A study on scar revision
Ashutosh Talwar1, Neerja Puri2
1Department of Surgery, Punjab Health Systems Corporation, Ferozepur, Punjab, India, 2Department of Dermatology and Venereology, Punjab Health Systems Corporation, Ferozepur, Punjab, India
ABSTRACT
Introduction: Scars are psychologically distressing for the patients and have an impact on the quality of life and self esteem of the patients. Scar revision is an aesthetic skill which is mastered by plastic surgeons and encroached now by dermatosurgeons. Scars on the face are aesthetically unacceptable and various techniques have been improvised for making a scar aesthetically acceptable. Various types of techniques are used for scar revision like W plasty, Z plasty and VY plasty.
Aims: To see the efficacy of various scar revision techniques including Z plasty, VY plasty and W plasty in 30 patients with disfiguring scars.
Methods: We selected twenty patients of disfiguring scars for the study. The scars from various causes including trauma and burns were included in our study. Various techniques of scar revision include Z plasty, W plasty and VY plasty were performed according to the type and site of scar.
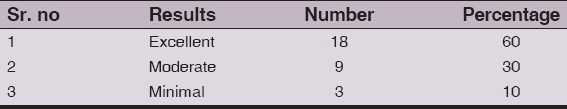
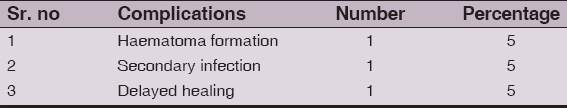
Results: Male: female was 1.5: 1. The scar revision surgery yielded excellent results with minimal complications including haematoma formation, secondary infection and delayed healing seen in 5% patients each. Regarding the efficacy of scar revision, excellent improvement was seen in 60% patients, moderate improvement was seen in 30% patients and mild improvement was seen in 10% patients.
Conclusions: Dermatologists can employ a number of surgical scar revision techniques. While some are better suited to treat specific types of scars, they can be used in combination with each other or with adjunctive therapies to achieve optimal results.
Key words:Scars; Facial; Techniques; W plasty; Z plasty; VY plasty; Revision
INTRODUCTION
Scar evaluation and revision techniques are chief among the most important skills in the facial plastic and reconstructive surgeon’s armamentarium. Often minimized in importance, these techniques depend as much on a thorough understanding of facial anatomy and aesthetics, advanced principles of wound healing, and an appreciation of the overshadowing psychological trauma as they do on thorough technical analysis and execution [1,2]. Scar revision is unique in the spectrum of facial plastic and reconstructive surgery because the initial traumatic event and its immediate treatment usually cannot be controlled. Patients who are candidates for scar revision procedures often present after significant loss of regional tissue, injury that crosses anatomically distinct facial aesthetic units, wound closure by personnel less experienced in plastic surgical technique, and poor post injury wound management [3,4]. While no scar can be removed completely, plastic surgeons can often improve the appearance of a scar, making it less obvious through the injection or application of certain steroid medications or through surgical procedures known as scar revisions. There are many variables affect the severity of scarring, including the size and depth of the wound, blood supply to the area, the thickness and color of your skin, and the direction of the scar [5,6].
A scar may cause cosmetic deformity and it may be an unpleasant reminder of a traumatic past and the patient may seek to erase its memories by erasing the scar. Finally, the patient may associate the scar with a personal failure – inability to impress a girlfriend or inability to get promoted and may be looking at treatment of the scar as a means of success in his/her endeavors. An ideal scar is thin and flat, has a good color match with the surrounding skin, is oriented along the relaxed skin tension lines (RSTLs), and does not produce any distortion of adjacent tissues. Any scar that does not fit the above definition is a suboptimal scar [7–9]. Every attempt should be made to convert a suboptimal scar into an ideal scar although it may not be always possible.
AIMS
To see the efficacy of various scar revision techniques including Z plasty, VY plasty and W plasty in 30 patients with disfiguring scars.
MATERIAL AND METHODS
We selected twenty patients of disfiguring scars for the study. The scars from various causes including trauma and burns were included in our study. Various techniques of scar revision include Z plasty, W plasty and VY plasty were performed according to the type and site of scar. Written informed consent was taken from all the patients before the study. Prior approval of hospital ethical committee was taken for the study. Pre and post operative photographs were taken of all the patients. Proper preoperative counselling of all the patients was done and the patients expectations were brought to the ground level.
Inclusion Criteria
The following patients were included in our study:
- Patients having facial scars
- Patients having realistic expectations.
Exclusion Criteria
The following patients were excluded from the study:
- Patients having history of keloid formation
- Patients having history of bleeding tendencies
- Patients on oral anticoagulants
- Patients having uncontrolled diabetes.
For assessing the efficacy of treatment, the patients were divided into three groups: Excellent results – More than 90% improvement after scar revision.
Moderate results – 75% – 90% improvement after scar revision.
Poor results – 25% – 50% improvement after scar revision.
Ethics
This study was performed on human subjects; thus, all patients were aware of the presence of the study and they were fully informed about the drug and its side-effects.
RESULTS
The data was collected, tabulated and the results were analyzed statistically using chi square test.
Results was presented in (Tables 1–3).
DISCUSSION
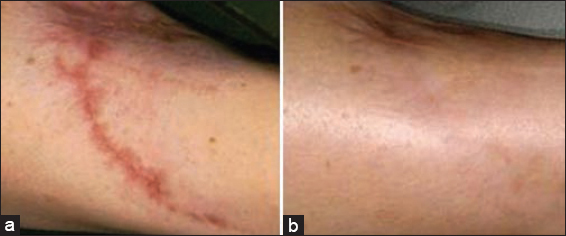
There were 12 males and 8 females and male: female was 1.5: 1. The scar revision surgery yielded excellent results with minimal complications including haematoma formation, secondary infection and delayed healing seen in 5% patients each. Regarding the efficacy of scar revision, excellent improvement (Figs. 1a and 1b) was seen in 60% patients, moderate improvement (Figs. 2a and 2b) was seen in 30% patients and mild improvement was seen in 10% patients. Poor scar is usually a result of poor technique or post-operative infection. In such cases, simple excision of the scar and resuturing using the above principles may be helpful in attaining a good appearance. Scars can be classified as -Mature scar – A light colored flat scar.
Immature scar – A red, sometimes itchy or painful, and slightly elevated scar in the process of remodelling. Many of these will mature normally over time.
Linear hypertrophic scar (e.g., due to incision) – A red, raised, sometimes itchy scar confined to the border of the original incision. These scars may increase in size rapidly for 3-6 months and then, after a static phase, begin to regress. After maturation, they may have an elevated, slightly rope like appearance with the increased width.
Widespread hypertrophic scar (e.g. due to burns): A widespread red, raised, sometimes itchy scar that remains within the borders of the original injury.
Minor keloid – A focally raised, itchy scar extending over normal tissue. This may develop up to 1 year after injury and does not regress on its own.
Major keloid – A large raised (>0.5 cm) scar, possibly painful or pruritic and extending over normal tissue. This may result from minor trauma and can continue to spread over years.
In addition to the above mentioned varieties, scars may also be atrophic, depressed, hypopigmented, hyperpigmented, or irregular with nodularity.
Scar revision is unique in the spectrum of facial plastic and reconstructive surgery because the initial traumatic event and its immediate treatment usually cannot be controlled. Patients who are candidates for scar revision procedures often present after significant loss of regional tissue, injury that crosses anatomically distinct facial aesthetic units, wound closure by personnel less experienced in plastic surgical technique, and poor post injury wound management. There are various techniques of scar revision including Z plasty, VY plasty, Wplasty and geometric broken line closure. The various techniques of scar revision are as follows:
Z PLASTY
It is a double transposition flap where the scar to be excised lies along the central limb of the Z with two peripheral limbs parallel to each other [10,11]. After transposition, the centre Z-plasty is one of the most versatile scar revision techniques available. As a transposition flap, Z-plasty allows for 2 adjacent undermined triangular flaps, constructed from the same central axis, to transpose over each other and to lie in the other’s originating bed. In essence, these 2 triangular flaps are transposed from areas of relative excess into areas of relative deficiency and eventually lie at near right angles to the original central axis. The usefulness of Z-plasty in scar revision rests in its ability to reorient a scar to lie more favorably in the direction of RSTLs; reorient the scar or anatomic landmark into a more favorable location or position; break up the length of the scar, thereby rendering it less visible; increase the scar length (ie, lengthen a contracted scar), thereby decreasing the prevailing scar contractile force and permitting better conformation to contoured surfaces and allow the surface-revised scar to run in a different angle to the deeper, more established scar, thus decreasing the tendency of the final scar to become depressed [12].
W PLASTY
It is designed to make a linear scar irregular, such that majority of the limbs lie along RSTL. While performing the W plasty, some amount of normal tissue is excised along with the scar such that the final scar is irregular, in the shape of multiple W’s lined side-by-side [13]. The W plasty consists of multiple small triangular advancement flaps on either sides of the scar such that the closure occurs in an interdigitating fashion. The advantages of W plasty are that it is easy to plan and execute and It breaks a straight scar into multiple small segments many of whom lie along the RSTL [14]. There are various disadvantages of W plasty- it may lead to a longer scar, it needs adjacent tissue laxity and sometimes regular repetitive pattern makes the scar noticeable W-plasty. The primary utility of the W-plasty (also termed the running W-plasty or zig-zag plasty) is in rendering a lengthy linear scar irregular. In addition to linear scar revision, the W-plasty is useful in the closure of semicircular incisions in which the sweeping unbroken curvilinear scar is more noticeable and under greater tension and, thus, over time more likely to become depressed or pincushioned. Note that while the W-plasty makes irregular a linear scar and spares unwanted lengthening that may arise from using small multiple Z-plasties, the final result is often readily visible because the eye easily can follow the predictable zig-zag configuration [15]. Finally, in its basic execution, this technique incorporates neither transposition nor rotation of adjacent flaps; therefore, the final scar is not elongated but only increased in the final total length.
Geometric Broken Line Closure
It is designed to convert a long linear scar into a randomly irregular scar. Interdigitating geometric lines are drawn in such a manner that triangles, rectangles, squares. and even semicircles are created on either side of the scar in a random fashion. Majority of the lines should lie along the RSTL [16]. After excision along these lines, the advancement flaps from both sides interdigitate so as to create a randomly irregular scar. Like in W plasty, ends have to be closed using 30° angulations to prevent the dog ear which may occur if higher angles are used Unfavorable facial scars result from a variety of influences, over which the reconstructive surgeon often has little initial control.
The decision regarding the location and type of incision used during any scar revision is based primarily on the concept of orienting all incisions perpendicular (as much as possible) to the direction of maximal underlying tension. Incisions made perpendicular (or nearly so) to this direction are better camouflaged and heal more favorably than those made parallel because these contractile forces tend to approximate the wound margins, rather than distract them apart. Understanding this concept is critical because it determines the difference between a long-term mediocre or superior scar revision. For various regions of the face, various scar revision techniques are used [17].
Cheek
The cheek represents a unique anatomic site in scar revision because the RSTLs do not run straight but rather in a curvilinear fashion from the malar eminence to the inferior border of the mandible. Scars crossing the cheek in the direction of the RSTLs are best treated with a running W-plasty (see image below). The surgeon may use a lateral-end Z-plasty for superior cosmesis. However, scars often run perpendicular (or nearly so) to the RSTL curvature mentioned above. In these cases, better camouflage is achieved by dividing the scar into multiple Z-plasties.
Nasolabial Fold
The pronounced sulcus of the nasolabial fold (ie, cheek-lip fold) is well suited to scar camouflage. Understanding the proper use of Z plasty is critical in this area where Z plasty may be used, either singly or in conjunction with a running W-plasty, for scars extending from the cheek and crossing the nasolabial fold. Of critical importance are the orientation of the lateral limbs and the angle at which they subtend the Z-plasty central limb. In designing the lateral limbs of the Z-plasty, only one combination yields the best cosmetic result and places the lateral limbs nearest the direction of the RSTL.
Mentum
Scars crossing horizontally over the mentum generally follow RSTLs and therefore are best treated with a running W-plasty Laterally based and more obliquely directed scars are good candidates for Z-plasty because the primary objective here is to redirect the scar in the RSTL direction. Often, these scars cross from an oblique lateral to a more horizontal orientation and require a combination of lateral Z-plasty and running W-plasty over the mentum.
Forehead
The underlying frontalis muscle creates unusually prominent forehead RSTLs. These well-defined lines run horizontally in the central forehead with their lateral ends projecting obliquely inferior over the temple region. Pay particular attention to the junction of the glabella and forehead. The vertical RSTLs of the glabella meet those of the forehead in a nearly perpendicular orientation. Correction of scars that cross both of these regions probably requires incorporation of differing revision techniques that redirect by Z-plasty and cause irregularity by W-plasty or that use simple fusiform excision.
Eyebrow
The prominence of the supraorbital rim renders it a probable site of injury in frontal facial trauma. Lacerations frequently cross the forehead to include the eyebrow and are a revision challenge because of their visibility and because they require special techniques to camouflage the scar within the brow hair. Important concepts in eyebrow revision procedures include creating irregularity within the scar and beveling incisions parallel to the hair shaft. W-plasty is the revision procedure of choice and requires particular attention in aligning the superior and inferior borders of the brow.
CONCLUSIONS
Abnormal scarring remains one of the major problems faced by surgeons and their patients. Surgical treatment of a suboptimal scar should be undertaken only after it matures, ideally after a year. A scar can be revised by excision and linear closure, Z plasty, W plasty, geometric broken line closure or excision and cover. Appropriate post-operative care and when indicated, adjuvant therapy form an essential part of the treatment plan. Laser, dermabrasion, and other adjuvant therapies mentioned in previous sections are useful in the management of immature scar. Classification of a scar abnormality guides the choice of treatment technique. A successful scar revision can dramatically improve a patient’s quality of life. Dermatologists can employ a number of surgical scar revision techniques. While some are better suited to treat specific types of scars, they can be used in combination with each other or with adjunctive therapies to achieve optimal results.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study.
REFERENCES
1. Shockley WW, Scar revision techniquesOper Tech Otolaryngol Head Neck Surg 2011; 22: 84-93.
2. Cupp CL, Johnson MB, Larrabee WF, Scar revisionFacial Plast Surg Clin North Am 1998; 6: 195-201.
3. Cooper JS, Lee BT, Treatment of facial scarring: Lasers, filler, and nonoperative techniquesFacial Plast Surg 2009; 25: 311-5.
4. Lorenz P, Sina Bari A, Neligan PC, Scar Prevention, treatment, and revisionPlastic Surgery 2012; 1, 1: 3rd Ed. New York: Elsevier Saunders; 297-318.
5. Bianchi FA, Roccia F, Fiorini P, Berrone S, Use of patient and observer scar assessment scale for evaluation of facial scars treated with self-drying silicone gelJ Craniofac Surg 2010; 21: 719-23.
6. Kaplan B, Potter T, Moy RL, Scar revisionDermatol Surg 1997; 23: 435-42.
7. Schweinfurth JM, Fedok F, Avoiding pitfalls and unfavorable outcomes in scar revisionFacial Plast Surg 2001; 17: 273-8.
8. Mostafapour SP, Murakami CS, Tissue expansion and serial excision in scar revisionFacial Plast Surg 2001; 17: 245-52.
9. McGillis ST, Lucas AR, Scar revisionDermatol Clin 1998; 16: 165-80.
10. Roggendorf E, The planimetric Z-plastyPlast Reconstr Surg 1983; 71: 834-42.
11. Rohrich RJ, Zbar RI, A simplified algorithm for the use of Z-plastyPlast Reconstr Surg 1999; 103: 1513-7.
12. Rodgers BJ, Williams EF, Hove CR, W-Plasty and geometric broken line closureFacial Plast Surg 2001; 17: 239-44.
13. Borges AF, W-plastyAnn Plast Surg 1979; 3: 153-9.
14. Shockley WW, Scar revision techniques: Z-plasty, W-plasty, and geometric broken line closureFacial Plast Surg Clin North Am 2011; 19: 455-63.
15. Park SS, Scar revision through W-plastyFacial Plast Surg Clin North Am 1998; 6: 157-61.
16. Thomas JR, Prendiville S, Update in scar revisionFacial Plast Surg Clin North Am 2002; 10: 103-11.
17. Mustoe TA, Cooter RD, Gold MH, Hobbs FD, Ramelet AA, Shakespeare PG, International advisory panel on scar management. International clinical recommendations on scar managementPlast Reconstr Surg 2002; 110: 560-71.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.


Comments are closed.