Polypoid melanoma: a rare clinical subtype frequently confused with benign entities
Manuel Valdebran1, Karen N Wu2, Andrew Wu3, Jacqueline M Junkins-Hopkins1
1Ackerman Academy of Dermatopathology, New York, NY, USA, 2Pathology Specialists of New England, Catholic Medical Center, Manchester, NH, USA, 3Surgical Care Group, Catholic Medical Center, Manchester, NH, USA
ABSTRACT
Polypoid melanoma represents a distinct variant of melanoma characterized by an ulcerated exophytic nodule. Although this melanocytic tumor is usually restricted to the papillary dermis, it presents with a thick Breslow level and aggressive course. Its rapidly growing vertical phase and its amelanotic nature frequently simulate benign or non-aggressive entities; leading to a delay in biopsy and resulting in an increased risk of metastasis at the time of the diagnosis.
Key words:polypoid; melanoma; dermatopathology; nodular; breslow
INTRODUCTION
Polypoid melanoma (PM) was first described by Manci in 1981 [1]. Histologically, it is differentiated from classic nodular melanoma by exhibiting an exophytic growth pattern that rarely extends into the reticular dermis [2,3]. This clinicopathologic variant is not common, and may have a delayed diagnosis. We present a case of PM to highlight the important features of this potentially aggressive subtype.
CASE REPORT
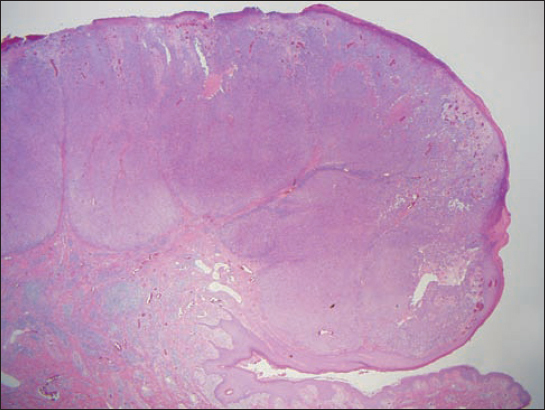
A 64 year-old male presented with a 6-month history of a rapidly growing nodule on his left flank. On physical examination, a 3 cm, well-circumscribed erythematous nodule with a partially eroded surface was found. The nodule was attached to the underlying skin by a narrow pedicle (Fig. 1). There was no lymphadenopathy. His past medical history was non-contributory.
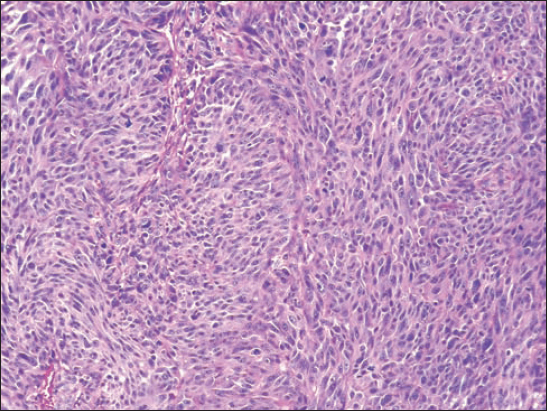
Histopathological examination of the lesion showed a polypoid tumor composed predominantly of atypical melan-A-positive melanocytes, with a nodular expansile tumor growth, poor maturation and abundant mitoses (Figs. 2 and 3). An HMB 45 immunohistochemical stain demonstrated diffuse positivity with no evidence of a gradient throughout the lesion. A computerized tomography scan failed to reveal any evidence of metastatic disease. Two sentinel lymph nodes were negative for melanoma after histological evaluation.
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure.
DISCUSSION
PM is the most common melanoma type of the gastrointestinal tract, frequently presenting as a pedunculated mucosal tumor [4]. In contrast, cutaneous PM represents a rare subtype, reported in less than a third of cutaneous melanomas [5]. Clinically, the initial stage is that of a macule exhibiting a slow radial growth, which subsequently transforms within months into a rapidly growing vertical phase [6]. The clinical differential diagnosis includes benign entities such as pyogenic granuloma, vascular malformation or non-melanoma malignant tumors such as basal cell carcinoma or squamous cell carcinoma.
Traditionally, it has been considered to be part of the nodular melanoma spectrum, however, it may also arise from the acrolentiginous, superficial spreading and lentigo maligna types, displaying a growth pattern restricted to the papillary dermis [6]. Since the tumor typically does not penetrate deeply into the reticular dermis, its aggressive behavior was considered to be somewhat unique to the pedunculated subtype. Nevertheless, it is recognized that the exophytic nature of the tumor contributes to the Breslow level which, in addition to the ulceration, dictate the aggressive course of PMs.
CONCLUSION
It is important to consider PM in the differential diagnosis when assessing pedunculated tumors. The benign appearance of PM and its amelanotic nature may delay the diagnosis, increasing the risk of metastasis and poor prognosis. Awareness of these type of tumors may offer clinicians and patients early detection and appropriate treatment.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Fabrizi G, Massi G, Polypoid Spitz naevus: the benign counterpart of polypoid malignant melanomaBr J Dermatol 2000; 142: 128-32.
2. Dini M, Quercioli F, Caldarella V, Gaetano M, Franchi A, Agostini T, Head and neck polypoid melanomaJ Craniofac Surg 2012; 23: e23-5.
3. Bandarchi B, Ma L, Navab R, Seth A, Rasty G, From melanocyte to metastatic malignant melanomaDermatol Res Pract 2010; 2010:
4. Prakoso E, Selby WS, Capsule Endoscopy for Management of Small Bowel Melanoma—Is It Time Yet?Gastroenterol Hepatol (NY) 2012; 8: 694-5.
5. Knezević F, Duancić V, Sitić S, Horvat-Knezević A, Benković V, Ramić S, Histological types of polypoid cutaneous melanoma IIColl Antropol 2007; 31: 1049-53.
6. Plotnick H, Rachmaninoff N, VandenBerg HJ, JrPolypoid melanoma: a virulent variant of nodular melanoma. Report of three cases and literature reviewJ Am Acad Dermatol 1990; 23: 880-4.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.

Comments are closed.