Our Dermatol Online. 2013; 4(2): 185-187
DOI:. 10.7241/ourd.20132.43
Date of submission: 09.02.2013 / acceptance: 22.03.2013
Conflicts of interest: None
POIKILODERMA OF CIVATTE
Uladzimir P. Adaskevich, Maryia A. Katina, Valeryia A. Miadzelets
Department of Dermatovenereology, Vitebsk State Medical University, Vitebsk, Belarus
Corresponding author: Prof. Uladzimir P Adaskevich e-mail: uladas@hotmail.com
How to cite an article: Adaskevich UP, Katina MA, Miadzelets VA. Poikiloderma of Civatte. Our Dermatol Online. 2013; 4(2): 185-187.
Abstract
Poikiloderma of Civatte (Poikilodermia vascularis et pigmentosa Civatte) is a chronic skin condition which refers to the group of melanodermas. Poikiloderma of Civatte (PC) is characterized by erythema associated with atrophy and pigmentation changes of the skin usually seen on the sun exposed areas such as cheeks and sides of the neck. Chronic exposure to ultraviolet light is considered to be an important etiologic factor. We report a 54 years old female patient presenting with confluent, symmetrical reticular dark-brown patches on her face, predominantly on the cheeks, in the preauricular zone, on the forehead and on the front and lateral parts of the neck. Characteristic of the patches are mottled hyper- and hypopigmentation with numerous telangiectasias and areas of atrophy. A biopsy specimen shows epidermal changes including atrophy of the epidermis and hyperkeratosis. Necrotic keratinocytes are found in the papillary dermis as well as occasional lymphocytes extending into the basal layer. The basal damage is associated with dermal involvement. The dermal infiltrate is predominantly lymphocytic. Multiple melanophages, free pigment and edema are seen in the dermis.
Key words: poikoloderma; sun exposure; histology; treatment
Introduction
Poikiloderma of Civatte (Poikilodermia vascularis et pigmentosa Civatte) is a chronic skin condition which refers to the group of melanodermas. The term „poikiloderma” means a skin change with atrophy (thinning), pigmentary changes (either hyperpigmentation or hypopigmentation) and telangiectasia formation (dilatation of fine blood vessels) [1-3]. Poikiloderma of Civatte (PC) is characterized by erythema associated with atrophy and pigmentation changes of the skin usually seen on the sun exposed areas such as cheeks and sides of the neck. The condition was first described by a French dermatologist Civatte in 1923 [1,2]. PC occurs in females more frequently than in males. Female individuals are most commonly affected in the menopausal period [3]. The incidence of PC is unknown; many patients may have a mild form of the disease and may not ask for medical attention. Fair-skinned people are more prone to the disease, although it may be seen in all skin types [1,3]. Some reports point out to clinical and pathomorophological similarity of poikiloderma of Civatte and Riehl’s melanosis. But in the latter case the skin atrophy is less intensive and teleangiectasias are not typical [1,2]. Chronic exposure to ultraviolet light is considered to be an important etiologic factor which is confirmed by the fact that lesions occur on sun-exposed areas. In addition, solar elastosis is a frequent histopathologic finding. Photosensitizing chemicals in perfumes or cosmetics have been implicated in the pathogenesis of poikiloderma of Civatte. Hormonal changes related to menopause or low estrogen levels may also be seen as a possible causative factor. There are some reports suggesting genetic background. The genetically determined predisposition may be expressed in an increased susceptibility of the skin to ultraviolet radiation [1-4]. UV-induced changes of the dermal connective tissue are the predominant histological feature of PC, leading to telangiectasia due to the loss of vascular support. Reticular pigmentation may result from a delayed hypersensitivity reaction to perfume or cosmetic ingredients. The lesions are usually asymptomatic, but some patients may feel mild burning, itching and increased sensitivity in the affected area. The main clinical sign of the disease is a formation of symmetrical reddish-brown patches on the face, lateral parts of the cheeks and sides of the neck, less commonly in the center of the chest. Poikiloderma of Civatte characteristically spares the shaded area under the chin. Reticulate pigmentation with atrophy and telangiectasia is usually present [1-3]. The first and most important step in the management of PC is to avoid sun exposure. Avoiding perfumes and using proper photoprotection are advocated. It is recommended to use a non-irritating sunscreen with SPF at least 50+. The treatment of PC must be directed to the simultaneous elimination of both components, the vascular and the pigmented ones [2,9,10]. Recently, Pulsed Dye Lasers and Intense Pulse Light therapy have been used with favourable results. Intense Pulsed Light systems have a wavelength spectrum of 515-1200nm with high-intensity light sources that emit polychromatic, noncoherent light and, thus, are different from lasers. Several treatment courses may be required for complete clearing [3-8]. Use of fractional photothermolysis (laser technology that creates microthermal injury zones in skin) to treat poikiloderma of Civatte has also been described, with promising results [10]. Attempts to correct the disorder using electrosurgery, cryotherapy, and argon laser have been unsuccessful [3,8]. Topical treatment. Mild topical steroid creams, e.g. hydrocortisone valerate, should be applied for 2-4 months twice a day. Topical retinoids, such as cream Retin A, could be beneficial if used for about a year. Hydroquinonecontaining preparations may help fade the pigmentation Pigment-lightening products, such as topical tretinoin, glycolic acid and hydroquinone, are most often recommended for combined usage.
Case Report
We report a 54 years old female patient, admitted to our clinic with the suspected diagnosis «Discoid lupus erythematosus». She had complaints of the skin affection on the face and neck accompanied by a slight tightening of the skin and a tingling sensation. The first changes of the skin appeared 8 month ago in summer time. The patient noticed deterioration of the skin appearance after sun exposure. After applying of hydrocortisone ointment a slight improvement was seen. The patient had been suffering from euthyroid nodular struma, hysteromyoma for 7 years. Clinical picture. Confluent, symmetrical reticular dark-brown patches were present on the face, predominantly on the cheeks, in the preauricular zone, on the forehead, on the front and on the lateral parts of the neck. Patches showed mottled hyper- and hypopigmentation with numerous telangiectasias with areas of atrophy (Fig. 1, 2). A biopsy specimen shows epidermal changes including atrophy of the epidermis and hyperkeratosis. Necrotic keratinocytes are found in the papillary dermis as well as occasional lymphocytes extending into the basal layer. The basal damage is associated with dermal involvement. The dermal infiltrate is predominantly lymphocytic. Multiple melanophages, free pigment and edema are found in the dermis (Fig. 3).
 Figure 1a, b. Brown patches on the face, neck
|
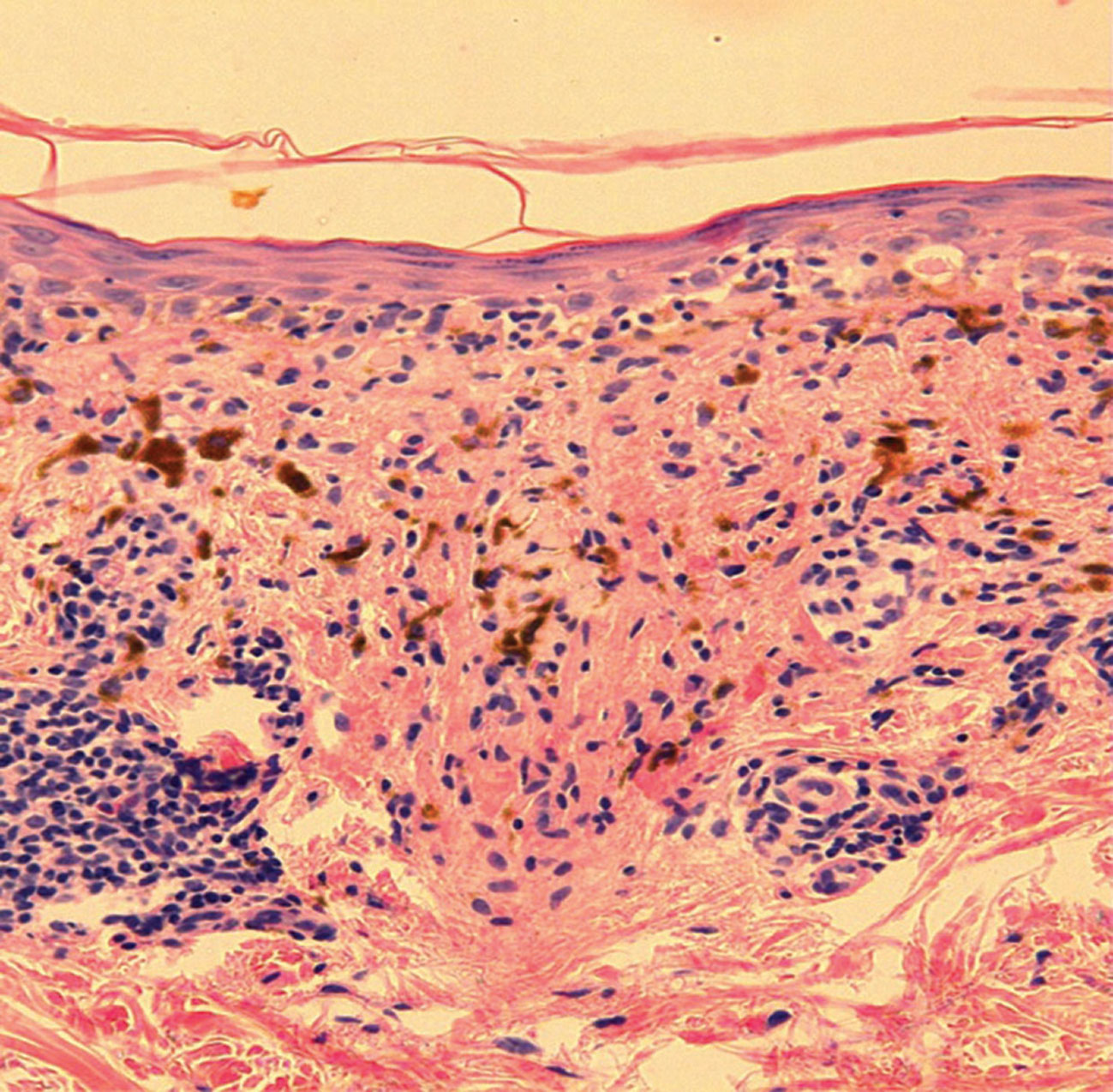 Figure 2. Histological examination
|
Discussion
Poikiloderma of Civatte (PC) although rather common in countries with lighter skin population and a lot of sunshine (e.g. Greece) is a rare condition in moderate climates of East-European countries like Belarus. Hence, the clinical picture of pigment changes suggestive of PC should be differentiated from other poikiloderma conditions in large-plaque parapsoriasis, lupus erythematosus, dermatomyositis, chronic radiation dermatitis, dyskeratosis congenital and rare syndromes, e.g. Bloom syndrome and Rothmund-Thomson syndrome. PC is classified into erythemato-telangiectatic, pigmented and mixed type depending on predominating clinical feature [3]. In our case it was a mixed type with mottled pigmentary changes and a lot of telangiectasias sparing the submental region and the anterior neck which is highly characteristic of PC. The perimenopausal age of the patient was also typical for this condition. Treatment of PC remains challenging [4-10]. Ideally it should combine the elimination of vascular and pigment components simultaneously [3]. Various treatment modalities include lasers, depigmenting agents, topical retinoids and chemical peelings [1,3]. Laser therapy is considered to be the most succsessful, though costly and not consistntly effective [3]. Since treatment of PC remains a challenge all means of photoprotection are fundamentally important. Our patient was recommended to use sunscreen with SPF at least 50+ from March till October; to apply pigment-lightening creams: hydroquinone + tretinoin + hydrocortisone from October till March an to visit a gynecologist and an endocrinologist for corresponding examination.
Recommendations to the patient:
– To use sunscreen with SPF at least 50+ from March till October;
– To apply pigment-lightening creams: hydroquinone + tretinoin + hydrocortisone from October till March
– Examination by a gynecologist and an endocrinologist
REFERENCES
1. Lautenschlager S, Itin PH: Reticulate, patchy and mottled pigmentation of the neck. Acquired forms. Dermatology. 1998;197:291-6. 2. Katoulis AC, Stavrianeas NG, Georgala S, Katsarou-Katsari A, Koumantaki-Mathioudaki E, Antoniou C, et al. Familial cases of poikiloderma of Civatte: genetic implications in its pathogenesis? Clin Exp Dermatol. Sep 1999; 24 (5):385-7. 3. Katoulis AC, Stavrianeas NG, Panayiotides JG, Bozi E, Vamvasakis E, Kalogeromitros D, et al. Poikiloderma of Civatte: a histopathological and ultrastructural study. Dermatology. 2007;214:177-82. 4. Goldman MP, Weiss RA: Treatment of poikiloderma of Civatte on the neck with an intense pulsed light source. Plast Reconstr Surg. 2001;107:1376-81. 5. Weiss RA, Goldman MP, Weiss MA: Treatment of poikiloderma of Civatte with an intense pulsed light source. Dermatol Surg. 2000;26:823-7. 6. Rusciani A, Motta A, Fino P, Menichini G: Treatment of poikiloderma of Civatte using intense pulsed light source: 7 years of experience. Dermatol Surg. 2008;34:314-9. 7. Campolmi P, Bonan P, Cannarozzo G, Bruscino N, Troiano M, Prignano F, et al. Intense pulsed light in the treatment of non-aesthetic facial and neck vascular lesions: report of 85 cases. J Eur Acad Dermatol Venereol. 2011;25:68-73. 8. Meijs MM, Blok FA, de Rie MA: Treatment of poikiloderma of Civatte with the pulsed dye laser: a series of patients with severe depigmentation. J Eur Acad Dermatol Venereol. 2006;20:1248-51. 9. Batta K, Hindson C, Cotterill JA, Foulds IS: Treatment of poikiloderma of Civatte with the potassium titanyl phosphate (KTP) laser. Br J Dermatol. 1999;140:1191-2. 10. Behroozan DS, Goldberg LH, Glaich AS, Dai T, Friedman PM: Fractional photothermolysis for treatment of poikiloderma of Civatte. Dermatol Surg. 2006;32:298-301.
Comments are closed.