|
Get Citation
|
|
|
Eftekhari H, Rana R, Arash D, Maryam MH, Sara NR. Lupus vulgaris of the auricle. Our Dermatol Online. 2017;8(1):31-33. |
|
|
Download citation file:
|
Lupus vulgaris of the auricle
Hojat Eftekhari1, Rafiei Rana1, Daryakar Arash2, Mohammad Hosseini Maryam1, Naji Rad Sara3
1Skin Research Center, Guilan University of Medical Sciences, Razi Hospital, Sardare Jangal St.Rasht, Iran; 2Gastrointestinal and Liver Research Center, Guilan University of Medical Sciences, Razi Hospital, Sardare Jangal St.Rasht, Iran; 3epartment of Internal Medicine, Nassau University Medical Center, 2201 Hempstead turnpike, East Meadow, NY, 11554, USA
Corresponding author: Rana Rafiei, MD., E-mail: rafieirana@yahoo.com
Submission: 15.05.2016; Acceptance: 23.07.2016
DOI: 10.7241/ourd.20171.07
ABSTRACT
Nowadays despite decrease in the tuberculosis (TB) incidence around the world with standard anti tubercular treatment, atypical forms of TB is increasing due to extensive use of immunosuppressive therapy for autoimmune diseases and increasing prevalence of HIV infection, so early diagnosis of pulmonary and extra pulmonary TB in these patients is very important. Cutaneous TB could be a great imitator and confused with other granulomatous lesions. It has different morphological patterns. Lupus vulgaris (LV) is the most common type of cutaneous TB which usually involves head and neck. We present herein a case of LV in auricular region without apparent systemic involvement.
Key words: Tuberculosis; Lupus vulgaris; Auricle
INTRODUCTION
Approximately 1%-2% of all cases of TB are cutaneous TB [1]. Considerable morphological variation in clinical presentation of cutaneous TB, difficulty in mycobacterium culture and even negative results using polymerase chain reaction (PCR) in paraffin-embedded specimens could result in delayed diagnosis of cutaneous TB [2]. Lupus vulgaris is the most common type of cutaneous TB often presents as an asymptomatic, slow growing plaque on the face [3]. LV could be complicated by scarring and deformity so we should consider it in any granulomatous lesions on the skin [4].
CASE REPORT
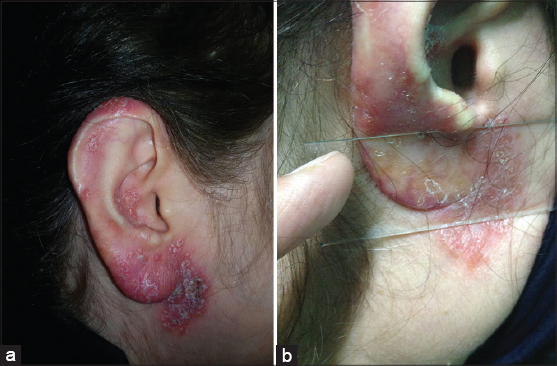
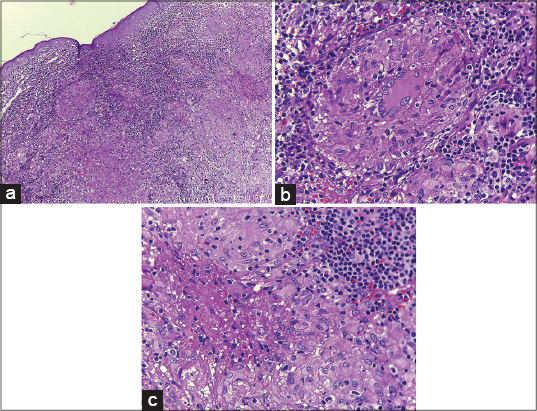
We present herein a 51-year old farmer woman with erythematous pruritic lesions over the right auricular region of one year duration. There were erythematous, scaly and infiltrated plaques on the auricle and periauricular area. The lesions initially manifested on the retro-auricular region and gradually involved whole ear and periauricular area. Diascopy revealed an “apple-jelly” color (Fig. 1a and b). Skin biopsy was taken from the ear lobe with considering sarcoidosis, lupus vulgaris, leprosy, leishmaniasis, deep mycosis and discoid lupus erythematosu as differential diagnosis. Histopathologic changes were flattened epidermis with confluent tuberculoid type granuloma in the upper and mid dermis included langhans type giant cell and small foci of fibrinoid necrosis (Figs. 2a–c). No acid fast bacillus or fungal element was identified in Ziehl-Neelsen and Periodic Acid Schiff (PAS) staining which was in favor of lupus vulgaris. Polymerase chain reaction (PCR) study in paraffin block was negative for mycobacterium tuberculosis.
In physical examination there was no lymphadenopathy, neural thickening or sensory changes. She had no weight loss, night sweats, fever, cough, and hemoptysis. She had Bacillus Calmette-Guerin (BCG) vaccination scar on her left arm but there was not any other skin lesion. Ritual ear piercing had been done in childhood but she did not remember any other trauma to the auricular region.
Past medical and drug histories were unremarkable. Family history was positive for pulmonary TB in her mother which was treated with anti-tuberculosis therapy (ATT) when our patient was a child. Her mother died of car accident a few years ago.
There were no abnormal findings in chest x ray and laboratory data Including complete blood count (CBC), basic metabolic panel (BMP), liver function test (LFT), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), angiotensin converting enzyme (ACE) level and urine analysis. The purified protein derivative (PPD) test was positive (25×20 millimeters induration with vesicle formation) after 48 hours and subsequently an edematous, erythematous, scaly plaque formed over the injection site (Fig. 3). We could not be able to rule out visceral tuberculosis in this patient so standard ATT was started.
DISCUSSION
TB is still a problem in the developed and underdeveloped countries and cutaneous TB is a small part of extra pulmonary forms [1]. The most common type of cutaneous TB is named lupus vulgaris which indicates destructive behavior of the disease (in Latin lupus means wolf). It usually affects females more than males and could be presented as plaque, nodule, ulcer, mutilating and vegetative lesions [3,5]. LV occurs on the face, ear, neck and less common extremities and trunk [6]. LV often develops by hematogenous spread of mycobacterium (endogenous type) especially in case of facial involvement but also lymphatic, contagious spread and acquired exogenous inoculation after BCG vaccination, body piercing or tattooing have been reported [6–8]. It may be confused with other granulomatous lesions or even masquerading hemangioma, psoriasis, lichen simplex, discoid lupus erythematosus and alopecia [4]. Due to high degree immunity against mycobacterium in LV patients, bacilli are rarely seen on acid fast staining and cultures are frequently negative [6,9]. Positive PPD test is observed in a subject who has a history of BCG vaccination or previous mycobacterial infection so this test is not reliable for diagnosis of LV but in our patient a LV-like plaque developed on the site of PPD test.
Absolute criteria for cutaneous TB are positive culture of mycobacterium tuberculosis or DNA identification by PCR [5]. Negative PCR result in paraffin block does not rule out cutaneous TB because formalin fixation has been found to decrease the PCR amplification signal, so a fresh specimen for PCR has been recommended [2]. In this case PCR study was done on formalin fixed tissue.
Association between LV and clinically undiagnosed visceral tuberculosis is not uncommon [10], so we advised our patient to receive standard ATT for visceral TB and the treatment is still ongoing. Delayed diagnosis of cutaneous TB results in deformity, contracture, lymphedema and increasing rate of squamous or basal cell carcinoma, hence early diagnosis is very important.
In conclusion, we should keep in mind cutaneous TB as a differential diagnosis for any chronic granulomatous skin lesions to prevent these complications and in some cases where PCR and culture are not helpful, a therapeutic trial of ATT has been recommended [4].
REFERENCES
1. Bravo F, Gotuzzo E, Cutaneous tuberculosisClin Dermatol 2007; 25: 173-80.
2. Okazaki M, Sakurai A, Lupus vulgaris of the earlobeJ Ann Plast Surg 1997; 39: 643-6.
3. Senol M, Ozcan A, Mizrak B, Turgut AC, Karaca S, Kocer H, A case of lupus vulgaris with unusual locationJ Dermatol 2003; 30: 566-9.
4. Saritha M, Parveen BA, Anandan V, Priyavathani MR, Tharini KG, Atypical forms of lupus vulgaris – a case seriesInt J Dermatol 2009; 48: 150-3.
5. Thomas S, Suhas S, Pai KM, Raghu AR, Lupus vulgaris-report of a case with facial involvementBr Dent J 2005; 198: 135-7.
6. Wozniacka A, Schwartz RA, Sysa-Jedrzejowska A, Borun M, Arkuszewska C, Lupus vulgaris:report of two casesInt J Dermatol 2005; 44: 299-301.
7. Khandpur S, Reddy BS, Lupus vulgaris:unusual presentations over the faceJ Eur Acad Dermatol Venereol 2003; 17: 706-10.
8. Ghorpade A, Tattoo inoculation lupus vulgaris in two Indian ladiesJ Eur Acad Dermatol Venereol 2006; 20: 476-7.
9. Hofman V, Selva E, Landraud L, Sicard D, Venissac N, Castillo L, Value of PCR amplification from formalin-fixed paraffin-embedded tissues in the diagnosis of Mycobacterium tuberculosis infectionAnn Pathol 2003; 23: 206-15.
10. Marcoval J, Servitje O, Moreno A, Jucgla A, Peyri J, Lupus vulgaris. Clinical, histopathologic, and bacteriologic study of 10 casesJ Am Acad Dermatol 1992; 26: 404-7.
Notes
Source of Support: Nil
Conflict of Interest: None declared.

Comments are closed.