Atypical pityriasis versicolor case report
Zonunsanga
Department of Skin and VD, RNT Medical college, Udaipur, Rajasthan-313001, India
ABSTRACT
Pityriasis versicolor is a superficial fungal infection caused by mycelial form of Malassezia spp, which is confined to stratum corneum. It usually present in the trunk as either hypo or hyperpigmented, aymptomatic, round to oval macules of varying sizes, which may merged to form geographic shape. Diagnosis is usually done clinically, or KOH examination which shows typical spagetti and meat balls appearances, or even by wood’s lamp which shows orange to yellow fluorescence. The case series had been recording in between 2012 to 2013. Within that period, we had recorded 32 cases. All the patients which we had recorded presented with multiple, asymptomatic macules of small sizes varying from 1-2 cm in diameter to 3-4mm in diameter, usually round to oval, hypopigmented, non scaly lesions. 26 patients had lesions on forearms, 3 patients had lesions on dorsa of hands bilaterally, 3 patients had similar kind of lesions on thigh. Besnier’s test was positive in 14 (43.75%) patients. KOH examinations showed fungal hyphae in 14 (33.33%) patients with typical spagetti and meat balls appearances in 9 (8.13%) patients. All of them were given and all of them got response and healed within 2-4 months.
Key words: Pityriasis versicolor; Malassezia; Besnier’s sign
INTRODUCTION
Pityriasis versicolor is a superficial fungal infection caused by mycelial form of Malassezia spp, which is confined to stratum corneum. It usually present in the trunk as either hypo or hyperpigmented, aymptomatic, round to oval macules of varying sizes, which may merged to form geographic shape. Diagnosis is usually done clinically, or KOH examination which shows typical spagetti and meat balls appearances, or even by wood’s lamp which shows orange to yellow fluorescence. The case series has been reported due to unusual sites and their appearances [1–6].
CASE REPORT
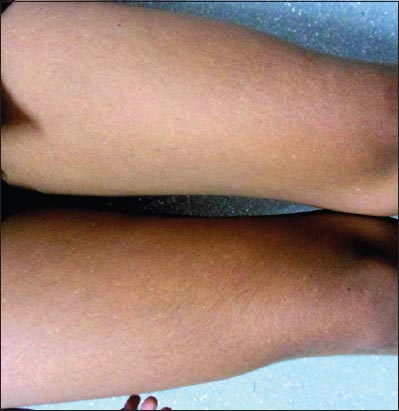
We had been recording the atypical pityriasis versicolor cases between 2012 to 2013. Within that period, we had recorded 32 cases. All the patients which we had recorded presented with multiple, asymptomatic macules of small sizes varying fromm 1-2 cm in diameter to 3-4mm in diameter, usually round to oval, hypopigmented, non scaly lesions. Among 32 patients,26 patients had lesions on forearms (Figs. 1 and 2), 3 patients had lesions on dorsa of hands bilaterally (Fig. 3), 3 patients had similar kind of lesions on thigh (Fig. 4). Besnier’s test was positive in 14 (43.75%) patients. KOH examinations showed fungal hyphae in 14 (33.33%) patients with typical spagetti and meatballs appearances in 9 (8.13%) patients. 24 patients (75%) showed fluorescence on wood’s lamp examinations. All of them were given oral fluconazole 450mg stat(as 400mg is not available in our setting) plus topical antifungals either miconazole or clotrimazole and all of them got response and healed within 2-4months. The lacunae of our study was that we did not have control site/patients. So, we could not ruled out spontaneous resolution. Clinically (by history and examinations, we ruled out other differential diagnosis which are mentioned in the discussion part as far as possible).
DISCUSSION
Pityriasis versicolor is a mild chronic superficial fungal infection (mainly Malassezia spp) of stratum corneum. The infection results from a change from its lipophilic yeast form to mycelial form of Malassezia. Yeasts are found in the body where there is abundance of sebaceous lipids. The organism enter the follicles, begin to spread and produce fine scales. The factors contributing to the infection include humid environment, hyperhidrosis, malnutrition and immunocompromised state, diabetes mellitus, Cushing’s diseases, patients on oral contraceptive pills as well as patients on corticosteroids. The pathomechanism is exact unclear. It may be associated with Delayed type hypersensitivity, release of lymphocytes by T cells, leukotrienes, which interferes with keratinocytes growth as well as collagen metabolism which may be particularly associated with atrophic type of pityriasis versicolor [1–7].
The condition is usually asymptomatic although mild itching is associated in some patients. It is characterized by patchy and scaly discloration of skin. It may be circular, oval, or even geographical due to merging of individual lesions. It may be hypopigmented due to production of dicarboxylic acid which inhibits tyrosinase, inhihibition of tanning due to overlying scales, or abnormally small melanosomes. It may be hyperpigmented also due to thicker stratum corneum, larger melanocytes and inflammatory reactions against fungus. Fluorochromes, especially pityriolactone, are linked with fluorescence in pityriasis versicolor. The typical site includes trunk, which may extend to upper arms, neck and abdomen. Atypical sites include face, genitalia, popliteal fossa, forearm and dorsa of hands and feet [3–8].
Diagnosis is done by clinical examination, KOH examination which shows typical spagheti and meat ball appearnance, and Wood’s lamp examination which shows orange to yellow fluorescence. It can be confirmed by histopathology which shows yeasts in the stratum corneum and sometimes in the perifollicular region. PAS staining is also confirmatory. Culture is rarely needed which uses Sabouraud’s dextrose agar with chloramphenicol, Acti-Dione, Tween-80 and layered with olive oil produces yellow colonies within 5-7 days. Serologically, Antibody specific to M. furfur can be determined by ELISA. Fluorescence microscopy shows green and orange fluorescent fungal elements[7–10]. The Differential diagnosis may include vitiligo, Pityriasis rosea, post inflammatory hypo or hyperpigmentation, sebhorreic dermatitis, pityriasis alba, polymorphic light eruption, secondary syphillis, and indeterminate leprosy [7–9].
Topical treatment includes 2.5% selenium sulfide, Ketoconazole shampoo for bathing, topical antifungals like clotrimazole, Miconazole, ciclopirox olamine etc, Whitfield ointment, Retinoids, Salicylic acid and Benzoyl peroxide. Systemic therapy includes Ketoconazole 200mg daily, A single dose of Fluconazole 400 mg, Itraconazole 200 mg per day for 5-7 days [11,12].
CONSENT
The examination of the patient was conducted according to the Declaration of Helsinki principles. Written informed consent was obtained from the patient for publication of this article.
REFERENCES
1. Crespo-Erchiga V, Florencio VD, Malassezia yeasts and pityriasis versicolorCurr Opin Infect Dis 2006; 19: 139-47.
2. Gaitanis G, Velegraki A, Alexopoulos EC, Chasapi V, Tsigonia A, Katsambas A, Distribution of Malassezia species in pityriasis versicolor and seborrhoeic dermatitis in Greece. Typing of the major pityriasis versicolor isolate M. globosaBr J Dermatol 2006; 154: 854-9.
3. He SM, Du WD, Yang S, Zhou SM, Li W, Wang J, The genetic epidemiology of tinea versicolor in ChinaMycoses 2008; 51: 55-62.
4. Rodoplu G, Saracli MA, Gümral R, Taner Yildiran S, Distribution of Malassezia species in patients with pityriasis versicolor in TurkeyJ Mycol Med 2014; 24: 117-23.
5. Yang YS, Shin MK, Haw CR, Atrophying pityriasis versicolor: is this a new variant of pityriasis versicolor?Ann Dermatol 2010; 22: 456-9.
6. Isa-Isa R, Cruz AC, Arenas R, Duarte Y, Linares CM, Bogaert H, Pityriasis versicolor in infants under one year of age. A report of 92 casesRev Iberoam Micol 2001; 18: 109-12.
7. Prohic A, Ozegovic L, Malassezia species isolated from lesional and non-lesional skin in patients with pityriasis versicolorMycoses 2007; 50: 58-63.
8. Gupta AK, Batra R, Bluhm R, Faergemann J, Pityriasis versicolorDermatol Clin 2003; 21: 413.
9. Lim SL, Lim CS, New contrast stain for the rapid diagnosis of pityriasis versicolorArch Dermatol 2008; 144: 1058-9.
10. Morishita N, Sei Y, Sugita T, Molecular analysis of malassezia microflora from patients with pityriasis versicolorMycopathologia 2006; 161: 61-5.
11. Muhammad N, Kamal M, Islam T, Islam N, Shafiquzzaman M, A study to evaluate the efficacy and safety of oral fluconazole in the treatment of tinea versicolorMymensingh Med J 2009; 18: 31-5.
12. Gupta AK, Lyons DC, Pityriasis versicolor: an update on pharmacological treatment optionsExpert Opin Pharmacother 2014; 15: 1707-13.
Notes
Source of Support: Nil
Conflict of Interest: None declared.



Comments are closed.