02 years with extremes between 2 and 96 years. The age groups 16-59 years represented 81% of cases, patients ≥ 60 years made up 14% of cases while children ≤ 15 years represented 5%. There was a female predominance (74%) with a sex ratio H/F = 0.35. 42.8% of the patients were unemployed.
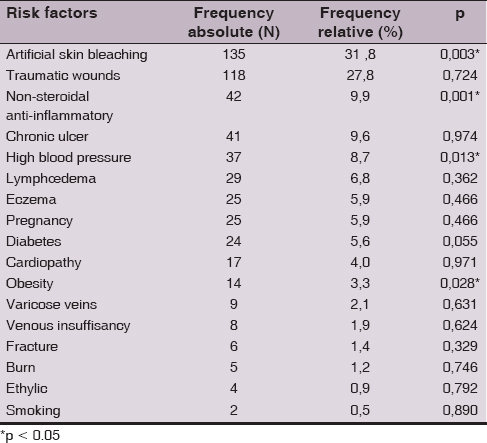
The mean time to consultation was 8.1 ± 9.5 days for non-necrotizing BDH and 12.3 ± 12.7 days for necrotizing fasciitis. 7.6% of patients self-medicated themselves, 4% with phytotherapy and 0.5% with non-steroidal anti-inflammatory drugs. Among the risk factors (Table 1), 31.8% practiced of artificial skin bleaching (p = 0.003) (Fig. 1) and all pregnant women. Of these, 10 were in the second quarter and 8 were in the third. Other risk factors were non-steroidal anti-inflammatory drugs (p = 0.001), arterial hypertension (p = 0.013), obesity (p = 0.028). BD was localized to the lower limbs in 90.4% of the cases and 7.10% to upper limbs. The entry point was identified in 52.5% of the cases. According to the clinical forms, necrotizing BDH was represented by 89.6% of cases, necrosis by 5.7% of cases and necrotizing fasciitis in 4.7% of cases.
Retroviral serology was negative in all patients. Venous doppler echocardiography was performed in 18.9% of cases and found venous insufficiency in 2.4% of cases, venous thrombosis in 1.2% of cases. Of the 65.2% of patients were hospitalized. Forty-four of them (10.4%) underwent necrosis (Fig. 2) and all benefited from a skin graft (Fig. 3). Evolution was favorable in 89% of patients. The mean hospital stay was 8.6 ± 4.7 days in the non-necrotizing BDH and 63.5 ± 4.7 days in the necrotizing fasciitis.
DISCUSSION
We reported a series of 425 cases of BDH observed at the Thies regional hospital/Senegal (West Africa). This series shows that the emergence of this infectious pathology is limited only in the great capitals of black Africa. Indeed the classical factors identified, which are found in our series, are also listed all over Africa.
The frequency of BDH in our study was 1.19%. It varied with other studies [9,11]. It was lower than that of Niamba et al (1.47%) in Burkina Faso [12], Cissé et al in Guinea [5]. However, the BDH was the first reason for hospitalization in our series. The mean age of BDH in our study was similar to that found in the Pitché et al study [13]. One reason for this age range was the young, active age group with a higher risk of trauma. In our series, BDH peaks were found in summer (June, July, and August). This period coincided with the rainy season, rural work and rising temperatures in Senegal. The micro-traumas caused during this work could constitute ports of entry of the germs. Similar results were reported by Pitché et al [13]. According to these authors, this frequency peak could be explained by: the phenomenon of maceration and microbial growth due to heat; stasis edema of stasis favored by the strong heat; the high frequency of micro traumas to the lower limbs, which are frequent during this period act as germ entry points. The female predominance observed in our series is probably due to the fact that most women practiced artificial skin bleaching and that the latter constituted a risk factor for the occurrence of BDH. The use of skin bleaching cosmetic products in African women is a well-documented fact of the society [5,9,14]. It is common among young women. In the study by Mahé et al, the 20-39 years age range represents 63.5% [15]. The products used are based on corticosteroids and/or hydroquinone; can contribute to the onset of high blood pressure and obesity. In Kebe et al, 52% of women used corticosteroids. The latter result in local immunosuppression and fragilization of the skin. In our series, all pregnant patients practiced artificial skin bleaching and 18 of them after the first trimester of pregnancy. Pregnancy as a risk factor was noted in 5.9%. It was, by itself, a factor in reducing immunity. Kebe found that 49.4% of the patients were engaged in artificial skin bleaching to be beautiful on the day of their ceremony [14]. The most serious forms of artificial skin bleaching were encountered during the period preceding special events. In Senegal, ceremonies such as baptisms constitute an important event for public recognition. Women accentuate their efforts to be as white as possible on the day of the event. Topography of the lesions favored the lower limbs as the most frequent sites, probably due to the high proportion of other risk factors with podal localization: inter-toe intertrigo, leg ulcers, lymphedema and venous insufficiency. The non-necrotizing forms predominant in our series, are forms with a fairly long average time [8] days between onset of the disease and diagnosis. This delay would probably be due to the low socio-economic status of most of these patients, the use of herbal medicine, and self-medication with other drugs such as non-steroidal anti-inflammatory drugs. Observations have reported the occurrence of BDH in non-steroidal anti-inflammatory drugs during chickenpox in children [16].
Retroviral serology was negative in all our patients due to the low prevalence of HIV infection in Senegal which is 0.7% and 0.4% in the region of Thies. The 44 patients underwent necrosectomy and all had a skin graft. Due to lack of plastic surgeon in the area, the puncture graft was performed by dermatologists at the patient’s bed after local anesthesia of the sampling area. This surgery reduced patients’ hospital stay by an average of 63.5 ± 4.7 days in the necrotizing fasciitis. The morbidity of these conditions is very high, both in the literature and in our series, lengths of hospitalization are long, on average more than 1 month and can exceed 100 days in the necrotizing fasciitis due to multiple initial interventions and secondary reconstructions [8].
CONCLUSION
Our series shows that the emergence of BDH also affects regional hospitals in Africa. It also confirms that artificial depigmentation, non-steroidal anti-inflammatory drugs, high blood pressure, obesity are aggravating factors.
REFERENCES
1. Saka B, Kombaté K, Mouhari-Toure A, Akakpo S, Boukari T, Pitché P, et al. Bacterial Dermohypodermitis and Necrotizing Fasciitis: 104 Observations in Togo. Med Trop. 2011;71:162-4.
2. Society of Infectious Pathology of French Language and French Society of Dermatology. Consensus conference: erysipelas and necrotizing fasciitis: management. Med Mal Infect. 2000;30:245-6.
3. Diédhiou D, Ndour-Mbaye NM, Sarr A. Erysipelas of the lower limbs in patients with diabetes in 54 cases in Internal Medicine. Med Afr Noire. 2012;56:83-7.
4. Genné D, Laure Blum C, Menzinger S. Erysipelas-clinical manifestations and management. Rev Med Switzerland. 2013;9:1812-5.
5. Cissé M, Keïta M, Touré A, Camara A, Machet L, Lorette G. Bacterial Dermohypodermitis: a retrospective monocentric study of 244 cases observed in Guinea. Ann Dermatol Venereol. 2007;134:748-51.
6. Binan Y, Adom H, Konan M, Kacou E, Dosso S, Toutou T. Facteurs favorisant l’apparition des érysipèles chez les séniors. Facilitating factors as erysipelas in the erderly. Rev Int Sc Méd. 2013;2:54-6.
7. Fustes-Morales A, Gutierrez-Castrellon P, Duran-Mckinster C, Orozco-Covarrubias L, Tamayo-Sanchez L, Ruiz-Maldonado R. Necrotizing fasciitis: reports of 39 pediatric cases. Arch Dermatol. 2012;138:893-9.
8. Ecra EJ, Kouassi YI, Gbery IP, Sangaré A, Kourouma S, Kouassi A, et al. Comparative Study of Necrotizing Bacterial Dermohypodermitis or Necrotizing Fasciitis Depending on the HIV Serostatus in Abidjan (Cote d’Ivoire). J Clin Exp Dermatol Res. 2014;6:234.
9. Dieng MT, Diop Ng, Niang So. Bacterial dermohypodermitis and artificial skin bleaching: About 60 cases observed in Senegal. Nouvell Dermatol. 2001;:630-2.
10. Diatta BA, Ly F, Diallo M, Ndiaye N, Diop A, Niang SO, et al. Risk factors of bacterial dermohypodermitis in Senegal: multicenter case-control study. Ann Dermatol Venereol. 2013;140:36.
11. Sarr A, Ly F, Manga M. Dermatoses associated with diabetes in Senegalese patients (prospective study of 140 patients). Rev CAMES. 2012;13:128-32.
12. Niamba P, Traore A, Traore-Barro F. Epidemiological, clinical and evolutionary aspects of erysipelas at the Yalgado Ouédraogo university hospital center in Ouagadougou (Burkina Faso). Med Afr Noire. 2006;53:257-60.
13. Pitché P, Diatta B, Faye O, Diané BF, Sangaré A, Niamba P, et al. Risk factors associated with leg erysipelas (cellulitis) in sub-Saharan Africa. A multicentre case-control study. Ann Dermatol Venereol. 2015;142:633-8.
14. Kebe M, Yahya S, Lo B, Ball M. Etude des complications de la dépigmentation artificielle à Nouakchott, Mauritanie. Mali Medical. 2015; tome III, N°1: 38-40.
15. Mahé A, Ly F, Gounongbé A. La dépigmentation cosmétique à Dakar (Sénégal): facteurs socio-économiques et motivations individuelles. Sciences Sociales et Santé. 2004;22:5-33.
16. Kologlu MB, Yildiz RV, Alper B, Ya?murlu A, Ciftçi E, Gökçora IH, et al. Nicrotizing fasciitis in children: diagnostic and therapeutic aspects. J Pediatr Surg. 2007;42:1892-97.
Notes
Source of Support: Nil
Conflict of Interest: None declared.



Comments are closed.