A case of inverse psoriasis with interdigital involvement
Müzeyyen Gönül1, Hasan Benar1, Aysun Gökce2, Murat Alper2
1Dermatology Clinic, D?şkap? Y?ld?r?m Beyaz?t Education and Research Hospital, Ankara, Turkey, 2Pathology Clinic, D?şkap? Y?ld?r?m Beyaz?t Education and Research Hospital, Ankara, Turkey
Sir,
Inverse psoriasis is an uncommon form of psoriasis that involves intertriginous areas such as axillae and inguinal creases [1]. Interdigital psoriasis (IP), a subtype of inverse psoriasis, has been defined firstly as a distinct entity by Waisman in 1961 and this entity was called as “white psoriasis” or “psoriasis alba” [2]. There are few reported cases of IP in literature [2–4]. This report presents a case of IP who has been misdiagnosed as tinea pedis for one year and then diagnosed with the development of psoriasis lesions in other intertriginous areas.
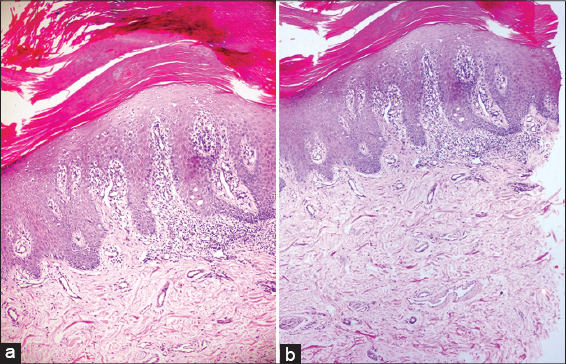
A 65-year-old woman attended with the complaints of erythematous pruritic eruptions on his axillae, inframammary and inguinal regions. The lesions had appeared on the toe web one year ago and they did not change although the patient took topical antifungal therapies several times. Later, complaints of pruritus and dandruff of scalp was added. 15 days ago red pruritic rash occured on her axillae, inguinal creases and inframamary areas. Grouped, erythematous and squamous papules on the axillae, inguinal and inframamary areas and bilaterally whitish plaque and desquamation on the 4. and 5.web of toes were detected on dermatological examination (Fig. 1). There were distal onycholysis, subungual hyperkeratosis and melanonychia striata on the toe-nails. Wood lamp examination and KOH preparation were negative. Histopatological examination of biopsy material obtained from interdigital area showed focal parakeratosis, thinning of granular layer, regular acanthosis and perivascular infiltration (Figs 2 a and b). Inverse psoriasis with interdigital involvement was diagnosed based on clinical and histopatological findings. Topical corticosteroid therapy was suggested and the complaints of the patient improved significantly.
The patient’s informed consent was obtained.
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure.
IP involves the intertoe spaces of one or both feet and is clinically characterized with macerated white, sodden patches/plaques resembling interdigital fungal infections [2–4]. There is little or no itching but sometimes fissures may occur and then itching may become more severe. The present case had severe itching [4].
The cases of IP may have other stigmatas of psoriasis and histopathological findings of IP resemble classical psoriasis but varying degrees of alterations such as atypical or incomplete parakeratosis and intermittant or intact stratum granulosum may be seen [4]. In our case, incomplete parakeratosis was seen.
Nowadays, it is debatable if IP is a distinct entity or not. Although some authors suggest that IP is a distinct atypical form of psoriasis, in a recent study, it is reported that IP is not a distinct form and it may be seen in 3.66% of the modarete or severe psoriasis patients [2–4].
IP is clinically important as it is often misdiagnosed and commonly mistaken for interdigital fungal infections [2–4]. Sometimes, coexistence of IP and interdigital fungal infections may occur, while fungal infections may superimpose psoriasis lesions, psoriasis lesions may be triggered by fungal infections due to Koebner phenomenon [4].
The treatment of IP is similar to treatment of inverse psoriasis but it may be resistant to therapy and may shows recurrences [2].
Consequently IP is a misdiagnosed form of psoriasis because of clinical similarity to fungal infections. Diagnosis of this entity may be more difficult if it occurs earlier than psoriasis lesions as in our case. So, IP must be kept in mind in patients who have interdigital lesions particularly unresponsive antifungal therapies. If native examination and fungal culture are negative skin biopsy must be obtained from interdigital lesions. These simple methods supply certain diagnosis and prevent the use of unnecessary drugs.
CONSENT
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Syed ZU, Khachemoune A, Inverse psoriasis: case presentation and reviewAm J Clin Dermatol 2011; 12: 143-6.
2. Waisman M, Interdigital psoriasis (“white psoriasis”)Arch Dermatol 1961; 84: 733-40.
3. Mommers JM, Seyger MM, van der Vleuten CJ, van de Kerkhof PC, Interdigital psoriasis (psoriasis alba): renewed attention for a neglected disorderJ Am Acad Dermatol 2004; 51: 317-8.
4. Bardazzi F, Antonucci VA, Patrizi A, Alessandrini A, Tengattini V, Interdigital psoriasis of the feet (psoriasis alba): not a distinct form of psoriasisDermatology 2013; 227: 130-3.
Notes
Source of Support: Nil
Conflict of Interest: None declared.

Comments are closed.