Histopathological spectrum of benign melanocytic nevi – our experience in a tertiary care centre
Shivanand Gundalli1, Smita Kadadavar1, Somil Singhania1, Rutuja Kolekar2
1Department of Pathology, S N Medical College, Bagalkot, Karnataka, India, 2Department of Obstetrics and Gynaecology, S N Medical College, Bagalkot, Karnataka, India
ABSTRACT
Introduction: Melanocytic lesions show great morphological diversity in their architecture and the cytomorphological appearance of their composite cells. Histological assessment of these melanocytic nevi constitutes a substantial proportion of a dermatopathologist’s daily workload. The aim of our study was to observe the histological spectrum and types of benign melanocytic nevi and melanoma and also to identify the unusal/atypical histological features in these melanocytic nevi.
Results: Intradermal nevus was the most common benign melanocytic nevi comprising 11 (62.5%) out of the total 13 cases. In ten cases lesions were located on head and neck region. Maximum number (60%) of cases were seen between 30-40 years of age.
Conclusion: Melanocytic lesions of the skin are of notorious challengefor the pathologist. Face was the most common site and intradermal nevus was the most common lesion in our study.
Key words: Melanocytic lesions; Histological features; Intradermal nevus
INTRODUCTION
Benign Pigmented Lesions and Malignant Melanoma
Melanocytic proliferations are composed of one or more of three related types of cells: Melanocytes, nevus cells or melanoma cells, each of which may be located in the epidermis or in the dermis. Melanocytes are solitary, dendritic cells with small regular nucleus. Nevus cells are rounded or spindle shaped cells arranged in clusters with small regular nucleus. Melanoma cells are rounded or spindle shaped arranged in clusters and sheets with large irregular hyperchromatic nucleus [1].
Benign tumors of nevus cells are called melanocytic nevi, while malignant tumors are called malignant melanomas and the cells of these lesions are called as melanoma cells. Melanocytic lesions are of importance primarily because of malignant melanoma, which is the single most common potentially lethal neoplasm of skin [1].
Melanocytic Nevus
Melanocytic nevus is generally considered to be a benign neoplastic proliferation of melanocytes (Fig. 1). Melanocytic nevi are only rarely present at birth. Most nevi appear in adolescence and early adulthood. Melanocytic nevi are defined by the presence of nevus cells, which, even though they are melanocytes, differ from ordinary melanocytes by being arranged at least partially in clusters or nests, by the tendency to be round rather than having dendritic cell shape and a propensity to retain pigment in their cytoplasm [1]. Many nevi appear to be clonal [2].
There are transitional stages in the life cycle of nevi, which are believed to start out as junctional nevi, then become compound nevi and after having become intradermal nevi, undergo involution [1].
Junctional Nevi
It presents as a well circumscribed brown to black macule which can appear anywhere on the body surface and appears during childhood or early adolescence [2].
Histopathology
It is composed of nevus cells that lie in well-circumscribed nests either entirely within the lower epidermis or bulging downward into the dermis but still in contact with the epidermis. The nevus cells in these nests generally have a regular, cuboidal appearance, although they are occasionally spindle-shaped. Varying amounts of melanin granules are seen in the nevus cells [1].
Compound Nevi
They occur more commonly in children and adolescents [2]. Clinically, a compound nevus is a pigmented papule or a plaque [1].
Histopathology
A compound nevus possesses features of both a junctional and an intradermal nevus. Nevus cells in the upper, middle, and lower dermis may present characteristic morphologic variations called types A, B, and C, respectively. Usually, the type A nevus cells in the upper dermis are round to cuboidal and show abundant cytoplasm containing varying amounts of melanin granules. Melanophages are occasionally seen in the surrounding stroma. The cells in the mid-dermis usually are type B cells. They are smaller than the type A cells, display less cytoplasm and less melanin, and generally lie in well-defined aggregates or cords. Type C nevus cells in the lower dermis tend to resemble fibroblasts or Schwann cells, because they are usually elongated and possess a spindle-shaped nucleus. They often lie in strands and only rarely contain melanin [1].
Intradermal Nevus
It is the most common type of melanocytic nevi and vast majority are found in adults [2]. Intradermal nevi show essentially no junctional activity. Nevus cells are confined to the dermis where they are arranged in nests and cords. Multinucleate cells may be seen. In the deeper parts of the lesion nevus cells may assume a neuroid appearance [1].
Baloon cell nevus
This is a rare lesion clinically indistinguishable from ordinary nevus [2]. The ballooning is believed to develop from melanosome degeneration [2].
Histologically, nevus may be compound or dermal and the swollen nevus cells have clear cytoplasm and a central hyperchromatic nuclei. The diagnosis is restricted to lesions containing over 50% of balloon cells and not nevi showing focal balloon cell changes [2,3].
Halo Nevus
It is characterised by the presence of a depigmented halo several cms in width, around a melanocytic nevus [2]. Most persons with halo nevus are children or young adults, and the back is the most common site [1].
Histologically, there is dense lymphocytic infiltrate within the dermis and nevus cells are seen surviving in nests or singly among lymphocytes. Macrophages are also present in the infiltrate. The depigmented halo shows an absence of melanin pigment and melanocytes in the basal layer. Rarely a halo nevus is devoid of inflammatory cells [2]. At a later stage, only a few, and finally no distinct nevus cells can be identified [1].
Spitz Nevus
Synonym
Spindle cell nevus, epithelioid cell nevus, benign juvenile melanoma [2].
The Spitz nevus, named after Sophie Spitz, who first described it in 1948 [1,2]. The lesion usually is solitary and is encountered most commonly on the lower extremities and face. In most instances, it consists of a dome-shaped, hairless, small pink nodule. In 95% of the patients, the size of the tumor is <1 cm. Its differentiation from a melanoma can often be very difficult and occasionally even impossible [1].
Histologically, most Spitz nevi are compound, 5-10% are junctional and 20% are intradermal lesions (Fig. 2).
The Major Diagnostic Criteria Include
- Symmetrical appearance of lesion
- Cell type- epitheloid and/or spindle cells
- Maturation of nevus cells
- Lack of pagetoid spread of single melanocytes
- Coalescent, pale pink Kamino bodies.
Minor Criteria
- Junctional cleavage
- Pseudoepitheliomatous hyperplasia
- Superficial dermal edema and telangiectasia
- Giant nevus cells (multinucleate and uninucleate)
- Absence of pleomorphism.
Congenital Melanocytic Nevus
A congenital melanocytic nevus may be defined as a lesion present at birth and containing nevus cells (Fig. 3). Congenital nevi are found in about 1% to 2% of newborn infants [1]. Majority are less than 10mm in diameter [1,2]. Giant congenital nevi have the distribution of a garment(garment nevi) [1].
Histopathology
Congenital nevi may be junctional, compound or intradermal in type, depending on the age at which they are removed. Nevi removed after neonatal period show the presence of nevus cells between collagen bundles singly or in Indian file or extension of nevus cells around nerves, vessels and adnexae [2,4].
Blue Nevus
It is a small slate blue to blue black macule or papule found in the extremities, acquired after infancy. Histologically, the common blue nevus is composed of elongated, sometimes finely branching melanocytes in the interstices of dermal collagen in upper and middermis. Laterally the lesion merges with the dermis without a clear margin and macrophages containing melanin are often found [2,4].
The cellular blue nevus is composed of dendritic melanocytes with islands of epitheloid and plump spindle cells with abundant pale cytoplasm and usually little pigment. Heavily pigmented varieants do occur.
MATERIALS AND METHODS
A total of 13 cases of melanocytic nevi were studied retrospectively over a period of seven years. Skin biopsies with a primary clinical diagnosis of nevus/mole/melanoma were considered in the study. Relevant data was recorded and analysed.
Mesenchymal tumours of skin, haematological tumours of skin, neural tumours of skin, nonneoplastic lesions of skin and all tumours arising from mucosal area of mucocutaneous junction such as glans penis and eyelid margin were excluded.
The study was prospective (2years) as well as retrospective (5 years) and was done during the period of September 2004 to September 2011 i.e.7 years. Data for retrospective study was obtained from departmental records, tissue blocks and slides. Data for prospective study was obtained from clinical records, tissue specimens, tissue blocks and slides Clinical details were obtained and maintained according to the proforma.
All the biopsies and resected specimens received in the histopathology section were immediately fixed in 10% formalin for 24 hours. Gross features of the specimen were noted. Multiple sections of the specimen were taken. Then they were processed and embedded in paraffin wax. Three-five microns thick sections were prepared and then stained with Haematoxylin & Eosin.
Detailed study of the sections was performed under the light microscope and then the final diagnosis was given.
Ethical clearance
Ethical clearance has been obtained from Ethical committee of institution.
Statistical Methods Applied
Following Statistical methods were applied in the present study.
- Number and percentage
- Descriptive statistics
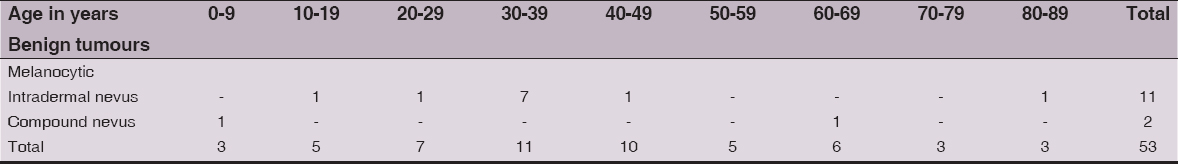
Table 1 shows age distribution of melanocytic tumours of skin.
Benign Melanocytic Tumours
Intradermal nevus
This lesion was seen in 11 cases. In all 11 cases the lesion was located in head and neck region. Maximum number (60.3%) of cases were seen between 30-40 years of age. Histologically the dermis showed nests, cords and sheets of nevus cells showing maturation. The cells showed varied amount of intracytoplasmic melanin pigment. Also few melanophages were seen in the dermis [4].
Compound nevus
This lesion was diagnosed in the two cases. One patient was a seven year old child and another was 70 year old male patient. Histologically epidermis was thinned out and showed junctional activity at dermoepidermal junction with dermal component of nevus cells showing maturation.
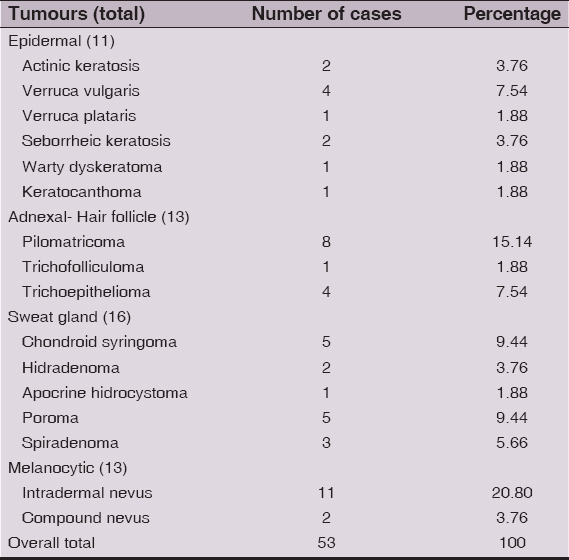
Table 2 shows comparison of melanocytic tumours of skin with distribution of different benign tumours of skin.
So to summarize the above table benign adnexal tumours formed the majority 29 cases (54.74%) followed by melanocytic tumours 13 (24.56%) and benign epidermal tumours 11 (20.70%). Thus indicating predominance of benign adnexal tumours of total 53 benign skin tumours [1,4].
CONCLUSION
Benign Melanocytic Nevus
In the present study there were 13 cases of benign melanocytic naevi, out of these 11 were intradermal and two were compound naevi. In ten cases lesions were located on head and neck region. Maximum number (60%) of cases were seen between 30-40 years of age. Shoko M, et al [1] has analyzed 531 cases of naevi out of which 15 (2.82%) were junctional, 134 (25.23%) cases were compound naevi, and 382 (71.9%)cases were dermal naevi. Thus we also noted maximum number of intradermal naevi in our study as that of Shoko M, et al.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study.
REFERENCES
1. Shoko M, The histopathological analysis of 531 cases of melanocytic nevus of the faceJap J Dermatol 2002; 112: 803-10.
2. Elder DE, Elenitsas R, Benign pigmented lesions and malignant melanomaLever’s histopathology of skin 2005; 9th ed. Philadelphia: Lippincott Raven; 715-804.
3. Weedon D, Lentigenes, nevi and melanomas. Weedon David’s Skin Pathology 2002; 2nd ed. Churchill Livingstone; 803-835.
4. Mckee PH, Brenn T, Tumours of surface epitheliumpathology of skin 3rd ed. Elsevier Mosby; 1153-1237.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.



Comments are closed.