Epithelial predominant synovial sarcoma presenting as chronic non-healing ulcer of foot: A rare presentation
Gauri Salgaonkar1, Kanthilatha Pai1, Padmapriya Jaiprakash1, Sathish Pai2, Anurag Ayachit3
1Department of Pathology, Kasturba Medical College, Manipal Univeristy, Karnataka, India, 2Department of Dermatology, Kasturba Medical College, Manipal Univeristy, Karnataka, India, 3Department of Radiology, Kasturba Medical College, Manipal Univeristy, Karnataka, India
ABSTRACT
Synovial sarcoma is a morphologically and cytogenetically distinct aggressive neoplasm which presents as a deep seated painful mass in the lower extremities of young adult males. We report a rare case of synovial sarcoma presenting as a non-healing ulcer over the foot in a 29 year old male, which was misdiagnosed initially as a malignant skin adnexal tumour.
Key words: Synovial sarcoma; Epithelioid variant; Non-healing ulcer
INTRODUCTION
Synovial sarcoma is defined as a mesenchymal spindle cell tumour which displays variable epithelial differentiation including glandular formation and has a specific chromosomal translocation [1]. It is an aggressive and rare neoplasm which is histologically classified into two subtypes: monophasic and biphasic. Epithelial predominant synovial sarcoma can mimic epithelial neoplasms and is frequently misdiagnosed.
CASE REPORT
A 23 year old male patient presented to his GP with history of non-healing ulcer over the lateral aspect of the right foot for 1 month. A clinical diagnosis of Madura foot was made and a biopsy was performed, which was reported as malignant adnexal tumour at the local diagnostic centre. He was referred to our hospital for further management.
At presentation in our surgery OPD, a 4x5cm chronic non-healing ulcer was noted along the lateral and plantar aspects of the right foot having irregular margins covered with granulation tissue. An enlarged right inguinal lymph node (1x1cm) was also noted. Magnetic Resonance Imaging (MRI) was was performed, which revealed an ill-defined heterogeneous lesion along the lateral and plantar aspects of the right foot measuring approximately 5.3×4.2cm, infiltrating the subcutaneous fat, skeletal muscles and skin with surface ulceration.
FNA of the inguinal node showed reactive hyperplasia of lymphoid tissue.
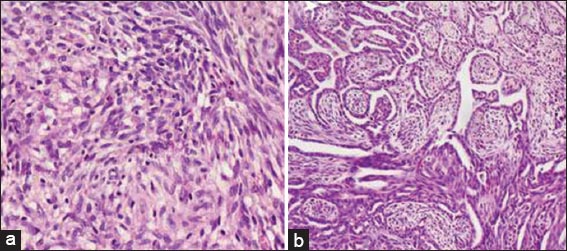
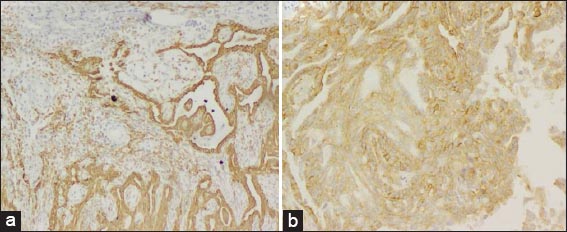
A wide excision was performed followed by split skin grafting. The excised specimen was subjected to histopathological examination which revealed a poorly circumscribed multifocal tumour composed of varying sized nodules of epithelial cells forming cleft-like and tubular spaces lined by cuboidal to low-columnar cells with nuclear pleomorphism, nests and sheets focally merging with a cellular spindle cell component with occasional mitosis. Immunohistochemically, the epithelial cells showed strong reactivity for cytokeratin and weak to moderate CD99, while the spindle cell component showed strong CD99 positivity. A diagnosis of epithelial predominant biphasic synovial sarcoma was made (Figs 1 and 2).
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure
The patient received radiotherapy over 6 weeks (total 60 Gy). Chemotherapy was started but he developed significant side-effects after the first cycle of chemotherapy with Etoposide, refused further treatment and got discharged against medical advice. Despite repeated attempts, skin grafting was unsuccessful and the patient returned two months later with a large non-healing ulcer having slough and purulent discharge. In view of the progressive nature of the disease and the deteriorating clinical condition he underwent a below-ankle amputation (Fig. 3). The subsequent postoperative period was uneventful and the patient was discharged with advice to follow up regularly.
DISCUSSION
Synovial sarcoma is a rare malignant soft tissue neoplasm typically seen in the extremities of adolescents and young adults in the age group of 15-40 years, with a predilection for knee and ankle [2]. There is a slight male preponderance with male to female ratio being 1.2:1 [3]. The term synovial sarcoma is a misnomer since it does not arise from the synovium, although at microscopy it does resemble developing synovial tissue. According to some authors, it is believed to arise from multipotent stem cells with the potential to differentiate into epithelial or mesenchymal structures [4].
It typically presents as a painful deep seated swelling or mass gradually increasing in size, unlike most other soft tissue sarcomas which are painless. Ours is a rare case which presented as a non-healing ulcerated lesion with very few similar cases having been reported in literature. One similar case was reported by Zhang at al, as a non-healing ulcer on the buttocks in a young female [5].
Microscopically, synovial sarcomas are composed of a varying proportion of well-defined epithelial cell components and fibrosarcoma-like spindle cell components, depending on which, they can be subclassified into four types:
- Biphasic with predominance of epithelial/spindle cell component
- Monophasic spindle cell/fibrous
- Monophasic epithelial and
- Poorly differentiated round cell type
A synovial sarcoma with predominance of epithelial cells and minimal spindle cell component makes it difficult to differentiate from other lesions displaying similar morphologic appearance, such as a malignant skin adnexal tumour, thus posing a diagnostic difficulty as happened in our case. The differential diagnosis includes metastatic and malignant adnexal carcinoma, malignant melanoma, malignant epithelioid schwannoma and epithelioid sarcoma [6]. Hence, small tissue biopsies showing predominantly epithelial cells with glandular formation should be viewed cautiously.
The epithelial component in our case was strongly positive for cytokeratin while the spindle component was positive for CD99 confirming our diagnosis. Thus immunohistochemistry and cytogenetic studies have proved to be excellent tools in the diagnosis. Synovial sarcomas are uniformly positive for Cytokeratin, CD99, EMA, vimentin, desmoplakin, Leu-7, S-100 protein and negative for CD34, desmin, smooth muscle actin and vascular tumour markers [4].
Recent molecular studies have shown that a majority of synovial sarcomas are associated with a specific balanced chromosomal translocation (X;18) (p11.2 q11.2) which is not associated with other sarcomas [7]. The molecular and cytogenetic studies can supplement the morphological and immunohistochemical diagnosis.
Prognosis of synovial sarcoma generally considered poor. However some studies show that not all synovial sarcomas are associated with a bad prognosis [6]. Some indicators of adverse prognosis are male gender, truncal location, tumour size more than 5cm, higher tumour grade, aneuploidy and neovascular invasion. On the contrary, young age at onset, Her-2 expression, complete tumour resection with free margins and response to chemotherapy have been defined as good prognostic indicators [4].
The preferred choice of treatment is surgery with emphasis on adequate margins. Chemotherapy and radiotherapy may be beneficial, particularly in high risk patients. According to a study by Siegel et al patients who received chemotherapy following surgery have shown better survival rates compared to those who did not. The role of radiotherapy has been controversial. According to studies by Ocku et al lack of radiotherapy is also one factor associated with poor outcome, especially in high risk patients [6].
CONCLUSION
We have reported a case of epithelial predominant biphasic synovial sarcoma presenting as a non-healing ulcer of the foot with rapid progression, that was initially misdiagnosed as a malignant skin adnexal tumour. This stresses on the point that not only is a high degree of clinical suspicion essential in evaluating young male patients presenting with non-healing ulcer of the foot, as also the role of immunohistochemistry in differentiating epithelial predominant synovial sarcoma from its mimics.
CONSENT
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Fisher C, de Bruij DR, Geurts van Kessel A, Fletcher CD, Krishnan Unni K, Mertens F, Synovial sarcomaPathology and Genetics of Tumours of Soft Tissue and Bone 2002; Lyon: IARC Press;
2. Hasan R, Kumar S, Rao L, Dumb-bell shaped poorly differentiated pelvic synovial sarcoma with molecular confirmation: A rare presentation of an uncommon disease entityIndian J Pathol Microbiol 2013; 56: 396-8.
3. Arafah M, Zaidi SN, Poorly differentiated monophasic synovial sarcoma of the mediastinumIndian J Pathol Microbiol 2011; 54: 384-7.
4. Braham E, Aloui S, Aouadi S, Drira I, Kilani T, El Mezni F, Synovial sarcoma of the chest wall: a case report and literature reviewAnn Transl Med 2013; 1: 9.
5. Zhang H-Y, Feng Y, Zhang Z, Gao G, Zhao J-S, Synovial sarcoma of the buttocks presenting with a non-healing wound and rapid progression after local resection: a case reportWorld J surg Oncol 2012; 10: 125.
6. Siegel HJ, Sessions W, Casillas MA, Said-Al-Naief N, Lander PH, Lopez-Ben R, Synovial sarcoma: clinicopathologic features, treatment and prognosisOrthopedics 2007; 30: 1020-5.
7. Oda Y, Tsuneyoshi M, Recent advances in the molecular pathology of soft tissue sarcoma: Implications for diagnosis, patient prognosis, and molecular target therapy in the futureCancer Sci 2009; 100: 200-8.
Notes
Source of Support: Nil
Conflict of Interest: None declared.

Comments are closed.