Miescher granulomatous macrocheilitis: A case report
Snehal Balvant Lunge1, Pradeep Mahajan2, Vishwas Naik1
1Department of Dermatology, JNMC, Belgaum, India, 2Bhingare Laboratory, 1478 Sadashiv Peth, Opp. S. P. College Post Office, Tilak Road, Pune, India
ABSTRACT
Cheilitis granulomatosa (CG) is a chronic swelling of the lip due to granulomatous inflammation. It is a rare inflammatory disorder first described by Miescher in 1945. It is a monosymptomatic form or an incomplete variant of Melkersson-Rosenthal syndrome. As the etiology remains unknown, treatment of CG is challenging. We present a case of CG in a 20-year-old male patient presented to us with diffuse swelling of the lower lip of seven years duration. On examination, there was gross enlargement of his upper-lip. A histopathological specimen from the lower lip showed non-caseating granulomas. We treated our patient with intralesional triamcinolone acetonide and oral clofazimine. The present case highlights the importance of thorough clinical examination, history & investigations in the diagnosis of this lesion as the findings mimic many other granulomatous conditions in dermatology.
Key words: Cheilitis granulomatosa; Upper lip swelling; Melkersson-Rosenthal syndrome
INTRODUCTION
Miescher granulomatous macrocheilitis (cheilitis granulomatosa) is a mono-symptomatic form of Melkersson-Rosenthal Syndrome (triad of recurrent labial and/or recurrent facial edema, relapsing facial paralysis, and fissured tongue) [1]. The complete classical presentation of Melkersson-Rosenthal syndrome is considered to be rare, occurring in only 25 to 40 percent of cases [2]. The condition was first described by Miescher in 1945 [3]. Orofacial granulomatosis is a unifying terminology showing similar clinical features and a broad spectrum of non-necrotizing granulomatous inflammation in the oral and facial region [4]. Other entities that need to be considered in the differential diagnosis of orofacial granulomatosis include sarcoidosis, Crohn disease, and infectious disorders (e.g., tuberculosis).
CASE REPORT
A 30-year-old male was brought to our outpatient department with the chief complaint of gross swelling and deformity of the upper lip of two years duration. Initially the swelling over the upper lip was minimal and gradual progression in nature which was persistent for two years of after single honey bee bite episode. There was no significant past history for tuberculosis, crohn disease, sarcoidosis. On detailed examination, our patient showed massive enlargement and protuberance of the upper lip (Fig. 1). The lips were firm and rubbery in consistency on palpation. No regional lymph gland enlargement was present. There was no other mucosal abnormality.
Figure 1: Massive enlargement and protuberance of the upper lip.
The initial investigations revealed a normal complete blood count. The levels of serum urea and creatinine, electrolytes, serum proteins and albumin, serum calcium and serum angiotensin-converting enzyme were normal. Urine and stool analyses were normal too. VDRL tests for syphilis were negative. Chest radiograph was normal. Tuberculin skin test and abdominal ultrasound was normal.
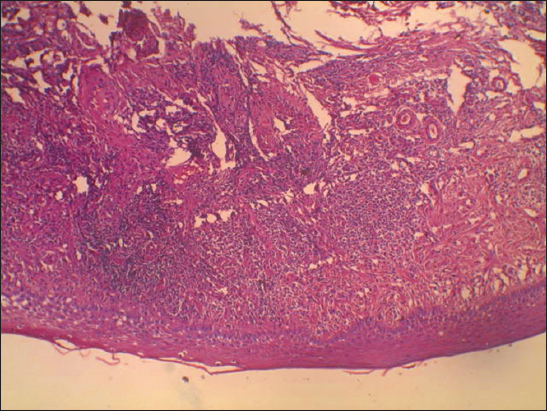
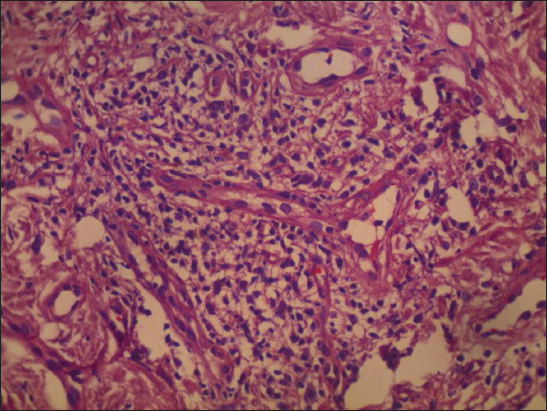
Histopathological examination of the tissue biopsy obtained from the mucosal surface of the upper lip revealed The sections show stratified squamous epithelium with atrophy at places. The dermis has focal dense superficial perivascular inflammatory infiltrate composed of lymphocytes and a few plasma cells. Occasional epithelioid cells are also seen in the present sections. In summary, in appropriate clinical settings, these histologic findings are suggestive of granulomatous cheilitis (Figs. 2 and 3).
Figure 2: Epidermis showing stratified squamous epithelium with atrophy at places. The dermis has focal dense superficial perivascular inflammatory infiltrate composed of lymphocytes and a few plasma cells. Occasional epithelioid cells are present. (H &E stain at 10x magnification).
Figure 3: The dermis showing dense superficial perivascular inflammatory infiltrate composed of lymphocytes and a few plasma cells with few epitheloid cells.(H &E stain at 40x magnification).
The patient received systemic steroids 40 mg per day for 15 days then in tapering doses till next 2 months along with oral clofazimine 100 mg three times a day (pre treatment and post treatment Figs. 1 and 4).
Figure 4: Post treatment photograph.
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure.
DISCUSSION
Granulomatous cheilitis is clinically characterized by diffuse and painless swelling of the lips. [5]. When associated with fissured tongue and facial palsy it is known as Melkersson-Rosenthal syndrome More Details [5,6]. Isolated granulomatous cheilitis, also known as Miescher granulomatous cheilitis, is sometimes considered a monosymptomatic variant of Melkersson-Rosenthal syndrome [5]. Histopathological features consist of epitheloid cell granulomas with Langhans giant cell in a mononuclear inflammatory background [7].
Cheilitis granulomatosa is considered a form fruste of Melkersson-Rosenthal syndrome. The cause is not known in the majority of the cases. But there may be genetic predisposition with increased incidence in siblings [8]. A few cases represent localized form of sarcoidosis or extraintestinal manifestation of Crohns disease [9,10]. Infective agents implicated in the etiology of granulomatous cheilitis are Toxoplasma gondii, Treponema pallidum, Mycobacterium tuberculosis, Mycobacterium leprae, Herpes simplex and Borrelia burgdorferi [8].
Cheilitis granulomatosa usually presents with recurrent and episodic swelling of the upper lip (common), which subsides in a matter of a few hours. Hence it is commonly mistaken for angioedema without undergoing for thorough investigations for patient. Gradually, the frequency of painless lip swelling increases and leads to a more persistent and firm swelling of both lips. Compression of lymphatics by the enlarging granulomas leads to an aggravation of swelling.
The differential diagnosis of acquired swelling of the lips are as following Acute causes – trauma, insect bite reaction, angioedema, anaphylaxis, drug reaction, erythema multiforme, urticaria. And chronic causes – Cheilitis granulomatosa, Sarcoidosis, Crohn disease, Melkersson-Rosenthal syndrome, Leprosy, Leishmaniasis, Syphilis, Tuberculosis, Rhinoscleroma, Malignancy, Actinic cheilitis, Cheilitis glandularis, Acromegaly, Amyloidosis, Cl esterase deficiency, foreign body granuloma.
Diagnosis of cheilitis granulomatosa relies on the typical history, clinical features and supportive evidence of non-caseating granulomas on histopathology. Two types of histology have been described for cheilitis granulomatosa (i) the sarcoid type with non-caseating granuloma consisting of epithelioid cells (histiocytes), lymphocytes, plasma cells, macrophages, and diffuse edema within the interstitial connective tissue and the (ii) lymphedematous type showing lymphatic distension, lymphedema, and plasma cell infiltration [11]. Our patient had the sarcoidal type of granulomatous inflammation present in the upper and mid dermis with edema, which corresponded to the massive swelling of his lower lip. However, no perilymphatic pathology was seen on pathology.
Treatment of cheilitis granulomatosa is a challenge for dermatologist. There are many drugs, which are reported to be useful in the management of cheilitis granulomatosa. Intralesional triamcinolone acetonide with lignocaine 2 percent is the first line of treatment for cheilitis granulomatosa [12]. Intralesional triamcinolone acetonide (10-20 mg/ml) in the volume of 1.0-1.5 ml into each side of the lip leads to prompt resolution of inflammatory granulomas. However, the response to intralesional steroid is of short duration and requires frequent painful injections. Other drugs that have been successfully used in cheilitis granulomatosa include dapsone, clofazimine [13], metronidazole [14], and roxithromycin [15]. Because of a similar pathogenesis of cheilitis granulomatosa and Crohn disease, the TNF antagonist (infliximab) has been reported to be successful in the management of cheilitis granulomatosa [16]. Owing to similar clinical and pathological features of cheilitis granulomatosa and sarcoidosis, hydroxychloroquine might prove useful in the treatment of cheilitis granulomatosa [17]. Treatment resistant and disfiguring cases of cheilitis granulomatosa need surgical intervention in the form of surgical reduction and cheiloplastic procedures with adjuvant intralesional steroid injection to prevent relapse [18,19].
CONCLUSION
We have presented a case of cheilitis granulomatosa (Miescher granulomatous macrocheilitis) secondary to honey bee bite and patient showed remarkable improvement with systemic steroids and clofazamine.
CONSENT
The examination of the patient was conducted according to the Declaration of Helsinki principles. Written informed consent was obtained from the patient for publication of this article.
REFERENCES
1. van der Waal RI, Schulten EA, van der Meij EH, van de Scheur MR, Starink TM, van der Waal I, Cheilitis granulomatosa: overview of 13 patients with long-term follow-up: results of managementInt J Dermatol 2002; 41: 225-9.
2. Zimmer WM, Rogers RS, Reeve CM, Sheridan PJ, Orofacial manifestations of Melkersson-Rosenthal syndrome. A study of 42 patients and review of 220 cases from literatureOral Surg Oral Med Oral Pathol 1992; 74: 610-9.
3. Miescher G, Über essentielle granulmatöse Makrocheilie (Cheilitis granulomatosa)Dermatologica 1945; 91: 57-85.
4. Sciubba JJ, Said-AI-Naief N, Orofacial granulomatosis: presentation, pathology and management of 13 casesJ Oral Pathol Med 2003; 32: 576-85.
5. Ghorbel IB, Sioud Dhrif A, Lamloum M, Trabelsi S, Habib Houman M, Melkersson-Rosenthal syndrome: Report of 5 cases and review of the literatureTunis Med 2006; 84: 816-20.
6. Allen CM, Camisa C, Hamzeh S, Stephens L, Cheilitis granulomatosa: Report of six cases and review of literatureJ Am Acad Dermatol 1990; 23: 444-50.
7. Wiesenfield D, Ferguson MM, Mitchell DN, MacDonald DG, Scully C, Cochran K, Oro-facial granulomatosis: A clinical and pathological analysisQ J Med 1985; 54: 101-13.
8. Hornstein OP, Melkersson-Rosenthal syndrome: A neuro-mucocutaneous disease of unknown originCurr Prob Dermatol 1973; 5: 117-56.
9. Kauzman A, Quesnel-Mercier A, Lalonde B, Orofacial granulomatosis: 2 case reports and literature reviewJ Can Dent Assoc 2006; 72: 325-9.
10. Hodgson TA, Buchanan JA, Porter SR, Orofacial granulomatosisJ Oral Pathol Med 2003; 33: 252
11. Park HS, Park ES, Park KC, Cho KH, Youn SW, Chronic idiopathic macrocheilia associated with simple lip enlargement and salivary gland hyperplasiaJ Dermatol 2008; 35: 234-7.
12. Bacci C, Valente ML, Successful treatment of cheilitis granulomatosa with intralesional injection of triamcinoloneJ Eur Acad Dermatol Venereol 2010; 24: 363
13. Ratzinger G, Sepp N, Vogetseder W, Tilg H, Cheilitis granulomatosa and Melkersson-Rosenthal syndrome: evaluation of gastrointestinal involvement and therapeutic regimens in a series of 14 patientsJ Eur Acad Dermatol Venereol 2007; 21: 1065-70.
14. Kano Y, Shiohara T, Yagita A, Nagashima M, Treatment ofrecalcitrant cheilitis granulomatosa with metronidazoleJ Am Acad Dermatol 1992; 27: 629-630.
15. Ishiguro E, Hatamochi A, Hamasaki Y, Ishikawa S, Yamazaki S, Successful treatment of granulomatous cheilitis with roxithromycinJ Dermatol 2008; 35: 598-600.
16. Barry O, Barry J, Langan S, Murphy M, Fitzgibbon J, Lyons JF, Treatment of granulomatous cheilitis with infliximabArch Dermatol 2005; 141: 1080-2.
17. Jones E, Callen JP, Hydroxychloroquine is effective therapy for control of cutaneous sarcoidal granulomasJ Am Acad Dermatol 1990; 23: 487-9.
18. Oliver DW, Scott MJ, Lip reduction cheiloplasty for Miescher’s granulomatous macrocheilitis (Cheilitis granulomatosa) in childhoodClin Exp Dermatol 2002; 27: 129-31.
19. Kruse-Lösler B, Presser D, Metze D, Joos U, Surgical treatment of persistent macrocheilia in patients with Melkersson-Rosenthal syndrome and cheilitis granulomatosaArch Dermatol 2005; 141: 1085-91.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.


Comments are closed.