Chronic cutaneous lupus erythematosus with systemic symptoms or systemic lupus erythematosus?
Suresh K. Malhotra, Nidhi Sharma, Daljit Singh
Department of Dermatology, Venereology and Leprology, Government Medical College, Amritsar, Punjab, India
ABSTRACT
Chronic cutaneous lupus erythmatosus (CCLE) and Systemic lupus erythematosus(SLE) are two separate diseases with some overlapping features. Upto 28% patients with CCLE are susceptible to develop SLE. But in some cases patients may present with CCLE with systemic features without developing SLE. Here, we present a case of Chronic cutaneous lupus erythematosus with systemic symptoms simulating SLE with no positive immunological markers to support the diagnosis of SLE.
Key words: Chronic cutaneous lupus erythematosus; Negative anti-nuclear antibody; Systemic lupus erythematosus
INTRODUCTION
Chronic cutaneous lupus erythematosus (CCLE) is a benign disorder characterised with skin lesions. But in some cases in addition to skin lesions patient may present with systemic symptoms, thus mimicking Systemic lupus erythematosus (SLE). Here, we present a case of CCLE with systemic symptoms distinguished from SLE by the absence of Anti-nuclear antibody, Anti-dsDNA and Rheumatoid factor.
CASE REPORT
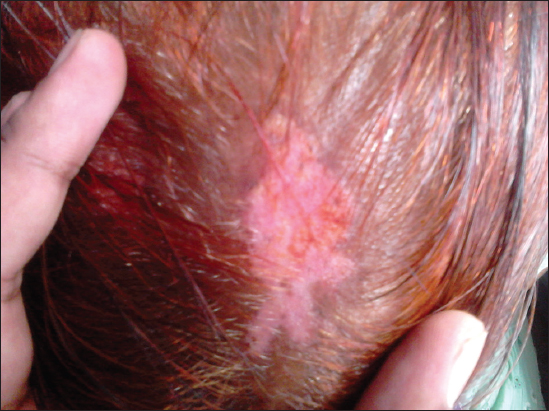
A 50 year old female presented to our hospital with complaints of hypopigmented itchy plaques over back and both pinnae since 6 years. She also complained of similar lesions in the scalp which were associated with loss of hair. History dates back to 6 years when patient noted an itchy papule on the upper back which gradually increased in size along with development of similar lesions over both pinnae and scalp over a period of next 4 years. History of photosensitivity was present. She also complained of recurrent oral ulcerations, pain and swelling in both ankle and knee joints for the past 6 years. On general physical examination she was poorly built, had pallor and diffuse non-scarring alopecia of the scalp. On mucocutaneous examination the lesions on the scalp, both pinnae and upper back were in the form of hypopigmented plaques with central atrophy and well defined irregular hyperpigmented margins of size ranging from 0.5X0.6 cm to 3X4cm (Figs 1 – 2). The lesion on the upper back had yellow coloured adherent scales in the lower half (Fig. 3). On removing the adherent scale, its undersurface showed horny plugs, so called tin-tack sign. Oral mucosa and nails were normal. On being investigated, her hemoglobin was 8.5g/dl. Total leucocyte count, Differential leucocyte count, Erythrocyte sedimentation rate, total serum proteins, differential serum proteins, fasting blood sugar, VDRL, Renal profile and Liver profile were within normal range. LE cells were not seen. Tests for Anti-nuclear antibodies, Anti-dsDNA antibodies and Rheumatoid factor were negative. Xrays showed effusion in Right knee joint and right ankle joint. Histopathology of the atrophic plaque showed acanthosis, keratotic plugging, necrotic keratinocytes, thickened basement membrane, ectatic blood vessels and focal areas of pigment incontinence. Superficial and deep perivascular and periadnexal lymphocytic infiltrate and leucocytoclastic vasculitis was also noticed. Histopathology from the scaly plaque showed marked orthohyperkeratosis, parakeratosis, acanthosis, necrotic keratinocytes, basal vacuolization and focal lymphocytic infiltrate at dermoepidermal junction. The findings were consistent with Chronic Cutaneous Lupus Erythematosus. Hence, based upon the clinical symptoms and histopathological findings she was diagnosed as a case of Chronic Cutaneous Lupus Erythematosus with systemic symptoms. The Diagnosis of SLE was not made as although the clinical criteria were fulfilled but no immunological criteria was present.
DISCUSSION
Discoid lupus erythematosus (DLE) also known as Chronic cutaneous lupus erythematosis (CCLE) is a benign disorder of the skin, clinically characterized by red scaly patches which heal with atrophy, scarring and pigmentary changes, and histopathologically by vacuolar degeneration of basal cell layer of epidermis and patchy dermal lymphocytic infiltrate. DLE is subdivided into a localized form in which lesions are confined to the face and neck or a disseminated form in which lesions also occur elsewhere on the body [1]. It has clinical variants like hypertrophic CCLE, lupus panniculitis, mucosal CCLE, tumid CCLE and chilblain CCLE. CCLE is more commonly seen in females between the age group of 20-40 years. Though all races are affected, the prevalence may be higher in African Americans than in Caucasians [2]. Genetic factors and somatic mutations are implicated in the pathogenesis of DLE. Three to five somatic mutations affecting autosomal genes and one mutation involving X-linked gene in lymphocytic stem cells of predisposed individuals, results in development of a forbidden clone of lymphocytes which synthesize cellular autoantibodies. Four temporally sequential phases are a prerequisite for clinical expression of lupus viz. inheritance of susceptibility genes, induction of autoimmunity by autoreactive T cells, expansion of autoimmune process with autoantibodies and immunological injury. Immunological injury is attributed to the action of autoantibodies and the immune complexes they form, which causes tissue damage [3].
Systemic features may be seen along with cutaneous lupus erythematosus. Up to 28% of patients with DLE are susceptible to develop systemic lupus erythematosus SLE. Various clinical and laboratory indicators, such as widespread DLE lesions, arthralgias/arthritis, nail changes, anaemia, leucopenia, high erythrocyte sedimentation rates (ESRs) and high titres of antinuclear antibodies (ANAs) are associated with progression to SLE in patients with DLE [4]. The Diagnosis of SLE can be made using the SLICC criteria given as under.
Requirements
≥ 4 criteria (at least 1 clinical and 1 laboratory criteria) or biopsy proven lupus nephritis with positive ANA or Anti-DNA.
Clinical Criteria
1-Acute cutaneous lupus. 2-Chronic cutaneous lupus. 3-oral or nasal ulcers. 4-Non-scarring alopecia. 5-Arthritis. 6-Serositis. 7-Renal. 8-Neurologic. 9-Hemolytic anemia. 10-Leukopenia. 11-Thrombocytopenia.
Immunologic Criteria
1-ANA. 2-Anti-DNA. 3-Anti-Sm. 4-Antiphospholipid Ab. 5-Low complement (C3,C4,CH50). 6-Direct Coombs’ test [5]. Although in our case four clinical criteria could be fulfilled namely 1- Chronic cutaneous lupus, 2- oral ulcers, 3- Non-scarring alopecia, 4- Arthritis but no immunological criteria was present hence a diagnosis of CCLE with systemic sympyoms was made rather than SLE.
There have been sporadic reports of neoplastic change in DLE which range from squamous cell carcinoma and basal cell carcinoma to malignant fibrous histiocytoma and atypical fibroxanthoma [6]. The incidence of squamous cell carcinoma developing in DLE ranges from 3.3 -3.4% in various studies [7].
There are various treatment modalities available for cutaneous lupus erythematosus like topical corticosteroids, topical tacrolimus, hydroxychloroquine, azathioprine, methotrexate, mycophenolate mofetil, cyclophoaphamide, cyclosporine, high dose intravenous immunoglobulin, etc [4].
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles. Written informed consent was obtained from the patient for publication of this article and any accompanying images.
REFERENCES
1. Goodfield MJ, Jones SK, Veale DJ, Burns T, Breathnach S, Cox N, Griffiths C, The connective tissue diseases (Discoid Lupus Erythematosus)Rook’s Textbook of Dermatology 2004; 7th ed. Oxford: Blackwell Science Ltd; 5-24.
2. Kanwar AJ, De D, Valia RG, Valia AR, Systemic collagen disordersIADVL Textbook of dermatology 2008; 3rd ed. Mumbai: Bhalani publishing house; 1220-66.
3. Grossman D, Leffell DJ, Freeberg IM, Eisen AZ, Wolff K, Auster KF, Goldsmith LA, Katz SI, Squamous Cell CarcinomaFitzpatrick’s Dermatology in Internal Medicine 2003; 6th ed. NewYork: McGraw Hill; 737-47.
4. Chong BF, Song J, Olsen NJ, Determining risk factors for developing systemic lupus erythematosus in patients with discoid lupus erythematosusBr J Dermatol 2012; 166: 29-35.
5. Petri M, Orbai A, Alarcon G, Gordon C, Merrill JT, Fortin PR, Derivation and Validation of Systemic Lupus International Collaborating Clinics Classification Criteria for Systemic Lupus ErythematosusArthritis Rheum 2012; 64: 2677-86.
6. Grover S, Murthy PS, Rajagopal R, Jalpota YP, Sudha KV, Discoid Lupus Erythematosus leading to Squamous Cell CarcinomaMed J Armed Forces India 2007; 63: 184-5.
7. Pandhi RK, Gupta R, Kumar SA, Bhutani LK, Discoid Lupus Erythematosus in Northern IndiaInd J Dermatol 1984; 50: 97-9.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.


Comments are closed.