Dermatoporosis, an emerging disease: case report
María Lorena Re Domínguez, Beatriz Di Martino Ortiz, Mirtha Rodríguez Masi, Oilda Knopfelmacher Domínguez, Lourdes Bolla Argüello de Lezcano
Department of Dermatology, Clinicas Hospital, Faculty of Medical Sciences, National University of Asuncion, Paraguay
ABSTRACT
The term dermatoporosis proposed by Kaya and Saurat in 2007, relates to the failure and chronic skin fragility due to aging. The first clinical manifestations appear by the age of 60, but fully developed signs of disease are evident among people between the ages of 70 and 90; affecting 1 in 3 people, with a prevalence of 32%. Typical manifestations of dermatoporosis are skin atrophy, senile purpura, stellate scars, skin lacerations, and dissecting hematomas. Injuries can be classified into primary and secondary. The primary are related to the timing of aging and photoaging; while secondary lesions are associated with chronic use of topical or systemic corticosteroids. The lesions usually appear on sun-exposed areas. They indicate the fourth stage. We report a case of a 74- year- old woman with deep dissecting extremity hematomas.
Key words:Dermatoporosis; Photoaging; Cutaneous dissecting hematomas
INTRODUCTION
The skin is the largest organ of our body and noteworthy it provides a protective barrier from external aggression. With skin aging, normal process mainly characterized by appearance of wrinkles, forms a thinner and dry skin, and all metabolic and physiological functions of loosing skin functionality. When skin aging is mainly exacerbated by lossing or decreaseing amount of intradermal hyaluronic acid, a modification of the extracellular matrix is produced by the likely effect of ultraviolet radiation or the non-enzymatic glycation of structural proteins, causing loosing skin elasticity [1–3].
Skin aging, may also have similar pathological signs to brittle bones (osteoporosis), consisting of an exaggerated skin fragility presenting with erosion and ulcers [4], similar to bedridden patients ulcers where the collagen in the dermis could be affected. This is known as a chronic failure of the skin or dermatoporosis.
Aging skin, weakened by the combination of chronological aging and photoaging, may have diminished the forces of friction and shear tolerance; so both processes, the chronological and photoaging have been cited as risk factors for developing pressure ulcers. Although mentioned the delay in wound healing as a feature of dermatoporosis, there are few publications that relate to the development of pressure ulcers with this condition. [5,6].
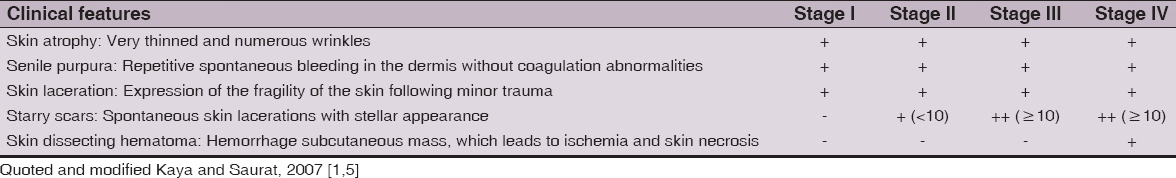
This syndrome consists of some structural tissue abnormalities including modifications of the extracellular matrix such as collagen and elastic fibers, and alterations in skin viscoelasticity. Furthermore, the histopathology of the lesions characteristic can show the flattening of the rete ridges and solar elastosis [7]. The lesions usually appear on sun-exposed areas such as the forearms, back of hands, anterior legs and chest; moreover, these areas are accesible to scratching because of the pruritus caused by dry skin itself and in many cases this scratching is the cause of injuries [3,4,8]. Within the morphological signs of dermatoporosis the presence of senile purpura, skin atrophy and scars are included. The loss of protection function results in delayed healing, lacerations after a minor trauma or deep bruises forming dissecting that, if are not drained, evolving into large necrotic areas [8]. 4 stages have been described [1,5,9] (Table 1).
Stage I is characterized by the presence of senile purpura, skin atrophy and scarring. Stage II also associates some located lacerations. Stage III has multiple lacerations and is associated with delayed healing. Stage IV associated dissecting deep bruises evolving into large areas of necrosis [1,8]. They are deep dissecting bruises on legs after the minor trauma. The vessels, which are fragile by age and placed under an atrophic skin, bleed easily. The bleeding vessel are located between the subcutaneous tissue and muscle fascia, and initially manifests clinically as red, edematous areas, with increased local temperature, which is clinically confused with cellulitis, which are usually treated with oral antibiotics. If the subcutaneous hematoma is not drained at the proper time, the ischemia of skin occurs and appear large necrotic areas requiring wide surgical debridement. The differential diagnosis must include vascular occlusion syndromes that affect the skin, mainly non inflammatory causes, although some may present with minimal inflammatory clinical lesions and skin necrosis. These syndromes result in clinically retiform purple type of injuries that can evolve into necrotic areas [1,8]. Healing of these wounds can be prolonged due to a process in which there is a decreased fibroblastic proliferation, which can be accompanied with local exudates, the risk of bacterial colonization and increased metalloproteases in exudates.
According to the stages [8] management schemes have been proposed: In stage I, II and III, it is proposed to perform applications of paraffin oil, debridement of scabs and small necrotic areas, application of Lanolin-based emollient, zinc oxide and hyaluronic acid throughout the affected area and cover with hydrocolloid meshes to avoid wetting the wound to the bed, to the secondary dressing of calcium alginate or according to the level of exudate gauze compresses applying a clamp or a semi compressive dressing.
Dermatoporosis in stage IV cases, requires a surgical debridement of the hematoma, ablution the lesion with saline solution and application of a desbridante dressing composed of Ringer, along with a cleaning solution with Polihexanide, also checking that the bed of the lesion does not show tunelization.
Once presented granulation tissue in the wound bed, is proposed to continue with the process of healing and epithelization, with the application of hyaluronic acid more topical retinaldehyde; according to some clinical trials performed for the treatment of the dermatoporosis, fragmented hyaluronic acid and the retinaldehyde show an effect dependent on the dose in the correction of atrophy of the skin [8,10].
CASE REPORT
Female, 74, housewife, from an urban area of Paraguay, admitted in an intensive care unit (ICU) of a public hospital for/because of sepsis with starting point in an urinary tract infection, which is treated with ceftriaxone. In its 8th day of hospitalization in ICU appearance of edema of both arms, with redness, prone to spontaneous bleeding and citrine suffusion fluid following minimum procedures. The case is interpreted as cellulite on upper limbs and after clinical worsening ceftriaxone is rotated to piperacilin tazobactam. In its 12th day of hospitalization a dermatological evaluation is performed because of the erythema and bruises on arms and legs.
Personal history: 3-month history of violaceous macules and bruises that appear spontaneously, without accompanying symptoms, difficult to cure, which are increasing in number. Fine, dry and frequently itching skin.
Physical exam: skin atrophy. Bruises of 3-20 cm -some of them qualify to be dissecting and lacerations from 1.5 to 10 cm in upper and lower limbs. Erosion of 15 cm in diameter with necrotic and jagged edges, in legs and thighs (Figs 1 and 2).
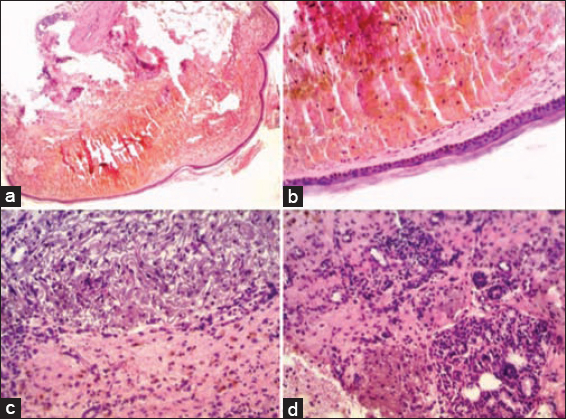
Histopathology: epidermal atrophy with loss of rete ridges and basal hyperpigmentation. Orthokeratosis.
Vaso congestion and superficial dermal vasodilation with significant hematic extravasation. Degeneration of elastic and collagen fibers in the dermis (Fig. 3).
Ultrasound of soft tissue: subcutaneous edema and important collection of lumps in both arms.
Laboratory: blood count with leukocytosis, neutrophilia and severe anemia (WBC 12,700/mm3 N: 80% L20%, Hb 5.9 g/dl hematocrit 20%); Normal blood pressure (PT 75% Platelets 247,000/mm3; APTT 24 seconds, fibrinogen 300mg/%), urea, creatinine, electrolytes, and normal liver function. Hypoalbuminemia (2,4 gr/L). Urine culture: E. coli..
Dermatological Diagnosis: Stage IV dermatoporosis.
Treatment: Surgical drainage of hematomas on both arms but bleeding persist in extremities. Cures with isotonic saline, vaseline petroleum jelly and gauze to cover.
Prior to the study, patient gave written consent to the examination and biopsy after being informed about the procedure.
DISCUSSION
Due to population longevity, and therefore to the existence of an older population with multiple pathologies generally considered deleterious to the healing process, and also to polypharmacy including anticoagulants, antiplatelet drugs and steroids, more than a photo prolonged exposure, dermatoporosis constitutes an entity that will increase. One of the greatest expressions of gravity, as presented by our patient, is the development of deep dissecting bruising.
In the case reported by Ramos G., et al [2], it was a 92 years old female patient with factors considered of risk for developing this condition such as been a carrier of Diabetes Mellitus, Hypertension and Chronic Respiratory Failure among others comorbidities, and therefore she had been only treated with antiplatelet agents, and inhaled corticosteroids. She had a dissected hematoma in her left leg confirmed by ultrasound, and proceeded to perform a surgical debridement and subsequent topical treatments, with progressive re-epithelialization.
In the series reported by Kaya G., et al [11], of 34 patients with dermatoporosis over a period of 7 years, the dissecting hematomas were located deep in the legs in all patients. The mean age of patients was 81.7 years and 85.3% of patients were women, being a ratio women/men of 5: 1. Among previous medications prescribed for these patients were inhaled corticosteroids (12%) and anticoagulant medication (29%) (aspirin, clopidogrel and acenocoumarol). Half of the patients was related to slow healing, diabetes mellitus, chronic venous insufficiency, arterial insufficiency and polyneuropathy processes. All patients except two the youngest, had advanced dermatoporosis, and the severe form was observed in older patients who were receiving long-term treatment with systemic corticosteroids. The patients reported a previous legs injury. Initial symptoms in all patients were pain and swelling of the leg. Erythema and edema were observed without fever. The skin necrosis developed as a late manifestation. Erysipelas was initially diagnosed in up to 14 patients, and 8 that had been treated with antibiotics before admission. MRI and histopathology confirmed deep anatomical location deep dissecting hematoma. Hospital treatment consisted mainly of deep incision and debridement followed by direct closure, skin grafts or wound healing by secondary activities. The average hospital stay was 3.5 weeks.
In the case of our patient, she is within the age group considered most affected, comprising from 70 to 90 years old; however had no history of prolonged regular intake of anticoagulants, antiplatelet or corticosteroids. However as influential factors in their photoaging are a Fitzpatrick II skin type, sun exposure without sun protection throughout their live, and limited to no care generally evidenced by a history of skin dryness and frequent itching skin. She had, bruises and scars in the 4 limbs and not only in the legs. The diagnosis is made by histopathology and soft tissue ultrasound; and as in the aforementioned publications, it proceeded to carry out surgical debridement and later topical cures.
Being an emerging, multifactorial and relatively newly diagnosed disease, handling protocols in relation to each of the stages, even drugs are not well define; however the consensus seems to be that before the existence of bruises they must be drawn on brevity.
CONCLUSION
Dermatoporosis is an emerging pathology inherent to the aging population, and deep dissecting hematoma is one of its major complications. Health professionals should know the symptoms and signs of this condition, as well as the risk factors involved, since diagnosis and treatment are important prognostic factors; and given the high cost involved, preventive measures should be applied as soon as possible.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Kaya G, Saurat JH, Dermatoporosis: a chronic cutaneous insufficiency/fragility syndrome. Clinicopathological features, mechanisms, prevention and potential treatmentsDermatology 2007; 215: 284-94.
2. Mengeaud V, Dautezac-vieu C, Josse G, Vellas B, Schmitt AM, Prevalence of dermatoporosis in elderly French hospital in-patients: a crosssectional studyBJD 2012; 166: 440-69.
3. Saurat JH, Dermatoporosis. The functional side of skin agingDermatology 2007; 215: 271-2.
4. Palomar Llatas F, Fornes Pujalte B, Arantón-Areosa L, Envejecimiento Cutáneo Y DermatoporosisEnfermeríadermatol 2013; 18: 8-13.
5. Kurashige Y, Minemuta T, Nagatani T, Three Cases of Sacral Pressure Ulcers Presenting Primary Dermatoporosis on the ForearmsCase Rep Dermatol 2013; 5: 73-8.
6. Kaya G, Saurat JH, Dermatoporosis: A new concept in skin agingEurop Geriatric Med 2010; 1: 216-19.
7. Kaya G, New therapeutic targets in dermatoporosisJ Nutrition, Health 2012; 16: 285-8.
8. Gamo R, Vicente J, Calzado L, Sanz H, López-Estebaranz J, Hematoma profundo disecante o estadio IV de dermatoporosis. Carta científico-clínicaActas Dermosifiliogr 2010; 101: 89-106.
9. Kaya G, Dermatoporose: un síndrome émergentRev Med Suisse 2008; 4: 1078-82.
10. Nikolic D, Ziori C, Kostaki M, Fontao L, Saurat JH, Kaya G, Hyalurosome Gene Regulation in DermatoporosisDermatology 2014; 229: 110-5.
11. Kaya G, Jacobs F, Prins C, Viero D, Kaya A, Saurat JH, Deep dissecting hematoma: an emerging severe complication of dermatoporosisArch Dermatol 2008; 144: 1303-8.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.



Comments are closed.