Gorlin syndrome: a case report
Abbas Darjani, Hojat Eftekhari, Nahid Nickhah
Department of Dermatology, Razi Medical Center, Guilan University of Medical Sciences, Rasht, Iran
ABSTRACT
Gorlin syndrome is a rare autosomal dominant disorder which characterize by multi-organ abnormities such as odontogenic keratocysts in the jaw, skeletal abnormities and multiple basal cell carcinoma etc. We report a case of this syndrome in a young man with palmar pits, multiple facial BCC, clacifications of the falx cerebri and bifid rib.
Key words: Gorlin- Golts syndrome; Nevoid basal cell carcinoma syndrome; Odontogenic keratocysts; Bifid rib
INTRODUCTION
The Gorlin syndrome, also known as nevoid basal cell carcinoma, resulting from mutation in the PTCH1 gene and inherited as an autosomal dominant trait with high penetration and variable expressivity. The estimated prevalence varies from about 1/57000 to 1/256000 with a male to female ratio of 1:1 [1]. It arises in all ethnic groups, but most of reported cases are in whites [2].
In the following we describe a case of this syndrome in a 38 year old man with emphasizing on its clinical and radiologic manifestations.
CASE REPORT
A 38 year old male patient presented to our dermatology department with numerous slow growing pigmented papules on his face and scalp. The patient first begun noticing the appearance of these lesions when he was teenager (14 years old) and then they became larger in size and number over the time and some of them became erosive recently.
He gave history of a facial swelling of the right mandible 10 years ago and subsequently had been operated for a mandibular cyst few years back.
He denied any same history and lesions in his family and child. Patient’s medical, personal and family history was non-contributory.
In physical examination dysmorphic features such as macrocephaly, prognatism and linear scar of operation in right side of his mandible were observed. Inspection revealed numerous (over 20) pigmented, some skin colour, papules and nodes on his cheeks, eyebrow, nose and scalp, predominantly on sun exposed areas (Fig. 1a). Some of these lesions were erosive. No regional lymph node was involved. The skin of his palms has tiny pits (Fig. 1b).
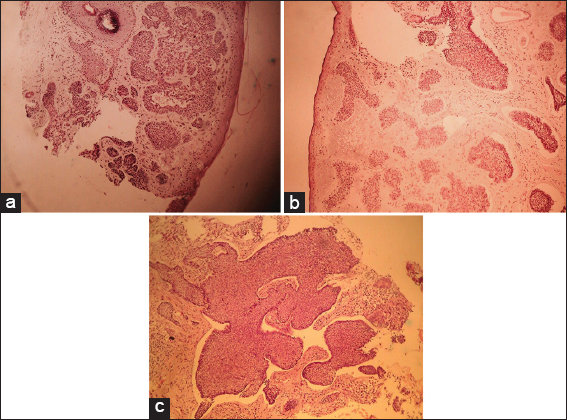
Multiple biopsies were done, the specimens were fixed in 10% formalin and submitted to histological examination and microscopically all of them showed basal cell carcinomas (multiple types such as morpheaform, micro nodular, nodular) (Figs. 2a – 2c).
The skull x-ray (AP view) showed a linear vertical radiopaque line in the midsagital plane of the cranium suggestive of calcified falx cerebri (Fig. 3a). The chest x-ray (PA) showed bifida rib (Fig. 3b).
Based on clinical, radiographic and microscopic data the diagnosis of nevoid basal cell carcinoma syndrome was established. Panoramic radiograph revealed well defined unilocular radiolucencie in maxilla (Fig. 4).
Patient underwent multiple surgical excisions with primary closure and flap for his lesions and we recommended him for regular check-ups and protection from sun exposure.
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure.
DISCUSSION
Nevoid basal cell carcinoma syndrome (NBCCS) or Gorlin-Goltz syndrome (GS) was described for the first time in 1894 by Jarisch and White [3]. This syndrome represents a series of multi-organ abnormalities known to be the consequence of abnormalities in the PTCH gene located in long arm of chromosome 9q22.3-q31 [4]. This gene has important roles in neurologic and anterior-posterior axis development as well as hair follicle formation. This explains the broad range of developmental anomalies including craniofacial, skeletal defects and the propensity for meduloblastomas, odontogenic keratocysts and multiple basal cell carcinomas to arise [5].
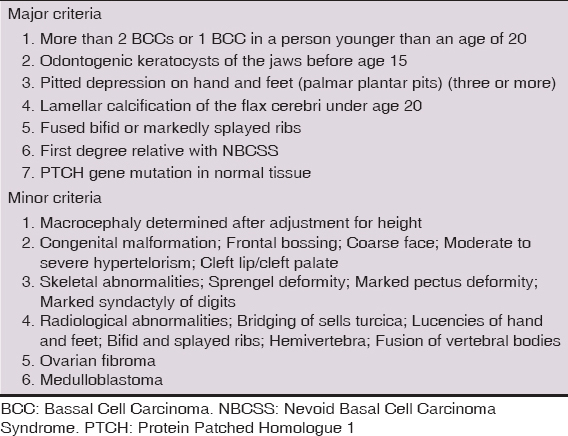
Evans et al proposed a diagnostic criteria that was further modified by Kimoni et al in 1997 (Table 1) [6,7]. The clinical diagnosis is made in the presence of two major criteria or one major associated with two minor.
Basal cell carcinomas favour the sun exposed areas of the face neck and trunk but may occur in sun protected sites too [5].
In general, the mean age of onset is about 25 years of age but it usually occur between puberty and 35th year of life [1]. And suspicion for Gorlin syndrome should be high if basal cell carcinoma are detected in pediatric age range as in our patient which is reported the onset of his lesions from fourteen years old.
Isolated cases are frequent, despite the hereditary characteristics of syndrome almost 60% of patients have no known affected family members and the absence of positive family history doesn’t exclude the diagnosis [1].
Palmoplantar pits occur in 30-65% of the patients and are 2-3 mm in diameter and 1-3 mm in depth they are found on palms commonly than soles (77% versus 50%) [8]. Lamellar calcification of the falx cerebri occur in 70-85% of these patients [9].
Odontogenic keratocyst (OKC) is the cystic lesion of odontogenic origin that illustrates the behaviour of a benign neoplasm with recurring propensity following surgical treatment. They are rarely symptomatic and can leads to the loss of bone and pathological fractures by losing the bone around the tooth [10,11].
Keratocysts may show a uni- or multilocular pattern and the cystic spaces may have a smooth or scalloped border [12]. Because of orthopantogram (OPG) findings we referred the patient to a dentist.
Through positive correlation of BCC with UV exposure the patients should be recommended for good UV protection with using sunglasses, sunscreen and avoiding from excess sun exposure.
Since the criteria of multiple BCC, multiple palmar pits, bifid rib in CXR, falx cerebri calcification, macrocephaly were present in our patient the final diagnosis of Gorlin syndrome was given.
The patient with Gorlin syndrome must be managed by several specialists such as dentist for odontogenic keratocysts, dermatologists for skin lesions and neurologists so familiarity with this syndrome is important for clinicians because of propensity of these patients to develop multiple neoplasms including basal cell carcinoma and meduloblastoma.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Muzio L, Nevoid basal cell carcinoma syndrome (Gorlin syndrome)Orphanet J Rare Dis.Diseases 2008; 3: 32.
2. Nikam B, Kshirsagar A, Shivhare P, Garg A, Familial Multiple Basal Cell Carcinoma (Gorlin’s Syndrome): A Case Report of a Father and SonIndian J Dermatol 2013; 58: 481-4.
3. Shobha CB, Ashwinirani S, Ajit SV, Veerendra SP, Gorlin Goltz syndrome: A clinicopathological case reportJ Ind Acad Oral Med Radiol 2014; 26: 85.
4. Garg P, Karjodkar F, Garg SK, Gorlin-Goltz Syndrome – Case ReportJ Clin Diag Research 2011; 5: 393-5.
5. Bolognia JL, Jorizzo JL, Schaffer JV, Bolognia’s Dermatology 3rd Edition.
6. Kimonis VE, Goldstein AM, Pastakia B, Yang ML, Kase R, DiGiovanna JJ, et al. Clinical manifestations in 105 persons with nevoid basal cell carcinoma syndrome. Am J Med Genet. 1997; 69: 299-308.
7. Evans DG, Ingham SL. Reduced life expectancy seen in hereditary diseases which predispose to early-onset tumors. Appl Clin Genet. 2013; 6: 53-61.
8. Gorlin RJ, Nevoid basal-cell carcinoma syndromeMed. (Baltimore) 1987; 66: 98-113.
9. Muzio LL, Nocini PF, Savoia A, Consolo U, Procaccini M, Zelante L, Nevoid basal cell carcinoma syndrome. Clinical findings in 37 Italian affected individualsClin Genet 1999; 55: 34-40.
10. Agani Z, Loxha PM, Krasniqi VH, Ahmedi J, Namani A, Murtezani A, Nevoid basal cell carcinoma: Case reportOpen J Stomatol 2014; 4: 29-32.
11. Sharif FN, Oliver R, Sweet C, Sharif MO. Interventions for the treatment of keratocystic odontogenic tumours. Cochrane Database Syst Rev. 2015; 11: CD008464.
12. Kalogeropoulou C, Zampakis P, Kazantzi S, Kraniotis P, Mastronikolis NS, Gorlin-Goltz syndrome: Incidental finding on routine ct scan following car accidentCases J 2009; 2: 9087.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.



Comments are closed.