Dermoscopy of shagreen patch: A first report
Shivanand Gundalli, Balachandra S Ankad, Ashwin PK, Rutuja Kolekar
Department of Pathology, S N Medical College, Bagalkot, Karnataka, India
ABSTRACT
The name is derived from French phrase peau chagrinee which is usually found on lower back, buttock and thigh. The major manifestations of Tuberous sclerosis include skin lesions in more than 95%, mental retardation in approximately 50%, autism, seizures in approximately 85%. The incidence at birth is estimated to be 1 in 5800. We report case of shagreen patch in a 27 year female which is present since birth. However there is no history of seizures or consanginous marriage in our case. Associated features are naevus comedonicus and naevus collagenosis, facial angiofibroma. Shagreen patch are present in mandibular area of face. Although, diagnosis is easy, it can be mistaken for inflammatory verrucous epidermal nevus, plaques of other inflammatory skin conditions. Diagnosis is usually on clinical background. Sometimes biopsy is necessary to confirm the diagnosis. Dermoscopy, a non-invasive, in vivo technique for the microscopic examination of pigmented skin lesions, has the potential to improve the diagnostic accuracy. Dermoscopy of Shagreen patch showed reddish-brown strands with white dots giving a cobblestone appearance It can be utilized as a diagnostic aide in the diagnosis of Shagreen patch. Authors evaluated the dermoscopic patterns of Shagreen patch and hence, it is useful in diagnosis.
Key words: Dermoscopy; Shagreen patch; Tuberous sclerosis; Reddish-brown strands, White dots
INTRODUCTION
Shagreen patch (SP) was first described by Hallopeau and Leredde in 1895. Since then it has been reported to be present in 20-50% of cases of tuberous sclerosis [1].
SP is a connective tissue nevus that presents as a firm to rubbery irregular hyperpigmented rough plaque ranging in size from 1 to 10cms. The surface may resemble the surface of an orange peel. It is commonly located over the back, buttocks, thighs and nape of neck [1,2].
Although, diagnosis is easy, it can be mistaken for inflammatory verrucous epidermal nevus, plaques of other inflammatory skin conditions. Diagnosis is usually on clinical background. Sometimes biopsy is necessary to confirm the diagnosis [3].
Dermoscopy, a non-invasive, in vivo technique for the microscopic examination of pigmented skin lesions, has the potential to improve the diagnostic accuracy [4].
It can be utilized as a diagnostic aide in the diagnosis of SP. Authors evaluated the dermoscopic patterns of SP and hence, it is useful in diagnosis.
CASE REPORT
A 22 year unmarried female patient presented with skin lesions. Patient was born from non-consanguineous parents. Lesions appeared at the age of 2years on right ramus of mandible and pre-auricle. Examination revealed a thick brownish-black pigmented plaque measuring 7×4 cm extending from right ramus of mandible to the upper part of the neck on right side (Fig. 1). There were angiofibromas on the face. There were no periungual fibromas, café-au lait macules, forehead plaques or hypopigmented patches. She had a normal psychomotor development and there was no history of convulsions, mental retardation. Magnetic resonance imaging was performed to exclude other potential manifestations of tuberous sclerosis (TS). Provisional diagnosis of tuberous sclerosis was made.
Figure 1: Clinical image of shagreen patch on the right ramus of mandible.
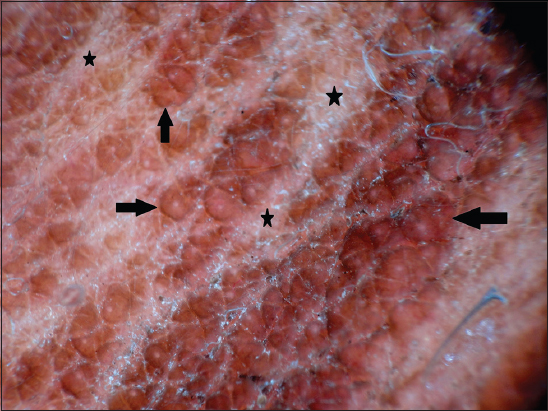
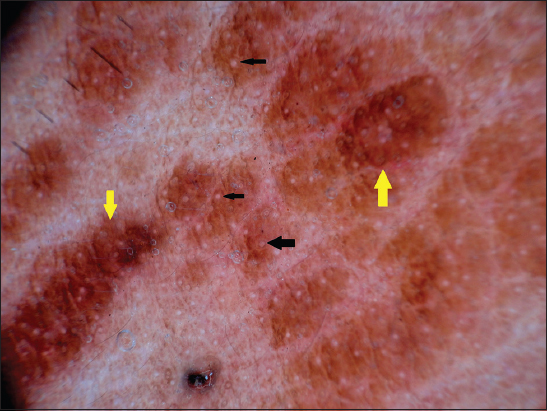
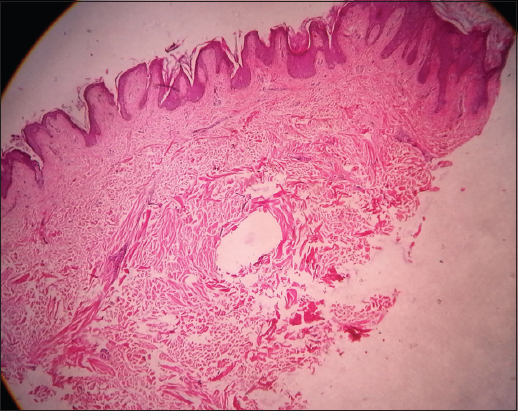
Dermoscopy of SP showed reddish-brown strands with white dots giving a cobblestone appearance (Fig. 2 and 3). Skin biopsy was taken from mandibular lesion and histopathology showed papillomatosis and dense collagen bundle in the dermis (Fig. 4).
Figure 2: Dermoscopy showing linearly arranged reddish-brown strands (black arrows) with whitish lines in between (black stars) giving a cobblestone appearance.
Figure 3: Dermoscopy showing white dots (black arrows) studded in reddish-brown strands (yellow arrows).
Figure 4: Histopathology showing papillomatosis, dense collagen bundles in the dermis. Acanthosis was present at some places, (H & E, ×10).
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure.
DISCUSSION
Dermoscopy patterns in inflammatory, melanocytic, non-melanocytic lesions correspond very much to the histological features [5].
It was utilized only for evaluation of melanoma in the past. Recently usage of dermoscopy in the diagnosis, differential diagnosis and monitoring of ectoparasitic, infectious and inflammatory skin diseases has been documented [6,7].
Hence, dermoscopic study of skin lesions will reveal histopathological changes with specific pattern and therefore, are helpful in the diagnosis of skin condition.
Cutaneous lesions are very characteristic and help in the early diagnosis of TS which is an autosomal dominant disorder characterized by seizures, mental retardation and skin findings, including congenital hypomelanotic macules and facial angiofibromas and SP [1].
SP is one of the major diagnostic features of the disease. Its frequency is less as compared to facial angiofibromas [8]. SP represents a collagenoma.
Dermis is replaced by thick collagen bundles and elastic fibers are typically absent. Fibroblasts are large and morphologically atypical [1]. Diagnosis of SP becomes impossible especially when it occurs in rare site without other signs of TS. In one report, authors observed SP in daughter and her mother over the face [9]. Therefore, SP occurring on rare sites makes it difficult to diagnose. In the present report, SP was situated on right mandible and on pre-auricle. In such scenario, biopsy is a must to prove the diagnosis. Dermoscopy can be used to diagnose SP. Till now dermoscopic patterns of SP are not described in the literature.
In the present study, authors observed reddish-brown strands on the ridges of skin lines appearing as cobblestone. They were arranged linearly with whitish lines in between which correspond to furrows of skin lines The linear strands were studded with regularly spaced white dots. The reddish-brown strands correspond to papillomatosis as well as dense collagen bundles in the dermis. White dots correspond to eccrine sweat duct openings on skin surface. Hence, dermoscopic patterns are specific and correspond well to histopathological changes of SP.
To conclude, dermoscopy shows specific patterns in SP and these patterns corresponds to the histological changes. Hence, dermoscopy enables dermatologist to diagnose SP without doing biopsy. To the best of our knowledge, this is first report of dermoscopic pattern in SP in the literature.
CONSENT
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Tsao H, Luo S, Bolognia JL, Jorizzo JL, Schaffer JV, Neurofibromatosis and Tuberous SclerosisDermatology 2012; 3rd edn. New York: Elsevier publication; 925-941.
2. Jozwiak S, Schwartz RA, Janniger CK, Michałowicz R, Chmielik J, Skin lesions in children with tuberous sclerosis complex: their prevalence, natural course, and diagnostic significanceInt J Dermatol 1998; 37: 911-17.
3. Schwartz RA, Fernandez G, Kotulska K, Jozwiak Tuberous sclerosis complex: Advances in diagnosis, genetics, and managementJ Am Acad Dermatol 2007; 57: 189-202.
4. Kittler H, Pehamberger H, Wolff K, Binder M, Diagnostic accuracy of dermoscopyLancet Oncol 2002; 3: 159-65.
5. Bowling J, Bowling J, Non-melanocytic lesionsDiagnostic dermoscopy- The illustrated guide 2012; 1st edn. West Sussex: Wiley-Blackwell; 59-91.
6. Micali G, Micali G, Lacarubbba F, IntroductionDermatoscopy in clinical practice- Beyond pigmented lesions 2010; 1st edn. London: Informa healthcare; 1-2.
7. Micali G, Lacarrubba F, Massimino D, Schwartz R, Dermatoscopy: Alternative uses in daily clinical practiceJ Am Acad Dermatol 2011; 64: 1135-46.
8. Raymond SK, Tuberous sclerosis complex and neurofibromatosis type 1: The two most common neurocutaneous diseasesNeurol Clin 2003; 21: 983-1004.
9. Patvekar MA, Jadhav AB, Tuberous sclerosis with shagreen patch over the faceMed J DY Patil Univ 2013; 6: 110-1.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.

Comments are closed.