|
Get Citation
|
|
|
Leroux MB. Herpes zoster in patients with systemic lupus erythematosus. Our Dermatol Online. 2016;7(4):494-495. |
|
|
Download citation file:
|
Herpes zoster in patients with systemic lupus erythematosus
Maria Bibiana Leroux
Centro de Referencia en Raynaud y Colagenopatías, Rosario, Argentina
Sir,
The onset of cutaneous herpes zoster (HZ) is due to a reactivation of the varicella zoster virus and it is characterized by a painful vesicular eruption following one or more dermatomes. Post herpetic neuralgia, the most common complication could develop persisting during months or even years. The HZ it is considered the most frequent viral etiology affecting patients with systemic lupus erythematosus (SLE).
Recently, Borda et al. describe the epidemiological characteristics of HZ in a Brazilian population affected with SLE. Fifty five episodes of HZ were reported in 51 patients. The onset of most of them was 5 years after the SLE diagnosis and frequently during inactive or mild activity. The majority of patients show a typical distribution and a good response to treatment. Nevertheless, complications such as secondary bacterial infection and post herpetic neuralgia could be present [1–3].
INCIDENCE
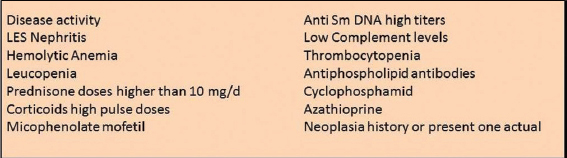
The HZ incidence is 1.2 – 4.9/1000 affected individuals annually. In SLE patients is significantly higher reaching 16-22/1000 annually. It is to be noticed that is associated with abnormal cytotoxicity mediated by T cells and aggravated by treatment with corticoids and immunosuppressant [1,2,4,5]. Infection risk factors in patients with SLE in Table I.
CLINICS
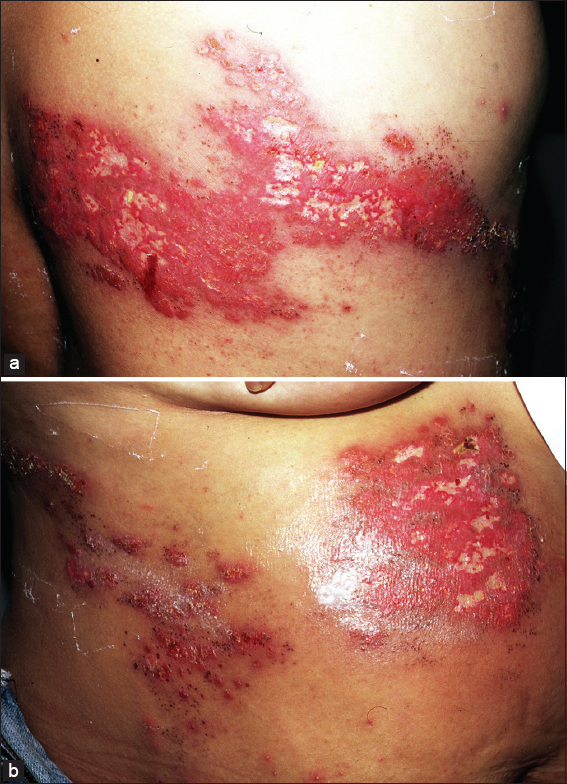
The classic HZ topography is in general unilateral affecting one dermatome, although 20% of patients could be extended to 3 contiguous dermatomes. Some authors classify this pattern as a disseminated HZ (Figs. 1a and b). A varicelliform eruption could be present in non selected patients and most frequently in immunocompromised ones. In cutaneous disseminated high risk patients visceral compromise i.e. disseminated intravascular clotting, encephalitis, hepatitis, neumonitis and pancreatitis among others could complicate [4,5].

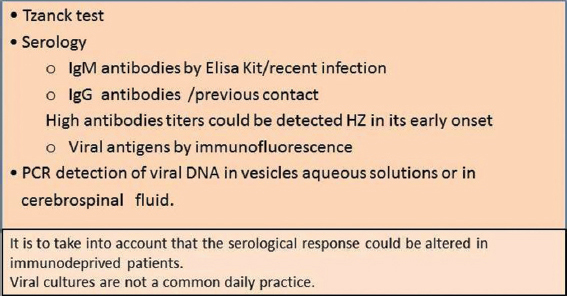
Diagnostic methodology shown in Table 2 [1–6].
TREATMENT
It is strongly recommended to initiate antiviral treatment within 72 hours of rash onset. The drugs above mentioned shall be maintained for 7-10 days and for 2 days after all the lesions are covered by a crust (Tabl. 3) [1–4].
Primary medications for acute zoster–associated pain include: analgesics, neuro active and anticonvulsant agents. Prompt treatment of acute zoster and its associated pain can prevent the development of post herpetic neuralgia. Hospital admission should be considered in these cases: severe symptoms, immunosuppression, significant bacterial super infection, disseminated herpes zoster, ophthalmic involvement or meningoencephalopathy involvement [1–4,6,7].
VACCINATION
It was introduced in 2006. It is a live attenuated vaccine recommended for 60 years old patients comporting a reactivation risk. In these individuals a diminished HZ incidence (50%) as well as post herpetic neuralgia has been observed (60%). There is no clear evidence to recommend HZ vaccine in patients with SLE. There are researchers that propose that the same rule could be applied to the general population but only in those that are not medicated with immunosupressors before of after vaccination [6–7].
CONCLUSION
Herpes zoster can be a serious problem in systemic lupus erythematosus. Its complications and its antiviral treatment are known, however, the indication of the vaccine to prevent it is not recommended in all patients.
REFERENCES
1. Chen H-H, Chen Y-M, Chen T-J, Lan J-L, Lin C-H, Chen D-Y, Risk of herpes zoster in patients with systemic lupus erythematosus: a three-year follow-up study using a nationwide population-based cohortClinics 2011; 66: 1177-82.
2. Navarra SV, Leynes MSN, Infections in systemic lupus erythematosusLupus 2010; 19: 1419-24.
3. Danza A, Ruiz-Irastorza G, Infection risk in systemic lupus erythematosus patients: susceptibility factors and preventive strategiesLupus 2013; 22: 1286-94.
4. Ruiz-Irastorza G, Olivares N, Ruiz-Arruza I, Martinez-Berriotxoa A, Egurbide MV, Aguirre C, Predictors of major infections in systemic lupus erythematosusArthritis Res Ther 2009; 11: R109-
5. Tektonidou MG, Wang H, Dasgupta A, Ward MM, Burden of Serious Infections in Adults With Systemic Lupus Erythematosus: A National Population-Based Study 1996–2011Arthritis Care Res (Hoboken) 2015; 67: 1078-85.
6. Pasoto SG, Ribeiro ACM, Bonfa E, Update on infections and vaccinations in systemic lupus erythematosus and Sjogren’s syndromeCurr Opin Rheumatol 2014; 26: 528-37.
7. Barbera C, Goldb WL, Fortin PR, Infections in the lupus patient: perspectives on preventionCurr Opin Rheumatol 2011; 23: 358-65.
Notes
Source of Support: Nil
Conflict of Interest: None declared.

Comments are closed.