Our Dermatol Online. 2013; 4(4): 506-507
DOI:. 10.7241/ourd.20134.130
Date of submission: 09.07.2013 / acceptance: 14.08.2013
Conflicts of interest: None
CUTANEOUS MYXOID CYST ON THE SCLEROTIC FINGER IN A PATIENT WITH DIFFUSE SYSTEMIC SCLEROSIS
Taeko Nakamura-Wakatsuki, Toshiyuki Yamamoto
Department of Dermatology, Fukushima Medical University, Hikarigaoka 1, Fukushima 960-1295, Japan
Corresponding author: Prof. Toshiyuki Yamamoto e-mail: toyamade@fmu.ac.jp
How to cite an article: Nakamura-Wakatsuki T, Yamamoto T. Cutaneous myxoid cyst on the sclerotic finger in a patient with diffuse systemic sclerosis. Our Dermatol Online. 2013; 4(4): 506-507.
Abstract
Skin tumors occurring on the scleroderma fingers are rarely seen. Swollen fingers are hallmarks of systemic sclerosis, and mucin deposition in the lesional skin is a constant feature in systemic sclerosis. Here we describe a case of cutaneous myxoid cyst on the flexor aspect of the sclerotic fingers in a patient with severe diffuse cutaneous systemic sclerosis. Cutaneous myxoid cyst is a relatively common benign tumor; however, cases of cutaneous myxoid cysts developing on the scleroderma fingers have not been reported to date. Mucin deposition in the sclerotic skin may be a predisposing factor in the induction of myxoid cyst on the scleroderma finger in our patient.
Key words: systemic sclerosis; myxoid cyst; mucin
Introduction
Cutaneous myxoid cyst usually occurs in the dorsal aspect of the proximal nail fold, the distal interphalangeal joint, or under the proximal matrix [1]. Histological features show pseudocysts filled with mucoid materials which are overproduced by fibroblasts. Systemic sclerosis (SSc) is a connective tissue disorder characterized by excessive production and deposition of extracellular matrix proteins released from activated fibroblasts. Biopsy specimen reveals mucinous edema in the dermis. Although mucin deposition may be attributable to the activated scleroderma fibroblasts, myxoid cysts are not frequently seen in patients with SSc. We herein report a case of cutaneous myxoid cyst on the flexor aspect of the sclerotic finger in a patient with diffuse SSc.
Case Report
A 45-year-old woman suffering from diffuse cutaneous SSc over several years visited our department, complaining of a symptomless nodule on the finger which appeared 1 year ago. On physical examination, her fingers were swollen, pale and sclerotic, and several digital ulcers were recognized (Fig. 1). A further examination revealed a well-circumscribed, translucent nodule on the flexor aspect of her second finger (Fig. 2). Skin sclerosis involved the forearms, upper arms, chest, and face. Also, she had lung fibrosis, and been treated with prednisolone (5 mg/day) and cyclosporine (NeoralR, 75 mg/day). Laboratory data on blood chemistry including liver and renal function were within the normal range. Antinuclear antibodies (ANA) were detected in the serum (1:1280, homogenous and nuclear). Serum antibodies against Topo-I are elevated to 133.2 U/ml (normal; <10 U/ml), and the anti-U1RNP antibody was slightly elevated to 28.4 U/ml (normal; <15 U/ml). Other antibodies against centromere, DNA, ss-DNA, ds-DNA, SS-A, SS-B, Sm and cardiolipin were all negative or within normal limits. Lung CT showed interstitial fibrosis. Histopathological examination of the skin tumor showed myxomatous spaces in the dermis. The myxoid stroma was positive for alcian blue and colloidal iron staining (Fig. 3). Also, the thickened collagen bundles were observed in the lower dermis. Digital ulcers were treated with topical application of recombinant human basic fibroblast growth factor.
 Figure 1. Clinical features showing swollen, pale and sclerotic fingers with several small ulcers.
|
 Figure 2. A dome-shaped translucent nodule on the flexor
aspect of the finger. |
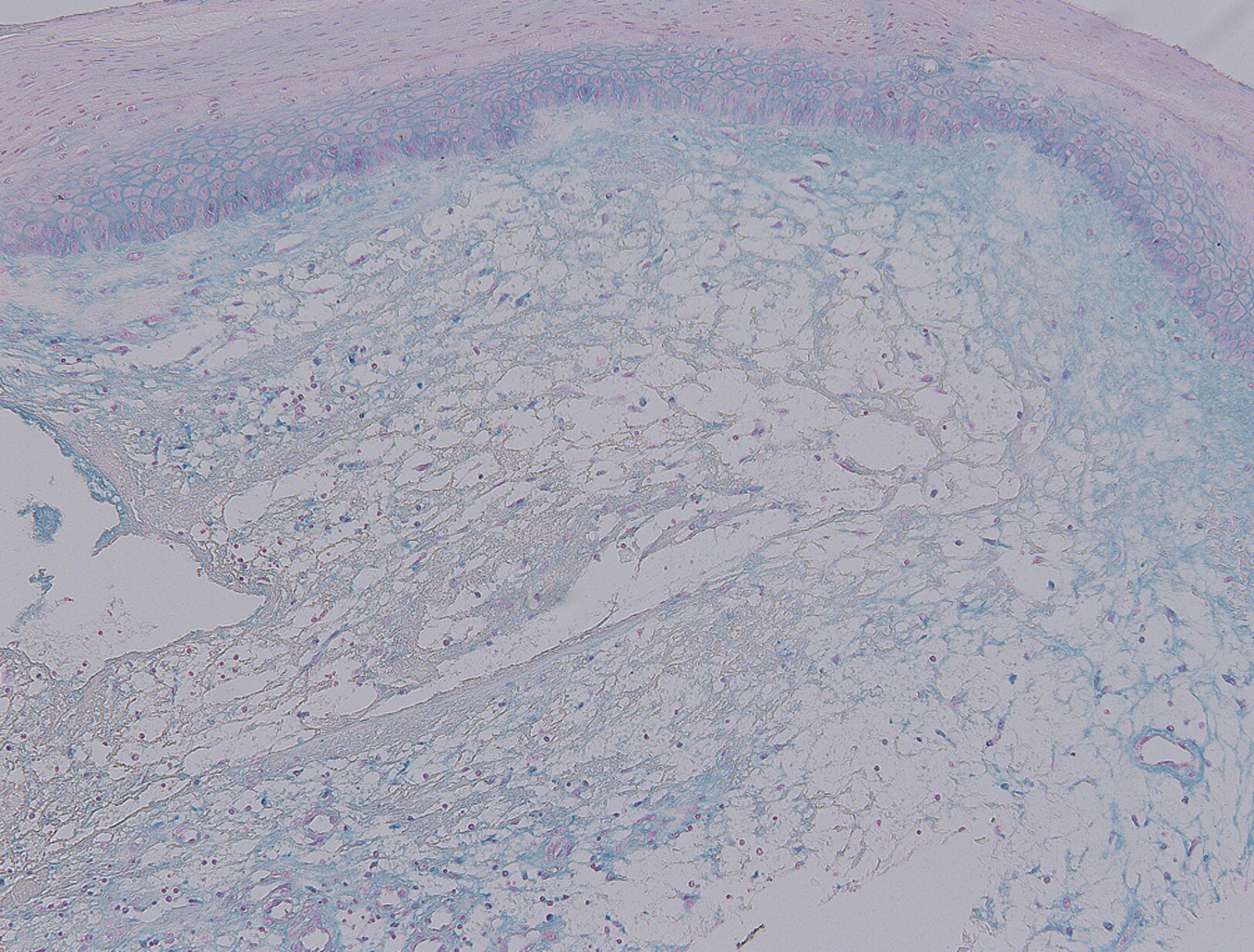 Figure 3. Histological features showing myxoid stroma in the dermis (Colloidal iron stain; x40).
|
Discussion
Cutaneous myxoid cyst is a translucent cystic nodule, frequently occurring between distal interphalangeal (DIP) joint and the proximal nail fold of the finger. In the majority of cases, myxoid cysts occur on the dorsal aspects, but sometimes on the flexor aspects of the finger [2]. Minor trauma and chronic pressure has been implicated as causative factors. Histological features show myxomatous and ganglion type. In the myxomatous type, fibroblasts are supposed to be a source of overproduction of hyaluronic acid. In the present case, mucinous nodule occurred in a patient with active diffuse SSc showing prominent sclerosis of the skin. Mucin deposition is observed in scleroderma [3], and scleroderma skin shows mucinous edema at the edematous phase.On the other hand, mucinous tumors infrequently occur in patients with SSc, and thus the occurrence of myxoid cyst may be incidental. Mucin deposition is mainly consisted of dermatan sulfate hyaluronic acid [4]. It has been suggested that mucin is produced by fibroblasts stimulated by IL-1 and IL-6. Our case developed myxoid cyst on the finger, suggesting that mechanical stimuli induced inflammatory cytokines such as IL-1 and IL-6 which exerted effects on activated scleroderma fibroblasts. Further, oxidant stress plays an important role in SSc [5], and low oxygen tension contributes to the increased fibrogenic properties of scleroderma fibroblasts, such as proliferation and collagen production [6,7]. A recent report suggests that hypoxia may play a role in the induction of dermal mucin deposition [8]. Local tissue hypoxia conditions potentially increase fibroblastic biosynthetic activity and dermal hyaluronan production. In addition, roles of CD44 variant 7 are recently reported in the accumulation of chondroitin-4-sulfate [9]. Although the occurrence of myxoid cyst may be coincidental in our case, mucin deposition produced by activated fibroblasts under several stimuli may contribute to the induction of myxoid cyst of the finger.
REFERENCES
1. Sundaram DM: Surgical correction of mucous cysts of the nail unit. Dermatol Surg. 2001;27:267-8.
2. Yamamoto T: Two cases of cutaneous myxoid cyst. Acta Derm (Kyoto). 1994;89:449-51.
3. Rongioletti F, Gambini C, Micalizzi C, Pastorino A, Rebora A: Mucin deposits in morphea and systemic scleroderma. Dermatology. 1994;189:157-8.
4. Fleischmajer R, Perlish JS: Glycosaminoglycans in scleroderma and scleredema. J Invest Dermatol. 1972;58:129-32.
5. Yamamoto T: Autoimmune mechanisms of scleroderma and a role of oxidative stress. Self Nonself. 2011;2:1-7.
6. Murrell GAC, Francis MJO, Bromley L: Modulation of fibroblast proliferation by oxygen free radicals. Biochem J. 1990;265:659-65.
7. Falanga V, Martin TA, Takagi H, Kirsner RS, Helfman T, Pardes J, et al: Low oxygen tension increases mRNA levels of alpha1(I) procollagen in human dermal fibroblasts. J Cell Physiol. 1993;157:408-12.
8. Pugashetti R, Zedek DC, Seiverling EV, Rajendran P, Berger T: Dermal mucinosis as a sign of venous insufficiency. J Cutan Pathol. 2010;37:292-6.
9. Kim JS, Bashir MM, Werth VP: Gottron’s papules exhibit dermal accumulation of CD44 variant 7 (CD44v7) and its binding partner osteopontin: a unique molecular signature. J Invest Dermatol. 2012;132:1825-32.
Comments are closed.