|
Get Citation
|
|
|
Brzeziński P, Senanayake MP, Karunaratne I, Chiriac A. Dermotology eponyms – sign – Lexicon (R): Part 1. Our Dermatology Online. 2017;8(1):114-120. |
|
|
Download citation file:
|
Dermatology eponyms – sign – Lexicon(R): Part 1
Piotr Brzeziński1, Manouri P. Senanayake2, Irantha Karunaratne2, Anca Chiriac3
1Department of Cosmetology, Institute of Biology and Environmental Protection, Pomeranian Academy, Slupsk, Poland; 2Department of Pediatrics, Faculty of Medicine, University of Colombo, Kynsey Road, Colombo 008, Sri Lanka; 3Department of Dermatology, Nicolina Medical Center, Iasi, Romania
Corresponding author: Piotr Brzezinski, MD, PhD., E-mail: brzezoo77@yahoo.com
Submission: 25.03.2016; Acceptance: 09.09.2016
DOI: 10.7241/ourd.20171.34
ABSTRACT
Eponyms are used almost daily in the clinical practice of dermatology. And yet, information about the person behind the eponyms is difficult to find. Indeed, who is? What is this person’s nationality? Is this person alive or dead? How can one find the paper in which this person first described the disease? Eponyms are used to describe not only disease, but also clinical signs, surgical procedures, staining techniques, pharmacological formulations, and even pieces of equipment. In this article we present the symptoms starting with (R) and other. The symptoms and their synonyms, and those who have described this symptom or phenomenon.
Key words: Eponyms; Skin diseases; Sign; Phenomenon
Rabbit Fever Sign
Tularemia infection [1].
Raccoon Sign
- The periorbital bruising associated with anterior basilar skull fracture or fracture of the nose and neuroblastoma. Sometimes associated with the reservoir phenomenon of cerebrospinal fluid in the sinus cavity [2]. Also known as “panda eyes”.
- The most common cutaneous manifestation of neonatal lupus erythematosus is erythematous, slightly scaly eruption on the face and periorbital skin (raccoon sign/owl-eye/eye mask).
- Periorbital hemorrhage due to laxity of blood vessels seen after proctoscopic examination (postproctoscopic periorbital Purpura) in patients having systemic amyloidosis is also called as Raccoon eyes/sign/panda sign.
Rag-sorters’s Sign
- Malignant pustule in rag-sorters [3].
- A febrile disease with cough and headache, seen in rag-sorters, and due probably to a bacillus.
Rain Rot Sign
Pustular desquamative dermatitis, caused by the zoonotic fungal Dermatophilus congolensis. Found in horses, cattle, sheep, and other mammals wordwide [4]. Also called Rain Scald sign and Dew Poisonning sign.
Rain Sclad Sign
Also called Rain Rot sign.
Rash-extinction Sign
Schultz-Charlton reaction phenomenon [5]. The specific blanching of a scarlatinal rash at the site of intracutaneous injection of scarlatina antiserum.
In 1918, Schultz and Charlton1 first reported that the intracutaneous injection of from 0.5 to 1 cc. of normal or scarlet fever convalescent serum would blanch the rash of scarlet fever at the site of injection. They also showed that the blanching substance was present in serum taken after the fourteenth day of scarlet fever, but that serum taken earlier in the disease did not have blanching power. Plain horse serum or diphtheria antitoxin failed to blanch the rash. Schultz and Charlton also made injections of a dilute solution of epinephrine hydrochloride intracutaneously, and found that the rash blanched within a few minutes. This blanching lasted five or six hours. In contrast, the reaction produced by scarlet fever convalescent serum appeared only after five or six hours and lasted several days. Schultz and Charlton expressed the belief that human serum contained some vasoconstricting factor which counteracted the vasodilating effect.
Rasin’s Sign
The pigmentation, usually brownish, occurring on the lid margins in many cases of hyperparathyroidism [6]. Also known as Jellinek‘s sign.
Stefan Jellinek
Austrian physician, 1871-1968 (Fig. 1). He studied medicine at the University of Vienna from 1892 to 1898. From December 1898 to April 1899 Senator’s assistant at the clinic in Berlin. In the years 1900-1903 the aspirant in the third clinic in Vienna, from 1903 sekundariusz in the Department of Dermatology. In December 1908 his habilitation in internal medicine. Since 1910 assistant at the Institute Elektropatologicznym. May 14, 1929 elektropatologii was an associate professor at the University of Vienna. In 1938, because of his Jewish origin had lost his job, then emigrated to the UK. He practiced at Queen’s College [6].
Raspberry Sign
Contagious raspberry like nodules beginning with minute red spots, then after seven days form yellow papules, then the raspberry crust, sometimes with edema of the limbs and eyelids. Also called by the Carib word yaws and the French framboise or frambesia. Believed to be same as button-scuvry of Ireland [7].
Raynaud’s Sign
Raynaud phenomenon, a vasospastic disorder, is characterized by sensitivity to cold temperatures, triggering the release of vasoconstrictors, including catecholamines, endothelin-1, or 5-hydroxytryptamine (Fig. 2). Clinically, vasospasm or vasoconstriction may be associated with a change in the color of the fingers or toes, starting with one or several digits and spreading symmetrically to all fingers or toes (A cold pale condition of the fingers and toes alternating with heat and redness). Attacks usually end with a sudden reflow of blood to the area, creating a reactive hyperemia. Criteria for primary Raynaud phenomenon (RP) are symmetrical attacks without necrosis, ulceration, or gangrene and no evidence of secondary causes. Typical onset of primary RP occurs in the early to middle teens as well as sometimes after the fourth decade of life. Symptoms may be mild. In contrast, criteria for secondary RP are associated with severe episodic attacks, usually asymmetrical or with ulcerations. Patients also may have other manifestations of connective tissue disease (eg, arthritis, systemic sclerosis). An early sign of asymmetric gangrene or Raynaud’s disease. Also known as acro-asphyxia or Dead-finger sign and sphaceloderma [8,9].
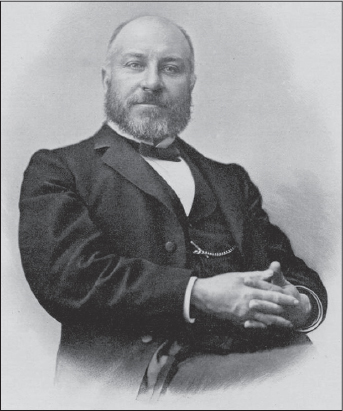
Auguste Gabriel Maurice Raynaud
French physician, (1834-1881) (Fig. 3). He discovered Raynaud’s Disease, a rare vasospastic disorder which contracts blood vessels in extremities and is the “R” in the CREST syndrome acronym, in the late 19th century.
Maurice Raynaud was the son of a university professor. He commenced his medical studies at the University of Paris with the help of his uncle, the well known Paris physician Ange-Gabriel-Maxime Vernois (1809–1877), and obtained his medical doctorate in 1862. He thus became one of the select few who have achieved eponymous fame with their doctoral dissertation, in his case: De l’asphyxie locale et de la gangrène symétrique des extrémités.
Raynaud never received a senior position at any of the Paris hospitals, but became Médecine des hôpitaux (received hospital privileges) in 1865. At various times, he was attached to the hospitals of Hôtel Dieu (1866), Sainte Périne (1868), Saint-Antoine (1872), Lariboisière (1872) et La Charité (1880), among others. In 1866 he became an agrégé with the works Sur les hyperhémies non phlegmasiques and De la revulsion, which established him as a professor of medical pathology.
He was made an officer of the Légion d’honneur in 1871 and elected to the Académie de Médecine in 1879, and lectured with great success at the university as well as the Lariboisière and Charité hospitals.
Although Raynaud always wanted to hold the chair of medical history at the University of Paris, he died on 29 June 1881, in his prime, before achieving that goal, shortly before the international medical congress in London that year. At the London congress, Raynaud’s paper, “Scepticism in Medicine, Past and Present”, was read by one of his colleagues.
He was also a busy writer. His book Sur la salive d’un enfant mort de la rage was the result of research done with Louis Pasteur and Odilon Marc Lannelongue.
Recklinghausen’s Sign
Multiple neurofibromata (Fig. 4) [10].
Friedrich Daniel Von Recklinghausen
German pathologist, 1833-1910 (Fig. 5). He began his medical studies in Bonn in 1852, continued them in Würzburg, and completed his doctorate in Berlin in 1855. Subsequently, he studied pathology with Rudolf Virchow, after which he traveled to Vienna, Rome, and Paris for further study. He returned to Berlin in 1858 and served as an assistant in Virchow’s Institute for Pathology until 1864. In Königsberg, he was briefly appointed as Professor Ordinarius—without having gone through the usual academic steps of Docent and Professor Extraordinary—until six months later, when he went to Würzburg until 1872. He was then appointed Professor at the new university in Strassburg. He became Rector of the university in 1877, and remained there until his death in 1910.
Recklinghausen was well known for many important contributions, including early descriptions of hemochromatosis, bone lesions in hyperparathyroidism, and, of course, a number of eponymous conditions: von Recklinghausen’s Disease, von Recklinghausen’s tumor (adenoleiomyofibroma on wall of the fallopian tube or posterior uterine wall), and von Recklinghausen’s canals (lymphatic canaliculi). He developed a silver nitrate stain to allow visualization of cell structures.
While von Recklinghausen was not the first to recognize spina bifida (the first description was apparently in 1641 by Fulpius, who coined the term), he was one of the first to provide such a complete description. We reproduce here a brief abridgement of his classic article, “Untersuchungen über die Spina bifida,” published in 1886 [11,12].
Relapsing Sign
A zoonotic louseborne Borrelia disease, causing a relapsing fever every three to five days. Also calleed relapsing fever disease [13].
Remak’s Sign
A double sensation caused by pricking with a needle. A sign of tabes dorsalis [14].
Ernst Julius Remak
German neurologist, 1849-1911 (Fig. 6). He was the son of famed neurologist Robert Remak.
He received his education at the Universities of Breslau, Berlin, Würzburg, Strasbourg and Heidelberg, and obtained the degree of M.D. in 1870. Afterwards he took part in the Franco-Prussian War of 1870-71. After serving as assistant in the department for nervous diseases at the Charité Hospital, Berlin from 1873 to 1875, he established himself as a neuropathologist in the German capital, where he became privat-docent in 1877, and professor in 1893. With Edward Flatau, he published an important work on neuritis and polyneuritis.
His name is associated with the eponymous “Remak reflex”, which is plantar flexion of the first three toes and sometimes the foot with extension of the knee, induced by stroking of the upper anterior surface of the thigh. This reflex takes place when the conducting paths in the spinal cord are interrupted [15].
Remak has contributed more than 50 essays to the professional journals, and is the author of:”Grundriss der Elektrodiagnostik und Elektrotherapie für Praktische Aerzte”, Vienna, 1895. “Neuritis und Polyneuritis,” in Nothnagel‘s, “Handbuch der Speziellen Pathologic und Therapie”, ib. 1900.
Renbök Phenomenon
In 1991, Happle et al. coined the term “Renbök” phenomenon to describe the opposite of the Koebner phenomenon, designating the withdrawal of a lesion with the appearance of another one. It was originally described in alopecia areata (AA) patients experiencing hair growth in psoriatic lesions. Although psoriasis can often co-exist with AA, reports on psoriasis-induced Renbök phenomenon in AA have been exceedingly sparse, and did not demonstrate the interchanging nature of these two disorders [16].
Rendu’s Sign
Telangiectases around the mouth found in the malabsorption Osler-Weber-Rendu disease [17,18].
Henri Jules Louis Marie Rendu
French physician, 1844-1902 (Fig. 7). In 1865, on the advice of his father, Rendu registered in the School of Medicine in Paris. First in his class, he became externe in 1867, and in 1868 interne at the Hôpital Saint-Antoine in the department of Jules Guyot, also working under Adolphe-Marie Gubler, Ernest Henri Besnier, Henri Louis Roger, and Pierre Charles Édouard Potain, with whom he became closely associated.
In 1870, after the declaration of the Franco-Prussian war, he was appointed as surgeon to the army. He did not accept the principle of evacuation of patients upon whom he had operated, taking a great risk, and asked the help of locals to keep them with him. Coming back to Paris, he held a junior appointment at the Hôpital Saint-Louis where he became involved in dermatology, then spent some time in the care of infants and children. In 1873 he was awarded the Médaille d’Or of internship and spent a year at the Hôpital Necker in the department of professor Pierre Charles Édouard Potain, one of France’s leading clinicians. In 1874 he produced his thesis on the “Paralyses related to tuberculous meningitis in children” for which he received the Médaille d’Argent. At this time he also started a private practice.
In 1877 Rendu received the degree of hospital physician – médecin des hôpitaux – and then married Marie Labric, whose father was a physician at the Hôpital des Enfants. In 1878 he finally achieved professeur agrégé with a thesis on “Comparative study of chronic nephritis”.
He then began his career in the Hôpital Tenon, and in 1885 moved to a senior post as Head of the Department of Medicine at the Hôpital Necker, where he spent the remainder of his career.
Rendu published more than 100 medical articles and his academic activities were rewarded in 1878 by elevation to the status of professor agrégé of the faculty of medicine at the University of Paris. In 1897 he received the ultimate accolade of election to membership of Academy of Medicine. He had a large private practice, and even though he was offered the chair of pathology after the death of Victor Charles Hanot he preferred to remain an active clinician [18].
He spent his spare time travelling throughout France seeking specimens for the botanical collection which had been started by his grandfather, and which he made one of the finest collections of plants in France. He was also a great lover of the belle arts.
Rendu published many of his articles in Bulletin de la Société anatomique de Paris and was its editor 1873-1874. He was a contributor to Dictionnaire enyclopédique des sciences médicales.
Reverse Namaskar Sign
Namaskar’ is the typical Indian way of greeting people, where the forearms are folded in front of the chest and the palms are closely approximated together. In patients with hyperextensible joints as seen in Ehler Danlos syndrome, they are able to fold their forearms at the back and oppose their palms to say “Namaskar,” demonstrating the hyper extensible joints [19].
Rhagades Sign
White linear scars which radiate from the corners of the mouth. a sign of congenital syphilis [20].
Rhodesian Sleeping Sign (Africa)
Zoonotic trypanosomiasis [21].
Rhodius’s Sign
The sweetness of sweat afetr the ingestion of honey [22].
Apollonius of Rhodes
Was a Greek epic poet and scholar of the Library of Alexandria (First half of 3rd century BCE) (Fig. 8). He was the author of a celebrated epic entitled the Argonautica which described the journey of the Argonauts in their quest for the Golden Fleece. The key episodes of the myth were sourced from older poets such as Hesiod and Pindar [23].
“Apollonius Rhodius. Argonautica. Translated by Seaton, R. C. Loeb Classical Library Volume 001. London, William Heinemann Ltd, 1912.”
Riga-Fede Sign
Cachectic aphthae (Fig. 9). It is a benign and uncommon mucosal disorder, characterized by an ulceration of the tongue, often caused by repetitive traumatic injuries due to backward and forward movements of the tongue over the mandibular anterior incisors. Also called as Riga’s disease or Riga-Fede disease [24].
Antonio Riga
Italian physician, 1834-1918 (Fig. 10). The young Antonio Riga after finishing his studies in medicine at the University of Naples, he joined the army, reaching the rank of Major.
Back in Sant’Elia Fiumerapido was very active in public and professional life, in fact quickly became known for his scientific studies led him to the discovery of a rash illness of childhood that is called “Riga Disease”.
Later he wrote remarkable works on scientific topics including “Epidemics of malaria fever in 1879”.
Very thick was another work written from Riga, but not scientific, but sociological inherent to the condition of the society of his time: “Memoria intorno al brigantaggio nel territorio di S’Elia e i suoi dintorni”. He was ruling with the painter Enrico Risi, the Workers’ Association of Sant’Elia.
In 1889 he did his utmost for the affixing of a commemorative plaque in memory of the martyr Angelo Santilli died in Naples during the riots of 1848. Major Doctor Antonio Riga after a very active life and satisfying, died aged 84. Today he is entitled to the square adjacent to the City Hall Sant’Elia. [25].
Francesco Fede
Italian pediatrician, 1832-1913 (Fig. 11). Francesco Fede studied medicine in Napoli and then worked at the physiological institute under Giuseppe Albini (1860-1885), while also teaching embryology. A large number of his works stems from this time. Besides his normal employment he was also physician to the Nosocomia degli incurabili and taught medical pathologie and clinics. He then changed to paediatrics and in 1892 became professor of this discipline in Napoli.

Fede’s works on anaemia splenica infantilis, nephritis, Parrot’s disease, rachitis, etc. are fundamental. In 1893 he founded the journal La Pediatria, which was to gain a leading role in Italian paediatrics [26].
REFERENCES
1. Su TY, Shie SS, Chia JH, Huang CT, Case Report of Low Virulence Francisella tularensis Presented as Severe Bacteremic PneumoniaMedicine (Baltimore) 2016; 95: e3390-
2. Kandavar S, Varghese N, Rao M, Shetty S, Curious case of raccoon eye under general anaesthesiaIndian J Anaesth 2016; 60: 442-3.
3. Chellini E, Martino G, Grillo A, Fedi A, Martini A, Indiani L, Malignant mesotheliomas in textile rag sortersAnn Occup Hyg 2015; 59: 547-53.
4. Beylot C, Bioulac P, [Pustular psoriasis in infants and Leiner-Moussous desquamative erythroderma]Nouv Presse Med 1973; 2: 1000-
5. Calder RM, Allergic Shock following a Schultz-Charlton TestBr Med J 1941; 2: 198-9.
6. Brzezinski P, Chiriac A, Munsey C, Sinjab AT, Dermatology Eponyms – sign – Lexicon (J)Our Dermatol Online 2013; 4: 399-402.
7. Morton RS, The button scurvy of ireland:postcript of the mssvd meeting in Dublin, May 29 and 30 1964Br J Vener Dis 1964; 40: 271-2.
8. Leroux MB, Lashak C, Evolution of video capillaroscopy for 10 years in a patient with RaynaudOur Dermatol Online 2014; 5: 374-7.
9. Ajili F, Mansour HB, Ghedira H, Zriba S, Metoui L, Gharsallah I, Digital ischemia due to Systemic Sclerosis associated to Essential Thrombocythemia:A case reportOur Dermatol Online 2013; 4: 508-10.
10. Radek M, Tomasik B, Wojdyn M, Snopkowska-Wiaderna D, Błaszczyk M, Radek A, Neurofibromatosis type 2 (NF 2) or schwannomatosis?–Case report study and diagnostic criteriaNeurol Neurochir Pol 2016; 50: 219-25.
11. Brand RA, Biographical sketch:Friedrich Daniel von Recklinghausen, MD (1833-1910)Clin Orthop Relat Res 2011; 469: 1225-6.
12. Al Aboud K, Al Aboud D, Eponyms in the dermatolopathology literature linked to the neural tissuesOur Dermatol Online 2013; 4: 395-8.
13. Seilmaier M, Guggemos W, Wieser A, Fingerle V, Balzer L, Fenzl T, Hoch M, von Both U, Schmidt HU, Wendtner CM, Strobel E, [Louse-borne-relapsing-fever in refugees from the Horn of Africa;a case series of 25 patients]Dtsch Med Wochenschr 2016; 141: e133-42.
14. Pearce JM, The Argyll Robertson pupilJ Neurol Neurosurg Psychiatry 2004; 75: 345-
15. Holdorff B, Winau R, Geschichte der Neurologie in Berlin. Walter de Gruyter 2001; Berlin/New York:
16. Ovcharenko Y, Serbina I, Zlotogorski A, Ramot Y, Renbök phenomenon in an alopecia areata patient with psoriasisInt J Trichology 2013; 5: 194-5.
17. Brzezinski P, Dermatology Eponyms – phenomen/sign – Lexicon (E)Our Dermatol Online 2011; 2: 235-40.
18. [No authors listed]. Henri Rendu (1844-1902). Rendu-Osler-Weber diseaseJAMA 1966; 197: 583-
19. Premalatha S, Sarveswari KN, Lahiri K, Reverse-Namaskar:a new sign in Ehlers-Danlos syndrome:a family pedigree study of four generationsIndian J Dermatol 2010; 55: 86-91.
20. Khetarpal S, Kempf E, Mostow E, Congenital syphilis:early- and late-stage findings of rhagades and dental anomaliesPediatr Dermatol 2011; 28: 401-3.
21. El-Bahnasawy MM, Khater MKh, Morsy TA, African trypanosomiasis with special reference to Egyptian Trypanosoma evansi:is it a neglected zoonosis?J Egypt Soc Parasitol 2014; 44: 741-8.
22. Finlayson LH, Osborne MP, Anwyl R, Effects of acetylcholine, physostigmine, and hemicholinium-3 on spontaneous electrical activity of neurosecretory nerves in Carausius and RhodiusJ Insect Physiol 1976; 22: 1321-6.
23. http://www.theoi.com/Text/ApolloniusRhodius1.html.
24. Senanayake MP, Karunaratne I, Persistent lingual ulceration (Riga-Fede disease) in an infant with Down syndrome and natal teeth:a case reportJ Med Case Rep 2014; 8: 283-
25. Lanni A, Guida storica-turistica-commerciale di Sant’ Elia FiumerapidoEditore LAPI sas, Arti Grafiche Carmanica Marina di Minturno (LT) 1999;
26. Farnetani F, Navarra A, Farnetani I, [Biography and bibliography of Francesco Fede, the founder of Italian pediatrics]Minerva Pediatr 2011; 63: 515-26.
Notes
Source of Support: Nil
Conflict of Interest: None declared.





Comments are closed.