Refractory lymphedema of the hand: an unusual presentation of recurrent herpes simplex virus infection
Ali Majdzadeh1,2, Mohammed I. AlJasser2,3, Sunil Kalia2
1Faculty of Medicine, University of British Columbia, Vancouver, BC Canada, 2Department of Dermatology and Skin Science, University of British Columbia and Photomedicine Institute, Vancouver Costal Health Research Institute, Vancouver, British Columbia, Canada, 3Division of Dermatology, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia
ABSTRACT
Introduction: Herpes Simplex Virus (HSV) infection of the hand resulting in lymphatic complications such as lymphangitis and lymphedema is exceedingly uncommon. Although these complications typically resolve in 21 days, they can be persistent and may not resolve even with antiviral use, thereby mimicking dyshidrotic eczema or a bacterial event and often being misdiagnosed and inappropriately treated as such. We report a case of frequently recurring HSV infection of the hand over a long period of time resulting in refractory lymphedema which did not resolve with antiviral treatment. We further endeavor to raise awareness about this highly unusual presentation of HSV infection. A comprehensive review of the literature was conducted for similar cases using PubMed and Medline.
Case Report: This is the first reported case with nearly a decade-long interval between the onset of primary HSV infection and the development of chronic lymphedema. Although valacyclovir significantly reduced the episodic aggravation of the lymphedema, it did not entirely resolve it. Similar cases of persistent lymphedema also included a long history of untreated and recurrent HSV infection of the hand, suggesting that this lymphatic outcome may be circumvented by prompt treatment with antivirals.
Conclusion: This case report not only presents a highly uncommon lymphatic manifestation and unusual timeline of exacerbation of the very common HSV infection, but also highlights the importance and benefits of early initiation of antiviral therapy and the prevention of reactivation.
Key words: Herpes simplex; Lymphedema; Communicable diseases; Viruses
INTRODUCTION
Herpes simplex virus (HSV) infection usually presents with grouped vesicles on an erythematous base. The two serotypes of this virus, HSV-1 and HSV-2, most commonly affect the labial mucosa, and the genital mucosa, respectively, in addition to the surrounding skin. While both serotypes can result in infection in different body sites, recurrent infection of the hand is more commonly caused by HSV-2 and the majority of these cases are seen in the age range of 20-40 years, with a notable preponderance of women [1]. HSV infection of the hand has a variety of symptoms and manifestations, yet lymphangitis and lymphedema of the hand are infrequently observed as a consequence [2]. Furthermore, recurrent HSV infection of the hand resulting in persistent lymphedema that is resistant to antiviral medicines is highly uncommon with only two cases reported in the literature [2,3].
We report a case of unresolved HSV-induced lymphedema of the hand which developed almost one decade following the onset of primary HSV infection and following frequent episodes of reactivation throughout this period. Such prolonged duration between the onset of primary HSV infection and presentation of chronic lymphedema has not previously been reported. We further review other comparable cases in the literature and highlight the similarities between cases of resolved and unresolved lymphedema of the hand.
CASE REPORT
A 33-year-old Caucasian female presented to our clinic with a two-and-a-half-year history of persistent swelling of the left hand and forearm. She further revealed that there was a history of painful episodic vesicular eruptions that occurred on the dorsal aspect of her left middle finger. Her first presentation of the vesicular eruption alone occurred at the age of 21. Since the development of the left hand and forearm swelling, the episodes recurred every one to two months. Each episode lasted approximately one week with an exacerbation of the swelling occurring within two days of vesicle formation. The patient has no known family history of any relevant skin disease. She denied any history of confirmed oral or genital herpes. Lymphatic massage drainage and compression bandages were previously recommended for managing the swelling, but worsened the condition.
Physical examination revealed non-pitting edema of the left hand and forearm (Fig. 1). During her subsequent clinical visit, grouped vesicles on an erythematous base involving the left middle finger were seen. No axillary or cervical lymphadenopathy was noted. Viral culture acquired from the base of a vesicle was positive for HSV-2. A prophylactic oral treatment with valacyclovir 500mg daily resulted in rapid and significant reduction of the periodic vesicular eruption and the associated transient aggravation of her persistent swelling. However, the chronic lymphedema persisted. After a 6 month follow-up, the patient reported only two recent milder episodes attributed to non-adherence to valacyclovir.
DISCUSSION
Uncomplicated HSV infection of the hand is marked by the recurrence of painful vesicles, with occasionally systemic symptoms such as malaise and fever [3]. Furthermore, lymphatic complications, such as lymphangitis and lymphadenopathy in axillary and/or epitrochlear lymph nodes, are well described and consist of proximal swelling, pain, and erythematous streaking [3,4]. More severe cases, lymphedema of the hand and/or forearm may rarely develop a few days after the onset of vesicles, and such complications can be misdiagnosed as cellulitis or dyshidrotic eczema [2,3,5]. These lymphatic events typically resolve within 21 days, but sometimes persist indefinitely [5].
Persistent lymphedema of the hand secondary to HSV infection despite antiviral treatment is exceedingly rare and has been reported only twice in the literature [2,3]. Furthermore, although there is initially involvement of lymph nodes and the spleen as early as 24 hours following infection with HSV [6], as well as immediate activation of tissue-resident CD8αα+T cells in containment of HSV-2 [7], the majority of patients with prolonged HSV-associated lymphedema of the hand did not present with any lymphadenopathy [2–4]. This clinical presentation adds further difficulty in arriving at HSV infection as a differential diagnosis. The repeated occurrence of HSV infection over long periods of time is a common element in all reported cases of unresolved and persistent lymphedema, including ours, and is likely the cause of the unresolved lymphedema. Interestingly, those who developed lymphedema which ultimately resolved in response to antiviral treatment experienced episodes of reactivation which were shorter in duration and less frequent than those with unresolved lymphedema.
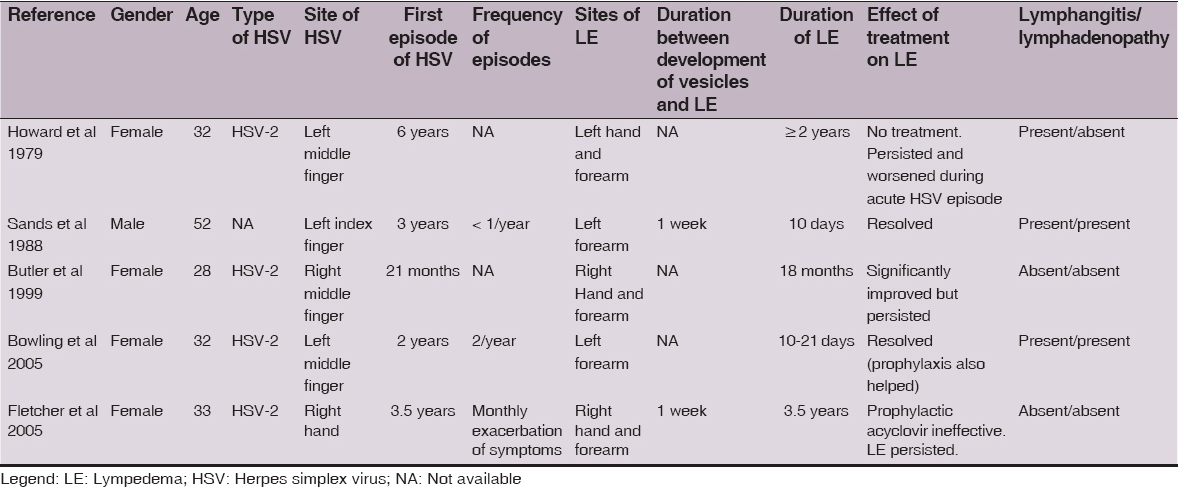
Table 1 lists all five reported cases in the literature of lymphedema secondary to HSV infection of the hand [2–5,8]. Our case and those reported in the literature demonstrate favorable outcomes with antiviral use, including suppression of the recurrence of vesicular eruptions and the episodic aggravation of the persistent lymphedema. The presentation of lymphedema of the hand as a complication of recurrent HSV infection nearly one decade following the primary infection and its persistence with antiviral treatment is of great clinical interest and didactic value. We hope that this case report will increase awareness of the abnormal manifestations and complications of HSV infection of the hand, and help clinicians avoid the unnecessary use of antibiotics, surgical manipulation, and hospitalization. The reviewed cases also strongly suggest that the prompt provision of antiviral treatment can be quite effective and may prevent the emergence of irreversible, chronic and antiviral-resistant lymphedema.
CONCLUSION
In conclusion, although uncommon, cases of episodic lymphedema in the hand with or without associated lymphangitis and lymphadenopathy should always take into account the possibility of HSV infection as a primary cause, and antiviral treatment should be promptly pursued if HSV infection is confirmed. This approach would help avoid inappropriate and unnecessary medical treatment and surgical manipulation.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Gill MJ, Arlette J, Buchan K, Herpes simplex virus infection of the hand. A profile of 79 casesAm J Med 1988; 84: 89-93.
2. Fletcher PG, Sterling JC, Recurrent herpes simplex virus type 2 infection of the hand complicated by persistent lymphoedemaAustralas J Dermatol 2005; 46: 110-3.
3. Butler DF, Malouf PJ, Batz RC, Stetson CL, Acquired lymphedema of the hand due to herpes simplex virus type 2Arch Dermatol 1999; 135: 1125-6.
4. Howard WR, Taylor JS, Steck WD, Lymphatic complications of manual herpes simplex infectionCutis 1979; 23: 580-3.
5. Sands M, Brown R, Herpes simplex lymphangitis. Two cases and a review of the literatureArch Intern Med 1988; 148: 2066-7.
6. Mueller SN, Jones CM, Smith CM, Heath WR, Carbone FR, Rapid cytotoxic T lymphocyte activation occurs in the draining lymph nodes after cutaneous herpes simplex virus infection as a result of early antigen presentation and not the presence of virusJ Exp Med 2002; 195: 651-6.
7. Zhu J, Peng T, Johnston C, Phasouk K, Kask AS, Klock A, Immune surveillance by CD8αα+ skin-resident T cells in human herpes virus infectionNature 2013; 497: 494-7.
8. Bowling JC, Saha M, Bunker CB, Herpetic whitlow: a forgotten diagnosisClin Exp Dermatol 2005; 30: 609-10.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.

Comments are closed.