|
Get Citation
|
|
|
Puttaiah M, Jartarkar SR. Intense pulsed light: A promising therapy in treatment of acne vulgaris. Our Dermatol Online. 2017;8(1):6-9. |
|
|
Download citation file:
|
Intense pulsed light: A promising therapy in treatment of acne vulgaris
Manjunatha Puttaiah, Shishira R. Jartarkar
Department of Dermatology, Venereology and Leprosy, KVG Medical College and Hospital, Kurunjibhag, Sullia, India
Corresponding author: Dr. Shishira R. Jartarkar, E-mail: dr.shishira@gmail.com
Submission: 16.05.2016; Acceptance: 21.09.2016
DOI: 10.7241/ourd.20171.02
ABSTRACT
Background: Medical treatment of acne vulgaris includes a variety of topical and oral medications. Poor compliance, lack of durable remission, potential side effects are common drawbacks to these treatment. Therefore, there is a growing demand for a fast, safe and side effect free novel therapy. Light-based therapies are an attractive alternative acne therapy because they potentially offer more rapid onset and better patient compliance with a low incidence of adverse events.
Aim: To study the efficacy of intense pulsed light in treatment of acne vulgaris.
Materials and Methods: Twenty five patients with acne vulgaris were subjected to IPL. Baseline grading of acne was done. IPL was administered every 2weeks for 4 sessions. Grading was done after the end of treatment. Clinical photographs were taken for evaluation.
Results: All patients showed a reduction in the number of acne lesions after 4 sessions of IPL. No significant side effects were noted. Patients also noted an improvement in skin texture.
Conclusion: IPL showed beneficial effects in the treatment of acne.
Key words: Improvement; Acne vulgaris; Novel therapy
INTRODUCTION
Acne vulgaris is an inflammatory disease of pilosebaceous unit, characterised by seborrhoea, comedones, papules, pustules, nodules and cysts, with occasional scarring [1].
Acne is one of the most prevalent skin disorder and single most common cause for visit to a dermatologist [1]. Acne, considered as a “Stigma of Adolescence”, causes significant psychological, social and emotional distress along with a self-perception of poor health [2,3].
The pathogenesis of acne is complex and multifactorial. The major factors in the pathogenesis of acne are increased sebum production, hypercornification of pilosebaceous duct, abnormality of the microbial flora, especially ductal colonization with Propionibacterium acnes and inflammation [4].
Current therapies available for acne are mainly targeted towards multiple factors contributing to the pathogenesis of acne [5]. We are in an era where dermatologists seek to use novel treatment modalities like chemical peeling, laser and light therapies, photodynamic therapy, etc. to circumvent antibiotic resistance, reduce adverse effects seen more commonly with conventional treatment of acne like antibiotics and retinoids. Light-based therapies are an attractive alternative acne therapy because they potentially offer more rapid onset and better patient compliance with a low incidence of adverse events. However, optimal treatment methods and the relative efficacy of light-based therapies as compared to traditional therapies remain unclear. Light-based acne therapies are thought to act via reducing P. acnes proliferation or by targeting the sebaceous gland to reduce sebum production; however, other mechanisms may also exist [6]. The trials of IPL on acne vulgaris have been small and conflicting, till date. Hence, it is worthwhile to study the efficacy of IPL in acne vulgaris.
To study the efficacy of IPL in patients with acne vulgaris.
MATERIALS AND METHODS
The study was done over a period of one year from September 2014 to August 2015. The study design is a randomized open prospective study. The ethical committee clearance was obtained prior to the start of the study. Twenty five patients with mild to severe acne between the age group of 15 years and 40 years, who gave consent for the treatment were included in the study.
Age less than 15yrs and more than 40yrs, patients with extra-facial acne and acneiform eruptions, patients with keloidal tendency, patients on oral retinoids in the past 6 months, pregnant and lactating women, patients with associated systemic diseases and other facial dermatoses, patients with active herpes infection and patients who gave a history of taking treatment for acne in any form in the past one month were excluded from the study.
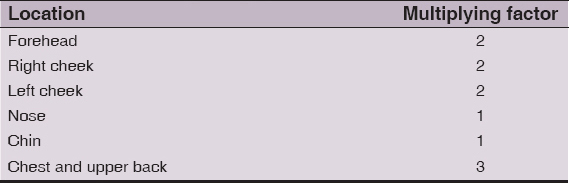
Baseline acne grading was done based on Global Acne Grading System [7] and acne classified as mild, moderate, severe and very severe (Tab. 1).
Note: Each type of lesion is given a value depending on severity. No lesions = 0, comedones = 1, papules = 2, pustules = 3 and nodules = 4. The score for each area (Local score) is calculated using the formula: Local score = Factor x Grade (0-4). The global score is the sum of local scores, and acne severity was graded using the global score. A score of 1-18 is considered mild; 19-30, moderate; 31-38, severe, and >39, very severe.
Informed consent was taken in all patients after ethical committee clearance from our institution for the study. Filter of 425nm was used. Test dose of IPL was given on forearm and maximum tolerable dose that the patient can tolerate was selected. According the skin type of the patients, fluence varied from 23-28J/cm2 and RF energy from 23-27W, with higher energy in fairer skin types and lower energy in darker skin types. Two shots of IPL per site were administered to the acne affected area at the distance of 1-2mm with a gel interface between the skin and the probe to prevent any side effects like blistering and pigmentation. IPL was administered every two weekly for 4 sessions. Post procedure instructions were advised to the patient in the form of bland moisturizers and a sunscreen with sun protection factor of 30. The degree of the improvement (total percentage reduction in the total acne score calculated by Global Acne Grading System) was noted after four sessions and photographs were taken.
0-25% reduction in score – mild improvement
26-50% reduction in score – moderate improvement
51-75% reduction in score – good improvement
>75% reduction in score – significant improvement.
OBSERVATIONS
In the present study, 15 (60%) were females and 10 (40%) were males. Of these, majority (80%) were students. In most of the patients 19 (76%), the duration of acne was between 1-4 years. The most common skin type noted was Fitzpatrick’s skin type IV [8]. 48% of the patients had severe acne, followed by very severe acne in 36% and moderate acne in 16%.
RESULTS
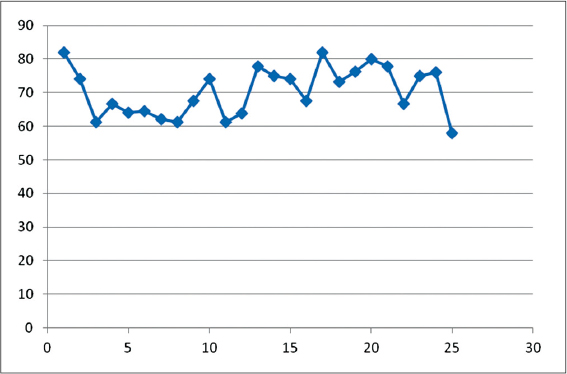
In the present study, the mean age was 21.7 yrs, with minimum age of 16yrs and maximum age of 32 yrs. The mean score of acne improved from 37.96 to 10.9 i.e., mean improvement noted was 71.3%. The maximum improvement noted was 81.9% and the minimum improvement being 57.9% (Fig. 1). Using Wilcoxon test, the improvement in acne before and after the treatment was found to be significant (p<0.005). All the patients with severe lesions, at the end of treatment had moderate lesions, patients with very severe acne, at the end of treatment had mild to moderate acne and patients with moderate acne had mild lesions. 64% of the patients had good improvement (Fig. 2) and 12% of the patients had significant improvement (Fig. 3). Moderate improvement was noted in 24% of the patients. In addition to clearance of acne, more than 70% patients also noted an improvement in skin texture, reduction in the oiliness of the skin and smoother appearance of the skin. No significant side effect was noted in most of the patients, though transient erythema and burning was noted in 40% of the patient, which spontaneously subsided over a period of few hours. One patient developed post inflammatory dyspigmentation (Fig. 4), who was treated with depigmenting creams and the dyspigmentation cleared in about a period of 1to2 months.
DISCUSSION
Intense pulsed light technology involves application of a non-coherent, non-laser broadband, filtered flash lamp source directed to the skin. Modifications of various parameters allow flexibility in treatment, which include wavelength, energy fluence, pulse duration and pulse delay. IPL acts by photodynamic therapy in treatment of acne vulgaris. P acnes produces porphyrins (protoporphyrin IX and coproporphyrin III) during their growth and proliferation in follicular units. These porphyrins have an absorption spectrum near ultraviolet and visible spectrum of light. The major absorption peak for these porphyrins is at 415nm, which is commonly known as the Soret band. A second peak corresponding to the red light is seen at 630nm. Therefore, devices that utilize either blue light or red light PDT have been developed for treatment of inflammatory acne vulgaris. After exposure to the appropriate light source, there is photo-excitation of the porphyrins. This will cause production of singlet oxygen in the organism, causing selective destruction of the organism [9].
IPL releases yellow, green and red light that is emitted in sequence of short pulses. The yellow/green light damages the bacteria that live in the skin and case acne, while red light will directly aim at the overactive sebaceous glands that causes outbreaks of pustules and nodules. This targeted heating, deep in the skin causes shrinkage of the inflamed sebaceous gland and helps prevent overproduction of excess sebum [10]. Hence, it is efficacious in nodulocystic acne also.
Elman et al. treated 19 patients with IPL and showed >50% improvement in acne lesions following twice weekly therapy for 4 weeks [11].
Paithankar et al. reported 50% reduction in acne vulgaris [12].
Dierickx reported 72% clearance rate in non-inflammatory acne and 73% improvement in inflammatory acne vulgaris lesions in 14 patients treated for five sessions two to four weeks apart [13].
Rojanamantin and Choawawanich demonstrated that IPL alone and following 5-aminolevulinic acid application can improve inflammatory facial acne [14].
We found a statistically significant decrease in the mean total score with a mean improvement of 71.3%. Our results were compatible with the results of Paithankar et al. but were different from Elman et al. This may have been due to difference in the skin type reaction to IPL therapy in Asians and Caucasians.
In the present study, we did not find any blister formation or scarring following treatment with IPL. Though, erythema and burning was noted in 40%, they were very trivial and tolerable and hence, all patients completed the study successfully. Also, the beneficial effect remained for atleast 3-4 months after the last IPL session.
CONCLUSION
Briefly, there are few previous studies demonstrating the efficacy of IPL as effective treatment modality in acne. While the previous studies excluded nodulocystic acne and have used IPL in combination with other treatment modalities, we included nodulocystic acne patients and treated successfully without encountering any significant side effects. However, further studies are necessary to define the correct role of IPL as a monotherapy in treatment of facial acne.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study.
REFERENCES
1. Garg VK, Sinha S, Sarkar R, Glycolic acid peels versus Salicylic-Mandelic acid peels in active acne vulgaris and post-acne scarring and hyperpigmentationDermatol Surg 2009; 35: 59-65.
2. Thomas DR, Psychosocial effects of acneJ Cutan Med Surg 2004; 8: suppl 43-5.
3. Al Robaee AA, Assessment of general health and quality of life in patients with acne using a validated generic questionnaireActa Dermatovenerol Alp Panonica Adrait 2009; 18: 157-64.
4. Rai R, Natarajan K, Laser and light based treatments of acneIndian J of Dermatol Venereol Leprol 2013; 79: 300-8.
5. Kim RH, Armstrong AW, Current state of acne treatment:Highlighting lasers, photodynamic therapy, and chemical peelsDermatol Online J 2011; 17: 2-
6. Ludgate M, Orringer J, Raulin C, Karsai S, Inflammatory dermatoses:AcneLaser and IPL technology in Dermatol and Aesthetic Medicine 2011; 7: 83-95.
7. Doshi A, Zaheer A, Stiller MJ, A comparison of current acne grading system and proposal of a novel systemInt J Dermatol 1997; 36: 416-8.
8. Sachdeva S, Fitzpatrick skin typing:Applications in DermatologyIndian J Dermatol Venereol Leprol 2009; 75: 93-6.
9. Kumaresan M, Srinivas CR, Efficacy of IPL in treatment of acne vulgaris:comparison of single and burst pulse mode in IPLIndian J of Dermatol 2010; 55: 370-2.
10. Torres V, Torezan L, Light based therapies for skin of color 2009; London: Springer; 249-61.
11. Elman M, Lask G, The role of pulsed light and heat energy in acne clearanceJ Cosmet Laser Ther 2004; 6: 91-5.
12. Paithankar DY, Ross EV, Saleh BA, Blair MA, Graham BS, Acne treatment with a 1450nm wavelength laser and cryogen spray coolingLasers Surg Med 2002; 31: 106-14.
13. Dierick CC, Treatment of acne vulgaris with a variable filtration IPL systemLasers Surg Med 2004; 34: 66-
14. Rojanamatin J, Choawawanich P, Treatment of inflammatory acne vulgaris with intense pulsed light and short contact of topical 5-aminolevulinic acid:a pilot studyDermatol Surg 2006; 32: 991-6.
Notes
Source of Support: Nil
Conflict of Interest: None declared.



Comments are closed.