Our Dermatol Online. 2013; 4(2): 176-178
DOI:. 10.7241/ourd.20132.40
Date of submission: 23.02.2013 / acceptance: 20.03.2013
Conflicts of interest: None
SYMPTOMATIC MACROGLOSSIA AND TONGUE MYOSITIS IN DERMATOMYOSITIS
Ajili Faida1, Bousseta Najeh1, Msakni Issam2, Metoui Leila1, Gharsallah Imen1, Laabidi Janet1,
Ben Abdelhafidh Nadia1, Louzir Bassem1, Ammar Bouziani2, Othmani Salah1
1Department of Internal Medecine, Military Hospital of Tunis, 1008, Tunisia
2Department of Anatomopathology, Military Hospital of Tunis, 1008, Tunisia
Corresponding author: Dr Ajili Faida e-mail: faida1977@yahoo.fr
How to cite an article: Ajili F, Bousseta N, Msakni I, Metoui L, Gharsallah I, Laabidi J. Symptomatic macroglossia and tongue myositis in dermatomyositis. Our Dermatol Online. 2013; 4(2): 176-178.
Abstract
The involvement of the tongue in dermatomyositis is rarely described in the literature. We report the case of a patient having a macroglossia whose etiologic was a dermatomyositis. The diagnosis was established by biopsy of the tongue which showed an interstitial lymphocytic infiltration associated with destruction of muscle fibers and perifascicular atrophy. The treatment was based on corticosteroids. The functional prognosis was dominated by the gene to speech and the swallowing disorders.
Key words: macroglossia; tongue myositis; dermatomyositis
Introduction
The macroglossia is observed in certain congenital muscle disease such us Becker’s and Duchenne’s dystrophies or Pompe’s disease. It rarely occurs in polymyositis. We report the case of a symptomatic macroglossia with myositis of the tongue associated with dermatomyositis.
Case Report
A 65 years old man was admitted in our service for macroglossia and macrochely (Fig. 1, 2) associated with a swallowing disorders with false routes and frequent tongue-biting during mastication lasting for a year. He had also an incomprehensible speech and complained of muscle weakness involving the shoulder and pelvic girdles and the limbs. The patient was in a good general condition. Blood pressure was 120/70 mmHg and cardiovascular examination was normal. On physical examination, a slight decrease in muscle strength in all 4 limbs and girdles was noted. He had a significant macroglossia with a falling of the lower lip and a nasal speeech. No skin abnormalities were observed and the neurological examination was strictly normal. The cell blood count was normal and there was no biological inflammatory syndrome. The creatinine phosphokinase (CPK) level was elevated at 606 IU/l and lactate dehydrogenase (LDH) at 416 IU/l. The hepatic and renal function was normal. Electromyography confirmed a diffuse typical myositic process. Muscle biopsy revealed necrotic muscle fibers, regenerating fibers, an endo- and perimysial inflammatory infiltrate and a perifascicular atrophy. The different etiologies of macroglossia have been eliminated by appropriate investigations. Thyroid balance was normal and biopsy of the tongue with congo red staining showed no amyloid deposits. Enzymatic assays were not made in the absence of clinical signs towards genetic myopathies. The biopsy of the tongue showed a phenotype T interstitial inflammatory infiltrate and perifascicular atrophy without neoplastic cells (Fig. 3). The diagnosis of dermatomyositis sine dermatisis revealed by tongue myositis was certain according to the Bohan and Peter criteria. The search for possible neoplasia was negative (thoraco-abdominal scan and tumor markers). The diagnosis of tongue carcinoma has been ruled out by the tongue biopsy. The patient was treated by prednisone at a dose of 1 mg/kg/day associated with methotrexate (20 mg/week) for five years with no improvement of the symptoms. Imunoglobulin infusions were administered so at a dose of 2 g/kg by cure. The patient received six cures spaced by one month. Evolution was marked by the disappearance of the muscular deficit, standardization of CPK and LDH levels, the partial reduction of macroglossia, improvement of speech and the disappearance of false routes. The current decline is of 12 months.
 Figure 1. Macroglossia Figure 2. Machrochely
|
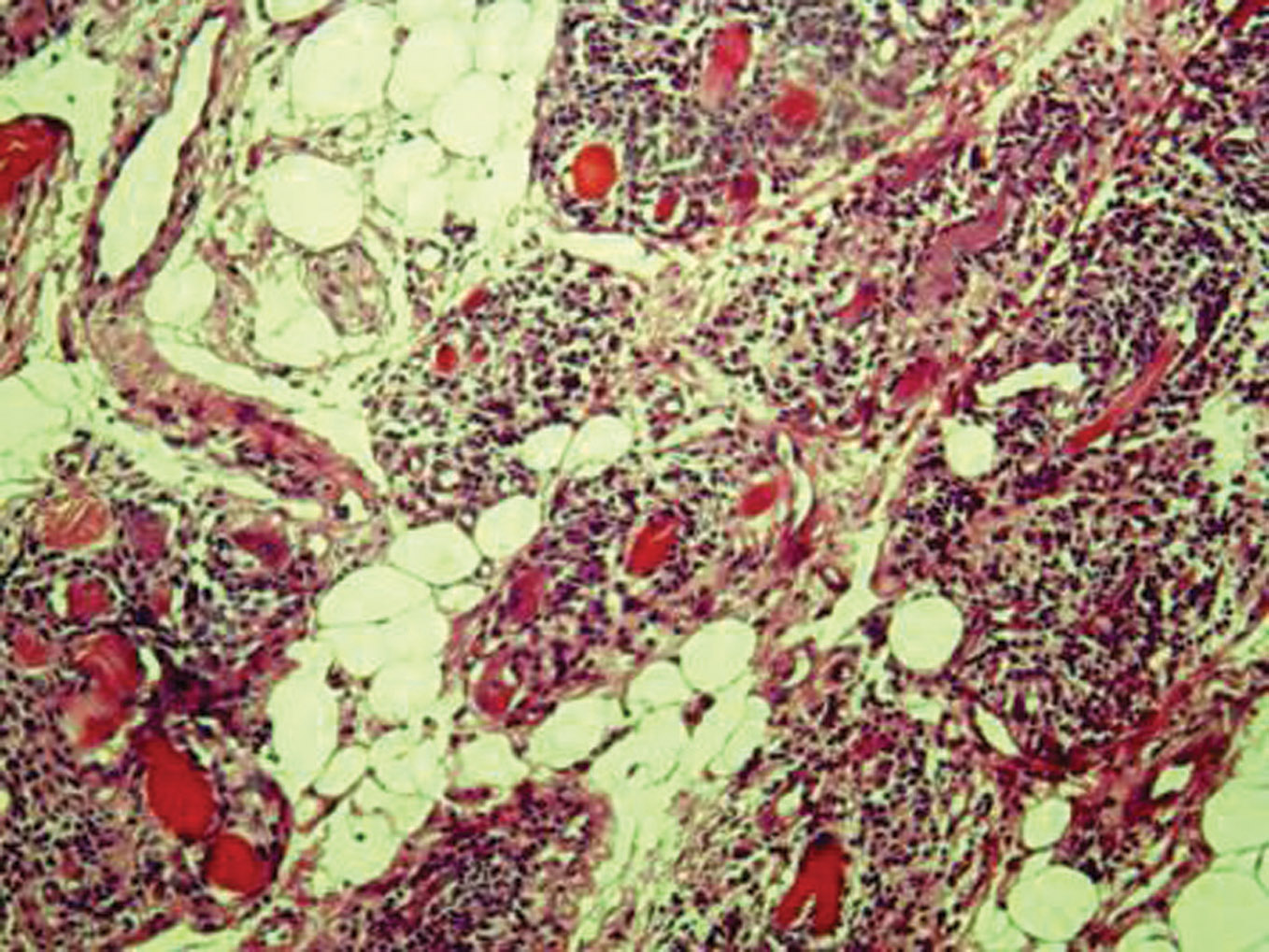 Figure 3. HEX160: The biopsy of the tongue showing a phenotype T interstitial inflammatory infiltrate and perifascicular atrophy without neoplastic cells
|
Discussion
Macroglossia is defined by hypertrophy or hyperplasia of the muscles of the tongue and it is due to congenital or acquired pathologies [1]. It can be observed in several pathologies such us endocrinopathies (hypothyroidism, acromegaly), granulomatoses (Sarcoidosis, crohn’s disease, amyloidosis), genetic syndromes (Myopathies, Mucopolysaccharidoses, glycogen storage diseases, neurofibromatosis) and tumours particularly the tongue carcinoma. The involvement of the tongue in dematomyositis is rare [2-5]. In our patient the diagnosis of dermatomyositis sine dermatisis was certain according to the Bohan and Peter criteria [6]: girdles muscular deficit, the elevation of the CPK level, myositic process in electromyography and perifascicular atrophy in muscle biopsy. In our case the challenge was to link the macoglossia to dermatomyositis and eliminate other causes of tongue hypertrophy. The most common causes of macroglossia (amyloidosis, hypothyroidism, acromegaly) were ruled out. Concerning genetic myopathies (Duchenne’s and Becker’s dystrophies, pompe’s disease), our patient’s age was against these diagnoses. Moreover, the physical examination did not show a waddling walk and difficulty of position change. In addition the biopsy of the tongue did not show dystrophy of the muscle fibers. Other pathology that could simulate a myositis of the tongue and be associated with dermatomyositis is the tongue carcinoma [7-9]. Thus the biopsy of the tongue was necessary to eliminate an eventual neoplasia. In our case,the macroglossia was probably a localization of dermatomyositis because we have noted an improvement of symptoms by corticosteroid treatment associated to immunoglobulin infusions. The magnetic resonance imaging (MRI) of the tongue could help to establish the diagnosis by showing a homogeneous tongue hypertrophy without fat deposits or oedema but the diagnosis is based on the tongue biopsy that showed an inflammatory infiltrate of the lingual parenchyma. The treatment is based on corticosteroid therapy associated with the methotrexate and immunoglobulin infusions relayed by azathioprine in case of resistance to the initial treatment [5]. Thus, our patient demonstrates a rare case of the literature with a real tongue myositis revealing a dermatomyositis. Indeed, a case report similar to ours was published in the literature [5]. It was a 58 years old woman. She had diabetes mellitus and hypertension treated by captopril. She consulted for diffuse myalgia and muscular weakness. The physical examination showed a deficit of pelvic girdles and limbs without skin lesions and a macroglossia. The creatinine phosphokinase (CPK) level was elevated at 2086 IU/l. Electromyography confirmed a diffuse typical myositic process. Muscle biopsy revealed necrotic muscle fibers, regenerating fibers, and an endo- and perimysial inflammatory infiltrate. The diagnosis of polymyositis was retained according to the Bohan and Peter criteria and the patient was treated only by methotrexate at the dose of 10mg/ week with partial improvement. After 6 months the patient reported progressive dysarthria, frequent tongue-biting during mastication, dysphagia, and noisy breathing. The physical examination showed a majoration of macroglossia, a proximal and distal muscular deficit. The CPK level was 1642 IU/l. Captopril-induced angioedema was suspected and the captopril treatment was stopped. Blood α glucosidase activity was normal. The MRI of the tongue showed a homogenous hypertrophy of the tongue and electromyography revealed signs of a diffuse myogenic process. Tongue biopsy was performed and showed a multifocal inflammatory infiltrate with septal and endomysial fibrosis. Congo red staining of tongue, muscle, bone, salivary gland, and skin biopsy specimens showed no evidence of amyloidosis. Immunoglobulin infusions was administered at a dose of 2 g/kg/ cure with a total of six cures and were relayed by azathioprine. In our patient, muscle weakness disappeared by treatment. On the other hand there was a slight improvement of macroglossia and of the speech. These results were similar to the case reported in the literature. Indeed the oropharyngeal symptoms in our patient were probably due to the hypomotility of the tongue caused by myositis and not only due to macroglossia. A surgical reduction of the tongue had been proposed by some authors to improve the functional complications of macroglossia. The glossectomy was the most used technique and consists of making an elliptical incision in the middle of the tongue and a resection at the level of anterior corner, and then sew the sides in a straight line [10]. However the complications were frequent and included a risk of excessive bleeding, airway obstruction due to the tongue oedema, a loss of taste that might occur as a result of damage of the lingual nerve and a lesion of the salivary canal.
Conclusion
Our case illustrates a rare case of the literature of tongue myositis revealing a dermatomyositis. The interest of this observation is to raise the importance of the histological study of tongue biopsy in case of macroglossia whose cause is not obvious.
REFERENCES
1. Willig TN, Paulus J, Lacau-Saint Guily J, Beon C, Navarro J: Swallowing problems in neuromuscular disorders. Arch Phys Med Rehabil. 1994;75:1175–81. 2. Khan AR, Bertorini TE, Horner LH: Tongue involvement in a patient with granulomatous myositis. South Med J. 1997;90:937–9. 3. Sanger RG, Kirby JW: The oral and facial manifestations of dermatomyositis with calcinosis: report of a case. Oral Surg Oral Med Oral Pathol. 1973;35:476–88. 4. Bamanikar S, Mathew M: Focal myositis of the tongue: a pseudotumoral lesion. Histopathology. 1995;26:291–2. 5. Chauvet E, Sailler L, Carreiro M, Paoli JR, Arrue P, Astudillo L: Symptomatic macroglossia and tongue myositis in polymyositis: treatment with corticosteroids and intravenous immunoglobulin. Arthritis Rheum. 2002;46:2762-4. 6. Bohan A, Peter JB: Polymyositis and dermatomyositis. N Engl J Med. 1975;292:344-7. 7. Norris JM Jr, Mustoe TA, Ross JS, Goodman ML: Desmoplastic squamous cell carcinoma of the tongue simulating myositis or fasciitis. Head Neck Surg. 1986;9:51–5. 8. McLendon CL, Levine PA, Mills SE, Black WC: Squamous cell carcinoma masquerading as focal myositis of the tongue. Head Neck. 1989;11:353–7. 9. Sugiyama T, Nakagawa T, Inui M, Tagawa T: Tongue carcinoma in a young patient with dermatomyositis: a case report and review of literature. J Oral Maxillofac Surg. 2001;59:925–8. 10. Wolford LM, Cottrell DA: Diagnosis of macroglossia and indications for reduction glossectomy. Am J Orthod Dentofacial Orthop. 1996;110:170-7.
Comments are closed.