Our Dermatol Online. 2013; 4(3): 341-343
DOI:. 10.7241/ourd.20133.84
Date of submission: 16.04.2012 / acceptance: 21.05.2013
Conflicts of interest: None
PERIORBITAL NECROBIOTIC XANTHOGRANULOMA WITHOUT PARAPROTEINEMIA
Taeko Nakamura-Wakatsuki, Toshiyuki Yamamoto
Department of Dermatology, Fukushima Medical University, Hikarigaoka 1, Fukushima 960-1295, Japan
Corresponding author: Taeko Nakamura-Wakatsuki M.D., Ph.D. e-mail: tnw0203@gmail.com
How to cite an article: Nakamura-Wakatsuki T, Yamamoto T. Periorbital necrobiotic xanthogranuloma without paraproteinemia. Our Dermatol Online. 2013; 4(3): 341-343.
Abstract
Introduction: Necrobiotic xanthogranuloma (NXG) is a rare histiocytic disease which most frequently involves periorbital areas. NXG is associated with paraproteinemia with a ratio over 80%. However, a few cases of NXG without paraproteinemia (isolated NXG) have also been reported.
Main observation: A 58-year-old Japanese woman complained about asymptomatic dermal nodules on the bilateral lower eyelids. The histopathological examination revealed granulomatous inflammation. Paraproteinemia was not detected either in the serum or in the urine. The size of the nodules has been constant, and she has been under careful follow-up without any systemic therapies.
Conclusions: NXG is frequently associated with paraproteinemia, which may develop later. Patients with NXG need careful follow-up including repeated blood tests.
Key words: necrobiotic xanthogranuloma; no paraproteinemia; periorbital lesions.
Introduction
Necrobiotic xanthograniloma (NXG) is a rare histiocytic granulomatous disease and it is known about the complication of paraproteinuria. However, we can also see NXG without paraproteinuria and sometimes it may develop later. We herein show the case of NXG without paraproteinuria.
Case Report
A 58-year-old Japanese woman visited our department complaining of asymptomatic dermal nodules on the bilateral lower eyelids. The size of the nodules had grown gradually during these two years. She had no relevant personal and family histories. A physical examination showed a circumscribed firm dermal nodule on the right eyelid (Fig. 1a).
 Figure 1a. Border unclear firm nodule with telangiectases on the right eyelid
|
The overlying epidermis was almost normal with slight telangiectasia. On the left eyelid, a relatively well-circumscribed nodule with yellowish surface was also seen (Fig. 1b).
 Figure 1b. Yellowish nodule on the left eyelid
|
Examination by computed tomography (CT) revealed tumorous iso-density lesions on the bilateral lower eyelids, without invasion into zygomatic bones (Fig. 2).
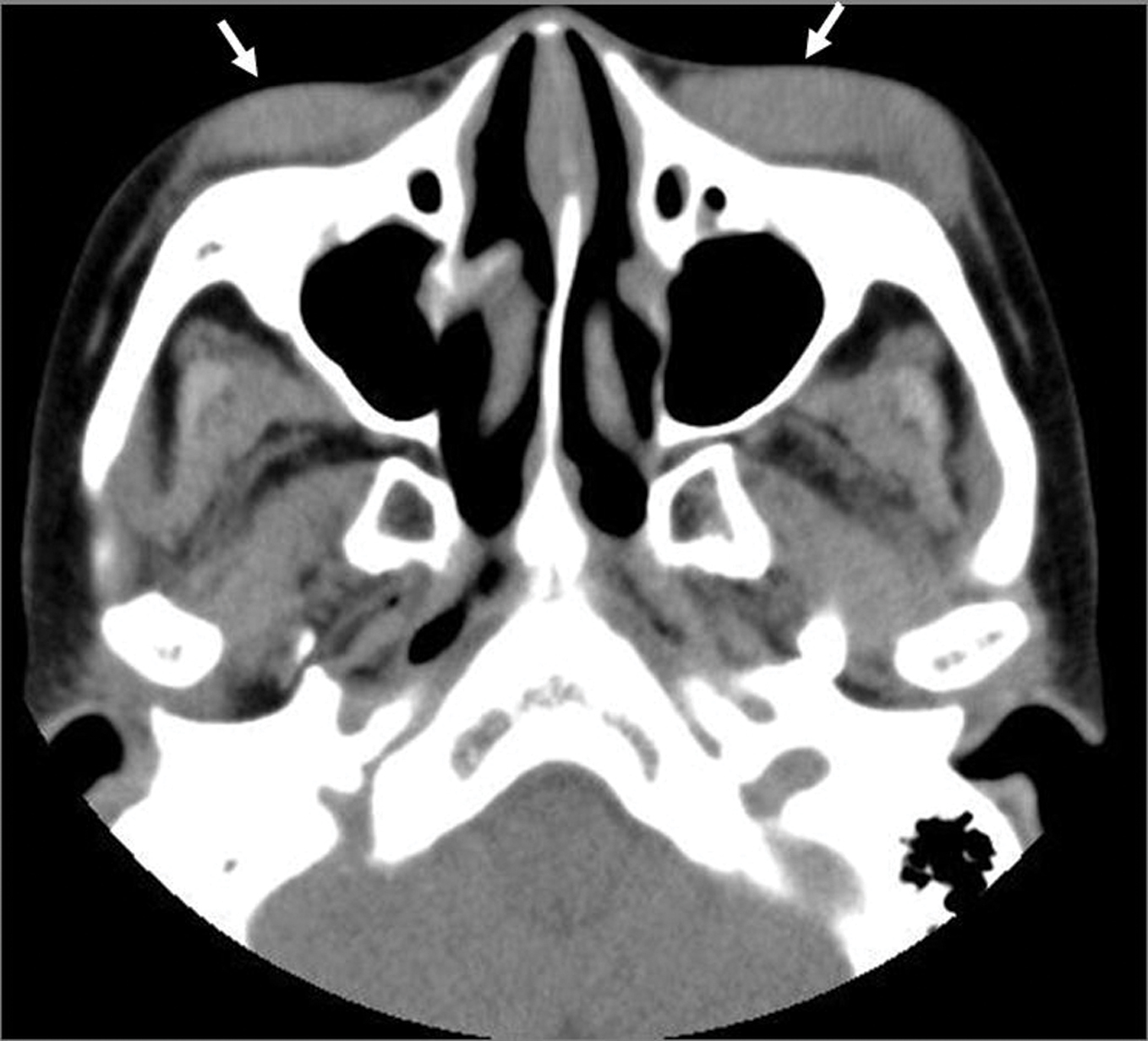 Figure 2. Tumorous lesions on the both lower eyelids(arrow), seen by computed tomography (transverse plane)
|
Histopathological examination revealed granulomatous inflammation in the upper to deep dermis. The granulomatous lesions were composed of histiocytes, foam cells, lymphocytes and Touton-type giant cells, surrounding degenerated collagen fibers (Fig. 3a, 3b).
 Figure 3a. Granulomatous inflammation is significant in the upper to deeper dermis. Touton-type giant cells are scattered (insert)
|
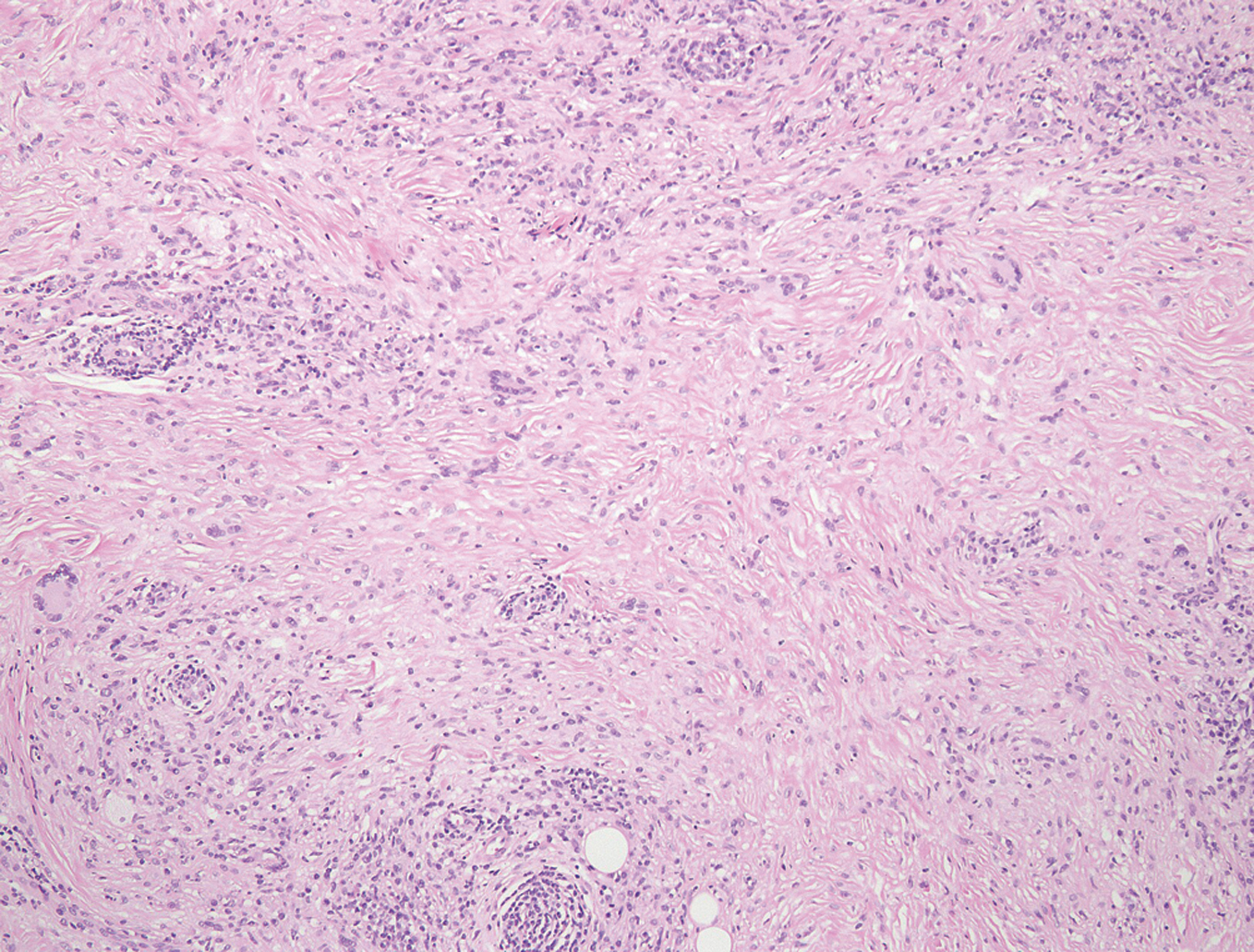 Figure 3b. The granulomas are composed of histiocytes, formy histiocytes, lymphocytes and giant cells surrounding degenerated collagen fibers
|
Immunohistochemical staining showed that the majority of infiltrating cells were positive for CD68. Based on the clinical and histological features, she was diagnosed as NXG. Laboratory findings did not show any indication of abnormalities, such as liver and renal function, and immunoglobulin levels. Serial investigations by serum electrophoresis resulted in no presence of M-protein. Bence-Jones protein was not detected in the urine. She refused either systemic (intralesional and oral) prednisolone or surgical operation. The size of the nodules has been constant, and she has been under careful follow-up.
Discussion
NXG is a rare, progressive histiocytic disease that often occurs in the fifth or sixth decade. The cutaneous lesions begin as yellowish or red-brown papules and nodules which tend to enlarge slowly. Periorbital areas are most frequently involved, and approximately 50% of the patients had ocular symptoms such as burning, itching or pain. Histopathologically, NXG shows granulomatous inflammation in the dermis, composed of foamy histiocytes, lymphocytes, foreign body-type multinucleated giant cells, and Touton-type giant cells alternating with degenerated collagen bundles [1]. Cholesterin crystals are sometimes seen.Paraproteinemia is closely associated with NXG, and monoclonal gammopathies have been described in approximately 80% of cases. For NXG patients, retrospective analysis indicated that 10-25% of patients with an associated monoclonal gammopathies of undetermined significance may subsequently develop to multiple myeloma and other malignancies such as mycosis fungoides, lymphoma, and leukemia [2]. In addition, we should consider about systemic involvement of NXG including heart, lung and kidney. The pathogenesis of NXG is still obscure. It was hypothesized that lipid-laden monocytes and immunoglobulins are deposited in the skin and elicited a giant cell inflammatory reaction [3]. On the contrary, M-protein may be the primary abnormality, and skin lesions arise from secondary proliferation of macrophages bearing receptors for Fc portion of their M-protein [4]. Another study identified spirochaetal organism in NXG lesions, suggesting infectious etiology of NXG [5]. Immunohistochemical analysis of 11 cases of NXG showed a polytypic staining pattern in the inflammatory cells and the number of the IgG4 plasma cells was not increased, suggesting that the skin lesions represent reactive inflammation [6]. Treatment of NXG is usually directed to associated hematologic disorders, with chlorambucil, corticosteroids, melphalan, cyclophosphamide, intravenous immunoglobulin, and radiation therapy. In our case, either paraproteinemia or other associated hematologic disorders were not detected. So far, only a few cases of NXG without paraproteinemia have been reported, [7,8] suggesting that NXG is not always associated with paraproteinemia or malignancies. By contrast, several papers show paraproteinemia might develop after the onset of skin lesions of NXG as long as 12 years [9] or even 20 years [10]. Further, there was a case which presented NXG after the therapy of lymphoplasmacytic lymphoma [11]. Ugurlu et al. summarized long-term outcome of 26 cases with NXG and reported that the time to emergence of hematologic disorder varied from 8 to 11 years after the onset of cutaneous lesion [12]. Thus, paraproteinemia may develop later, and patients with NXG need lifelong careful follow-up by repeated laboratory tests.
REFERENCES
1. Spicknall KE, Mehregan DA: Necrobiotic xanthogranuloma. Int J Dermatol. 2009;48:1-10.
2. Hawryluk EB, Izikson L, English JC 3rd: Non-infectious granulomatous disease of the skin and their associated systemic diseases. Am J Clin Dermatol. 2010;11:171-81.
3. Matsuura F, Yamashita S, Hirano K, Ishigami M, Hiraoka H, Tamura R, et al: Activation of monocytes in vivo causes intracellular accumulation of lipoprotein-derived lipids and marked hypocholesterolemia – a possible pathogenesis of necrobiotic xanthogranuloma. Atherosclerosis. 1999;142:355-65.
4. Langlois S, Brochot P, Reguiai Z, Bernard P, Moreau E, Gagneux-Lemoussu L, et al.: Necrobiotic xanthogranuloma with multiple myeloma. Case report and pathogenic hypotheses. Joint Bone Spine. 2006;73:120-2.
5. Zelger B, Eisendle K, Mensing C, Zelger B: Detection of spirochetal micro-organisms by focus-floating microscopy in necrobiotic xanthogranuloma. J Am Acad Dermatol. 2007;57:1026-30.
6. Wood AJ, Wagner MV, Abbott JJ, Gibson LE: Necrobiotic xanthogranuloma: A review of 17 cases with emphasis on clinical and pathologic correlation. Arch Dermatol. 2009;145:279-84.
7. Al-Niaimi FA, Dawn G, Cox NH: Necrobiosis xanthogranuloma without paraproteinaemia: marked improvement with psoralen ultraviolet A treatment. Clin Exp Dermatol. 2010;35:275-7.
8. Stork J, Kodetiva D, Vosmik F, Krejca M: Necrobiosis xanthogranuloma presenting as a solitary tumor. Am J Dermatopathol. 2000;22:453-6.
9. Ziemer M, Wedding U, Sander CS, Elsner P: Necrobiotic xanthogranuloma- rapid progression under treatment with melphalan. Eur J Dermatol. 2005;15:363-5.
10. McGregor JM, Miller J, Smith NP, Hay RJ: Necrobiotic xanthogranuloma without periorbital lesions. J Am Acad Dermatol. 1993;29:466-9.
11. Vieira V, Del Pozo J, Martinez W, Veiga-Barreiro JA, Fonseca E: Necrobiotic xanthogranuloma associated with lymphoplasmacytic lymphoma. Palliative treatment with carbon dioxide laser. Eur J Dermatol. 2005;15:182-5.
12. Ugurlu S, Bartly GB, Gibson LE: Necrobiotic xanthogranuloma: long-term outcome of ocular and systemic involovement. Am J Ophthalmol. 2000;129:651-7.
Comments are closed.