Graham little picardi lassueur syndrome
Ritu Rawat1, Vikram K Mahajan1, Bal Chander2, Karaninder S. Mehta1, Pushpinder S. Chauhan1, Mrinal Gupta1
1Department of Dermatology, Venereology & Leprosy, Dr. R. P. Govt. Medical College, Kangra (Tanda)-176001, (Himachal Pradesh), India, 2Department of Pathology, Dr. R. P. Govt. Medical College, Kangra (Tanda)-176001, (Himachal Pradesh), India
Sir,
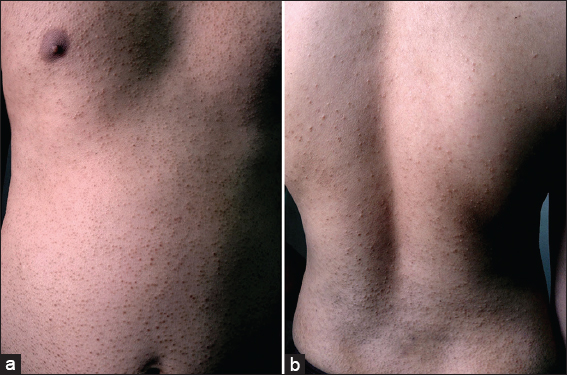
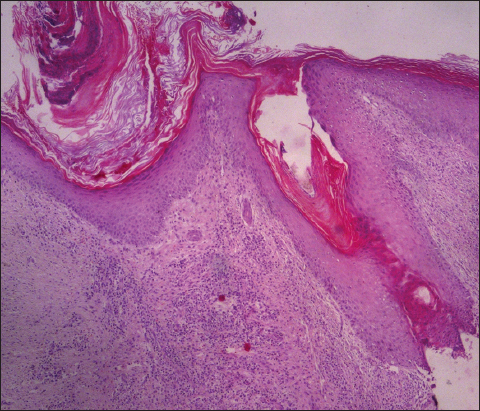
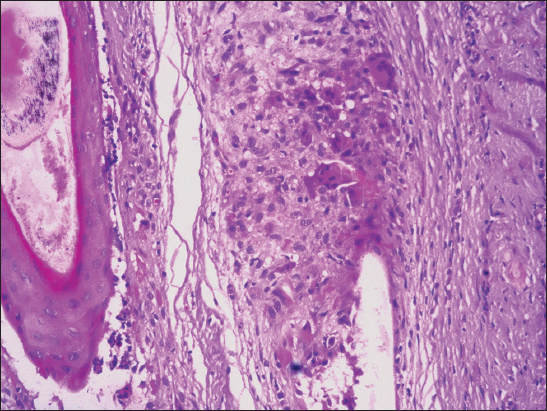
A 27-years-man presented with progressive and wide spread hair loss over scalp, axillae and pubic area for the last 3-4 years. A multitude of therapies did not benefit him and the initial hair loss over occipital area had progressed to involve the whole scalp and other body sites. His medical history was unremarkable and no other family member had similar problem. Cutaneous examination (Figs. 1 – 4) showed smooth and whitish parchment-like scalp skin, areas of variable brownish pigmentation, atrophy, scarring, and minimal scaling, and was devoid of hair. The cicatricial alopecia involved the whole scalp with few hair strands and tufts of remnant hairs particularly at scalp margins. The skin interspersed between intact hairs too had similar texture. Hair pull test was positive. The eyebrows were sparse at lateral half. Numerous erythematous-brownish follicular papules were noted over scalp margins, beard area, neck, and whole trunk. There was complete non-cicatricial alopecia in both the axillae and the pubic region showed partial non-cicatricial alopecia. Nails and mucosae were normal. Systemic examination and routine laboratory parameters including complete blood counts, serum biochemistry, ANA and thyroid function tests were normal. Histology showed features of lichen planopilaris (Figs. 5 and 6). Treatment with systemic prednisolone 30mg/day was initiated after counselling for long-term follow up in view of protracted clinical course and prognosis.
Graham Little Picardi Lassueur Syndrome is a very rare presentation of lichen planopilaris. Clinically, the triad of progressive cicatricial alopecia of the scalp, non-cicatricial alopecia involving axillae and groin, and follicular keratotic papules on the glabrous skin is characteristic. These three clinical features usually appear concurrently but scalp alopecia may precede the follicular keratosis in most instances. Pruritus, when present, is often severe. Follicular inflammation destroys hair follicles permanently with hardly any possibility of hair re-growth causing substantial scarring alopecia and significant cosmetic embarrassment leading to anxiety, psychological distress and psychosocial morbidity necessitating treatment that is more aggressive. Its exact etiology remains obscure and there is no underlying systemic disorder except for one report of its association with androgen insensitivity syndrome [1]. Most patients are females between 30 and 70 years while young males are affected very rarely [2]. There is no racial predilection but familial cases have occurred [3]. Its association with the hepatitis B vaccination too has been speculated [4]. It is considered immune mediated on the analogy of its other more common variant, cutaneous or mucosal lichen planus that occurs concurrently in about 50% cases [5]. The histologic features of infundibular hyperplasia, follicular plugging, wedge-shaped hypergranulosis, mild pigment incontinence, and dense perifollicular lichenoid infiltrate extending around its base (hugging type) are characteristic. Perifollicular lymphocytic infiltrate at the level of the infundibulum and the isthmus along with vacuolar changes of the outer root sheath are of early lichen planopilaris. More developed lesions show perifollicular fibrosis and epithelial atrophy at the level of the infundibulum and isthmus giving rise to a characteristic hourglass configuration. Alopecia with vertically oriented elastic fibres that replace the destroyed hair follicles is characteristic of advanced stage of the disease. The disease has a chronic unrelenting clinical course and needs differentiation from folliculitis spinulosa decalvans, keratosis pilaris atrophicans, pityriasis rubra pilaris, pseudopelade of Brocq and discoid lupus erythematosus. The treatment is usually symptomatic and targeted to arrest progression of disease and alopecia. Topical, intralesional or systemic corticosteroids, oral retinoids, PUVA therapy, and antimalarials have been used with a limited success. Few reports on efficacy of cyclosporin (5 mg/kg/day) are also available [6]. However, the claimed efficacy of thalidomide in lichen planopilaris remains unsubstantiated [7,8].
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Vega Gutierrez J, Miranda-Romero A, Perez Milan F, Martinez Garcia G, Graham Little-Piccardi-Lassueur syndrome associated with androgen insensitivity syndrome (testicular feminization)J Eur Acad Dermatol Venereol 2004; 18: 463-6.
2. László FG, Graham-Little-Piccardi-Lasseur syndrome: case report and review of the syndrome in menInt J Dermatol 2014; 53: 1019-22.
3. Viglizzo G, Verrini A, Rongioletti F, Familial Lassueur-Graham-Little-Piccardi syndromeDermatology 2004; 208: 142-4.
4. Bardazzi F, Landi C, Orlandi C, Neri I, Varotti C, Graham Little-Piccardi-Lasseur syndrome following HBV vaccinationActa Derm Venereol 1999; 79: 93.
5. Rodriguez-Bayona B, Ruchaud S, Rodriguez C, Linares M, Astola A, Ortiz M, Autoantibodies against the chromosomal passenger protein INCENP found in a patient with Graham Little-Piccardi-Lassueur syndromeJ Autoimmune Dis 2007; 4: 1.
6. Mirmirani P, Willey A, Price VH, Short course of oral cyclosporine in lichen planopilarisJ Am Acad Dermatol 2003; 49: 667-71.
7. Boyd AS, King LE, JrThalidomide-induced remission of lichen planopilarisJ Am Acad Dermatol 2002; 47: 967-8.
8. Jouanique C, Reygagne P, Bachelez H, Dubertret L, Thalidomide is ineffective in the treatment of lichen planopilarisJ Am Acad Dermatol 2004; 51: 480-1.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.



Comments are closed.