Hidradenitis suppurativa in Down’s syndrome: A case report
Nadeem Toodayan
Associate Lecturer, University of Queensland School of Medicine, Southern Clinical School, Brisbane, Australia
ABSTRACT
Of the many dermatological conditions thought to be linked with Down’s syndrome, hidradenitis suppurativa presents a peculiar manifestation. This brief case report summarises the clinical features and possible genetic basis for this fascinating association.
Key words: Hidradenitis suppurativa; Down’s syndrome; genodermatoses; genetic basis of skin disease; clinical dermatology
INTRODUCTION
The association of hidradenitis suppurativa with Down’s syndrome has long been suspected. First proposed in 1992 by Spanish authors [1], the connection came under the spotlight again more recently in a correspondence article published in the British Journal of Dermatology [2]. Including the five cases given in that article, there have only been ten such cases recorded worldwide to date, but the actual incidence of hidradenitis in Down’s syndrome may be much higher. Here the author presents another case.
CASE REPORT
A 20 year old female Paralympian swimmer with Down’s syndrome, presented to emergency with a progressively enlarging and tender right groin lump of several weeks duration. The patient reported the finding to her mother on the same day and was brought into emergency because of the size and appearance of the lesion. The lump had started to cause the patient considerable pain more recently but she had been afebrile and well otherwise. There had been no preceding trauma or any other specific inciting event. Further questioning revealed that the patient suffered from spontaneously recurring flexural abscesses and cysts up to three times a year. They first started happening when she was in primary school and affected only her axillary and groin regions – a search of her hospital record showed that she had indeed been repeatedly diagnosed with axillary ‘abscess’ and ‘cellulitis’ in past visits to emergency. Some of these attacks were more severe than others and she once had to complete four courses of oral broad spectrum antibiotics before her axillary lesions settled. The patient could only recall having ever had one incision and drainage operation for a persisting axillary abscess. With this history, a clinical diagnosis of hidradenitis suppurativa was made. There was no significant family history of the disease.
On examination, a fairly large ellipsoid and erythematous lump measuring 40 by 20 mm was seen in the right groin crease (Fig. 1). It was firm and tender to touch and appeared to be slightly indurated superficially. A small break in the skin was noted in close vicinity to the lump but there was no purulent discharge or bleeding. The left groin was clear and there were no obvious sinus tracts or signs of scarring in the region. Minimal grade scarring was seen in both axillae but there were no active lesions present (Fig. 2). Other dermatological features of Down’s syndrome that were noted during the examination included, mild to moderate xerosis, a fairly large and fissured tongue (lingua plicata), and multiple facial syringomas that were clearly appreciable infraorbitally on the right side. There was no palmoplantar hyperkeratosis, alopecia, vitiligo, or signs of elastosis perforans serpiginosa on the examined skin. The patient denied a history of eczema, cheilitis, or any other significant skin eruptions. Her white cell count turned out to be normal and so she was discharged with oral flucloxacillin and asked to return to emergency the following morning for an ultrasound scan of her right groin.
Figure 1: The patient’s right groin abscess as seen from above (left) and closer up (right). The original lesion was much more florid and erythematous. These pictures were taken when the patient returned for her ultrasound the following day – she had already commenced taking antibiotics at this stage. The patient’s mother (hands) helped to show us the lesion. Images reproduced with kind permission from the patient and her mother.
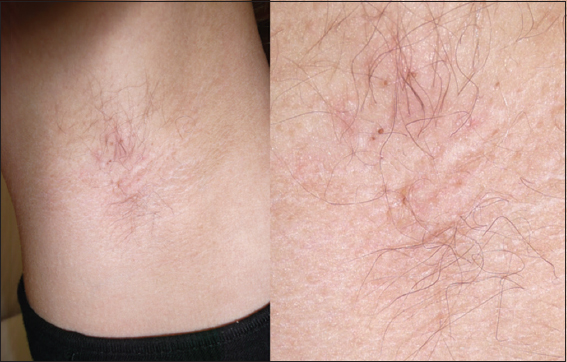
Figure 2: The patient’s right axilla showed minimal grade scarring from previous attacks of hidradenitis.
The ultrasound scan the next day showed simple abscess formation only, and by this time, the lesion had already reduced in size and redness (Fig. 1). Even so, it was incised and drained under Entonox analgesia and the small amount of pus that was extruded was sent off for microscopy and culture. The wound was left open to aid further drainage and the patient was advised to avoid swimming while it healed. After educating the patient and her mother on the condition she was advised of the possible association with Down’s syndrome. Since the history and examination findings suggested a relatively mild case of hidradenitis, the patient was asked to avoid triggers, and to present to her general practitioner in the event of a new breakout. Expert dermatological input could then be organised as required.
DISCUSSION
Although the exact pathogenesis of hidradenitis suppurativa remains to be understood, the development of the condition appears to be greatly influenced by a number of genetic and environmental factors. Notch pathway signalling defects brought on by loss of function mutations in gamma-secretase proteins like presenilin enhancer 2 (PSENEN), presenilin-1 (PSEN1), and nicastrin (NCSTN)are known to be associated with familial cases of the disease [3], and similar deficiencies have been implicated in follicular and skin appendage abnormalities in mice [4]. Activated innate immunity is also prolonged by Notch signalling defects, and this correlates with the chronic inflammatory nature of the disease [4]. All this indicates that Notch pathway signalling defects are central to the pathogenesis of hidradenitis suppurativa, but is there any causal explanation for such defects in Down’s syndrome?
A convincing answer to this question was given by Blok and colleagues in June of last year [2], when they hypothesised that the missing link between hidradenitis suppurativa and Down’s syndrome (Trisomy 21) may in fact be explained by the potential overexpression of amyloid precursor protein (APP), whose gene is located on chromosome 21. In line with the ‘gene dosage effect’ hypothesis – that is that the phenotypical features of Down’s syndrome result from the overexpression of specific genes on chromosome 21 [5]–, the authors suggest that excess APP levels in the epidermis could engender the hyperkeratosis and follicular plugging typical of hidradenitis suppurativa. Furthermore, they show how a functional decline in Notch signalling can be brought on by excess APP as it competes against Notch receptors for active binding sites on gamma secretase. The contributions of obesity and Down’s syndrome induced immune dysregulation are also listed as possible causal associations in these patients.
Our patient was not obese. She had mild mental retardation and a history of recurrent ear infections. She also had acquired hypothyroidism related to her Down’s syndrome but there was no other significant medical history. Although her symptoms were relatively mild, the case further supports the possibility of a real association between hidradenitis suppurativa and Down’s syndrome. It was only through curiosity that this association was questioned and given the relative triviality of such considerations in emergency and other generalist departments, one wonders if there haven’t been many other cases like this one which have gone by undiagnosed and therefore unreported.
CONSENT
The examination of the patient was conducted according to the Declaration of Helsinki principles. Written informed consent was obtained from the patient for publication of this article and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
REFERENCES
1. Borbujo Martínez J, Bastos Amigo J, Olmos Carrasco O, San José Hugenot I, Toribio Dapena R., Casado Jímenez M, Suppurative hidradenitis in Down’s syndrome. Apropos of three casesAn Esp Pediatr 1992; 36: 59-61.
2. Blok J, Jonkman M, Horváth B, The possible association of hidradenitis suppurativa and Down syndrome: is increased amyloid precursor protein expression resulting in impaired Notch signalling the missing link?Br J Dermatol 2014; 170: 1375-7.
3. Wang B, Yang W, Wen W, Sun J, Su B, Liu B, Gamma-secretase gene mutations in familial acne inversaScience 2010; 330: 1065
4. Melnik BC, Plewig G, Impaired Notch-MKP-1 signalling in hidradenitis suppurativa: an approach to pathogenesis by evidence from translational biologyExp Dermatol 2013; 22: 172-7.
5. Pritchard MA, Kola I, The “gene dosage effect” hypothesis versus the “amplified developmental instability” hypothesis in Down syndromeJ Neural Transm Suppl 1999; 57: 293-303.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.

Comments are closed.