Our Dermatol Online. 2012; 3(1): 29-32
Date of submission: 19.08.2011 / acceptance: 21.10.2011
Conflicts of interest: None
MILIARY OSTEOMA CUTIS OF THE FACE
ROZSIANY KOSTNIAK SKÓRY TWARZY
Saadia Bouraoui1, Mona Mlika1, Rim Kort2, Fayka Cherif2, Ahlem Lahmar1, Sabeh Mzabi-Regaya1
1Department of Anatomopathology, El Mongi Slim hospital, Tunis, Tunisia
2Department of Dermatology, Ben Arous hospital, Tunis, Tunisia
Corresponding author: Dr. Mlika Mona e-mail: mlika.zorgati.mona@hotmail.com
Abstract
Introduction: Miliary osteoma cutis (OC) of the face is a rare benign extra skeletal bone formation. For our knowledge, only 23 cases have been reported in the English literature. These lesions may be primary or secondary. They cause diagnostic, therapeutic and cosmetic concern especially in women who are usually concerned. Our purpose is to present a case which is completely documented with the clinical, histological and radiological findings. We also report a possible pathogenic theory according to our histologic findings. Case Report: We report a case of a multiple miliary OC of the face in a 45-year-old woman which suffered from gravidarum acne. These lesions were treated by focal surgical treatment. Conclusions: Based on our histological findings, an osteoblastic metaplasia seems to be a possible pathogenic theory. This metaplasia seems to be secondary to a chronic inflammation. Concerning therapeutic procedures, they are non consensual and debated and are based on surgical or medical treatment. More reports are needed in order to assess the therapeutic management of this disease and its inducing factors.
Streszczenie
Wstęp: Rozsiany kostniak skóry twarzy (KS) to rzadki przypadek pozaszkieletowego kostnienia. Zgodnie z naszą wiedzą, w czasopismach anglojęzycznych opisano do tej pory tylko 23 przypadki. Zmiany tego typu mogą być pierwotne lub wtórne. Powodują one trudności diagnostyczne, terapeutyczne i kosmetyczne – zwłaszcza u kobiet. Celem niniejszej pracy było przedstawienie całkowicie udokumentowanego (pod kątem badań klinicznych, histologicznych i obrazowych) przypadku tego schorzenia (przyp. red.). Informujemy w niej tak?e, na podstawie naszych badań histologicznych, o mo?liwej patogenezie (tego typu zmian-przy. red.). Opis Przypadku: Opisujemy przypadek 45-letniej kobiety z licznymi zmianami rozsianymi typu kostniaków na skórze twarzy, która cierpiała na cię?ką postać trądzika. Zmiany te były leczone za pomocą miejscowych wycięć. Podsumowanie: Na podstawie przeprowadzonych badań histologicznych metaplazja osteoblastyczna wydaje się najbardziej mo?liwą teorią patogenetyczną. Taka metaplazja jest prawdopodobnie wtórna do stanu przewlekłego zapalenia. Wcią? trwają dyskusje nad jednolitymi standardami procedur terapeutycznych, obecne leczenie polega na chirurgicznym wycięciu lub terapii lekami.
Key words: osteoma cutis; face; surgical treatment
Słowa klucze: osteoma cutis; twarz; leczenie chirurgiczne
Introduction
Miliary osteoma cutis (OC) of the face represents a primary extra-skeletal bone formation that arises within the skin of the face. It was first described by Wilekens in 1858 [1]. A few punctual cases have been subsequently reported in order to assess the diagnosis and the treatment of this benign disease which causes cosmetic concern.;
Case Report
We report the case of a 45-year-old woman with skin type III who suffered from gravidarum acne 20 years ago and was addicted to cosmetic products and skin cleansing. She hadn’t a particular gynecologic history, especially no metrorrhagia or endometriosis. No special drug intake was mentioned. She presented in 2003 with multiple and asymptomatic small papular lesions of the brow and the forehead. The lesions have been progressively increased during a 3-year period and achieved the temples. These lesions were as hard as bone. They ulcerate spontaneously secondary to the use of a gomage solution. The patient reported the elimination of rice-like grains. Facial examination revealed numerous skin-coloured papules ranging from 1 to 4 mm, localized on the brow, the forehead and the temples (Fig. 1a). Physical examination didn’t reveal osteo-articular pain or any other abnormalities. Because of the multiplicity of the lesions and the esthetical concern, the patient received initially an inefficient local antiviral treatment due to the suspicion of a verrucous disease. She secondary received a local 0,005% topical retinoin without improvement of the lesions. The diagnoses of cutaneous sarcoidosis and miliary lupus were suspected. In order to assess the diagnosis, a punch biopsy specimen of the largest and the long-lasting lesion was performed and revealed dermal nodules of lamellar mineralized bone. Between the concentrically arranged bone lamellae, medullar spaces contained foci of adipose tissue without hematopoiesis. The bone lamellae were surrounded by a fibrotic tissue without osteoblasts which were seen along the medullar spaces (Fig. 1b). A small nodule, corresponding to a recent lesion, was surrounded by fibroblasts (Fig. 1c). Some of these fibroblasts showed vacuolated nuclei (Fig. 1d). The adjacent dermis didn’t show any inflammation and the epidermis was normal. A CT–scan of the face showed frontal sub-cutaneous hydroxyapatite-containing lesions which were independent from the frontal bone (Fig. 1e,1f). The diagnosis of miliary osteoma cutis of the face was retained. In order to assess its primary or secondary origin, laboratory examinations were performed. They showed normal levels of calcium, inorganic phosphorus, parathyroid hormone and vitamin D. The past medical history of gravidarum acne leads to the diagnosis of a secondary miliary facial osteoma. The patient refused needle microincisions with curettage of the lesions. She underwent a technique consisting in a standard scalpel incisions and excision of the biggest and the most inaesthetical lesions leading to their disappearance without recurrence.
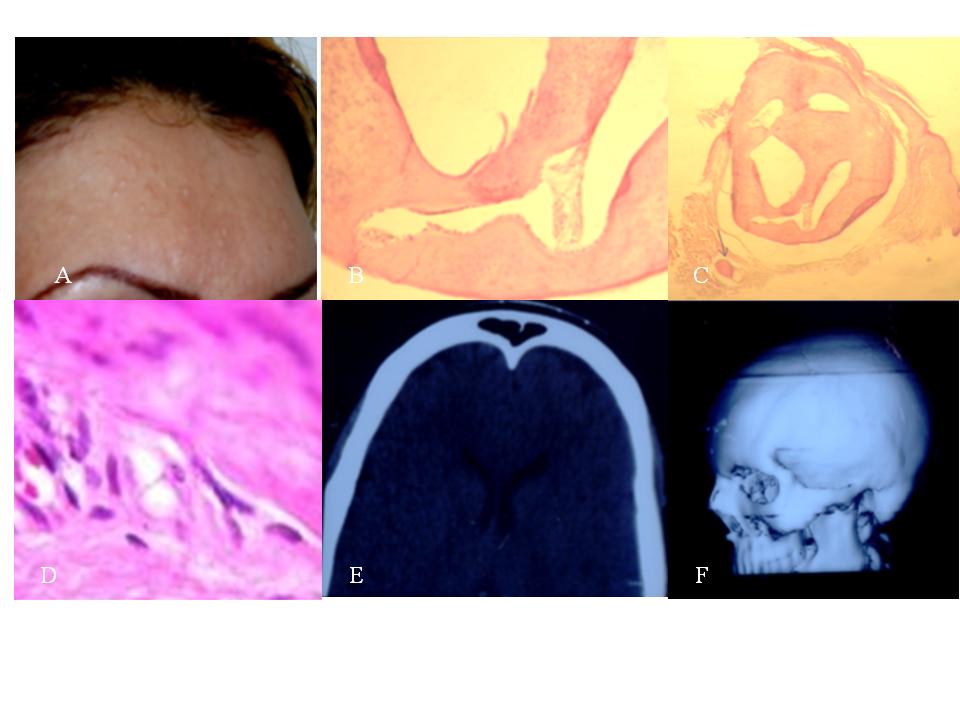 Figure 1. a/ Multiple small bumps on the brow. b/ osteoblasts are seen along the medullary spaces of a bone lesion (HEX400). c/ A small dermal nodule corresponding to a recent osseous lesion associated to a bigger nodule corresponding to a long-lasting lesion (HEX250). d/ Fibroblasts with vacuolated nuclei surrounding an osseous lesion (HEX400). e/ Axial CT-scan showing calcified lesions independent from the frontal bone. f/ Three dimensional CT-scan showing calcified lesions independent from the frontal bone
|
Discussion
Miliary OC of the face is a rare disease with about 23 cases reported in the Pubmed database (Tab. I). These lesions are secondary or primary. Secondary OC may be due to many disorders involving nevi, scleroderma, pilomatricoma, dermatomyositis, basal cell carcinoma, scars, inflammation, trauma, calcification, fibrous proliferations and venous stasis. Primary osteoma can’t be retained unless all the previous causes are excluded [11]. Some authors reported extensive endometriosis, metrorrhagia and osteoarthritis affections in association with this disease [8]. Most cases have been reported in women with no evidence of the implication of the hormonal status. There are 4 main syndromes in which OC can be observed: Albright’s hereditary osteodystrophy, fibrodysplasia ossificans progressive, progressive osseous heteroplasia and plate-like OC [11]. The patient described in our case suffered from gravidarum acne. Her lesions are therefore best characterized as a secondary miliary OC. These lesions are typically asymptomatic and usually appear as skin coloured papules in the scalp, the face as well as the trunk, the breast, the extremities and the buttocks. In cases with chronic acne, the differentiation from microcomedones and macrocomedones may be challenging [17]. In some cases, like in our patient, the diagnosis may be dismissed and the diagnosis of verrucous disease may be suspected. The diagnosis of OC may be suspected by the different size and consistence of the lesions and their radiological appearance but it can be retained only based on histologic examination. Histologic findings consist in a lamellar bone. Osetocytes and osteoblasts are embedded within the bone and are usually best seen along the periphery where mineralized and condensed collagen is still present. Osteoclasts and marrow elements may also be seen but are rare [11]. In our case, the osteoblasts were seen only along the lamellar bone’s medullary spaces, the periphery was fibrotic. The pathogenesis of this disease is mandatory to know in order to prevent its occurrence but it remains debated. Montgomery regarded the osteomas as hamartomas or nervoid tumours [21]. Burgdorf and Nasemann reported two possible processes. One theory assumes a disordered embryologic process, whereby primitive mesenchymal cells differentiate normally into osteoblasts but migrate to the wrong location. However, this remains speculative. The second theory, which appears more plausible and compatible with our histological findings, interprets the presence of bone as a result of osteoblastic metaplasia of mesenchymal cells, such as fibroblasts [22]. Levell reported that a long standing inflammation may cause mesenchymal cells differentiation into osteoblasts [9]. In fact, in our case, the gravidarum acne may have resulted in a fibrous scar and an osteoblastic metaplasia. According to our case, Thielen and coworkers reported an association of miliary osteoma cutis and chronic inflammatory acne [17]. This ultimate scar stage may represent a scarring phase, that’s why no inflammatory lesions are seen. All these phenomenon are documented by the figure n°1C which shows a big ossified lesion surrounded by a fibrotic tissue and corresponding to a long lasting lesion. Below this lesion, a small ossified nodule without surrounding osteoblasts or inflammatory cells is seen. Fibroblasts that are adjacent to this nodule and shown in the figure n°1D have a vacuolated nucleus. This transformation could be interpreted as a stage of osteoblastic metaplasia. This nodule corresponded to a recent lesion. All these histological lesions were secondary to inflammatory lesions. The procedures of treatment of this disease aren’t consensual. Some authors advocate the medical treatments based on topical retinoin which are reported to enable the transepidermal elimination of the bone formation [4,5,23,24]. Several authors reported successful surgical techniques. Ratnavel, Burrows and Pye, used standard scalpel excision to remove multiple miliary cutaneous osteomas [10]. This treatment was used in our case for some biggest and inaesthetical lesions, because of the inefficiency of the medical treatment, and induced their disappearance. Filton used dermabrasion combined with punch biopsies [25]. Dermabrasion was used to improve acne scarring and minimize post operative pigmentary changes. Baskan et al used needle microincision-extirpation method [19]. Oschendorf and Kaufmann used successfully the erbium: YAG laser to ablate the epidermis and upper dermis overlying the cutaneous osteomas [23]. A similar approach using the carbon dioxide laser was employed by Baginskin and Arpey [26]. Recenly, Ayaviri and coworkers reported the efficiency of the association medical and surgical treatment [18].
|
Authors
|
Year of publication
|
Manuscript’s title
|
| Essing M [1] |
1985
|
Osteoma cutis of the forehead
|
|
Schrallhammer K et al [2]
|
1988
|
Primary osteoma cutis
|
|
Collina G et al [3]
|
1991
|
Cellular blue naevus associated with osteoma cutis
|
|
Goldminz D et al [5]
|
1991
|
Multiple miliary osteoma cutis
|
|
Schuhmachers G et al [6]
|
1992
|
Osteoma cutis. Pathogenesis and therapeutic possibilities
|
|
Boehncke WH et al [7]
|
1993
|
Multiple miliary osteoma of the face
|
|
Ward M et al [8]
|
1993
|
Cas pour diagnostic
|
|
Levell NJ [9]
|
1994
|
Multiple papules on the face
|
|
Ratnavell RC [10]
|
1994
|
Osteoma cutis as a sequel of acne
|
|
Altman JF et al [11]
|
2001
|
Treatment of primary miliary osteoma cutis with incision, curettage and primary closure
|
|
Bowman PH et al [12]
|
2001
|
Primary multiple miliary osteoma cutis and exogeneous
ochronosis
|
|
Cohen AD et al [13]
|
2001
|
Treatment of multiple miliary osteoma cutis of the face with
local application of tretinoin: a case report and review of the
literature |
|
Stockel S et al [14]
|
2002
|
Multiple miliary osteomas of the face
|
|
Bergonse FN et al [15]
|
2002
|
Miliary osteoma of the face : a report of 4 cases and review of
the literature |
|
Stanke S et al [16]
|
2003
|
Multiple miliary osteomas of the face
|
|
Thielen AM et al [17]
|
2006
|
Multiple cutaneous osteomas of the face associated with
chronic inflammatory acne |
|
Cohen PR et al [18]
|
2006
|
Isolated primary osteoma cutis of the head : Case report
|
|
Baskan EB et al [19]
|
2007
|
Miliary osteoma cutis of the face: treatment with the needle
microincision-extirpation method |
|
Haro R et al [20]
|
2009
|
Plaque-like osteoma cutis with transepidermal elimination
|
Table I. The different reported cases of miliary osteoma cutis of the face
Conclusion
OC is a rare disease whose pathogenic origin remains debated. According to the past medical history of our patient and the progression of the histological lesions, we can suppose that the chronic inflammatory gravidarum acne induced osteoblastic metaplasia.
REFERENCES
1. Essing M: Osteoma cutis of the forehead. HNO. 1985; 33: 548-590. 2. Schrallhammer K, Landthaler M, Braun-Falco O: Primary osteoma cutis. Hautarzt. 1988; 39: 509-513. 3. Collina G, Annessi G, Di Gregorio C: Cellular blue naevus associated with osteoma cutis. Histopathology. 1991; 19: 473-475. 4. Moritz DL, Elewski B: Pigmented postacne osteoma cutis in a patient treated with minocycline : report and review of the literature. J AM Acad Dermatol. 1991; 24: 851-853. 5. Goldminz D, Greenberg RD: Multiple miliary osteoma cutis. J Am Acad Dermatol. 1991; 24: 878-881. 6. Schulmachers G, Worret WI: Osteoma cutis. Pathogenesis and therapeutic possibilities. Hautarzt. 1992; 43: 422-425. 7. Boehncke WH, Kaufmann R, Weber L, Sterry W: Multiple miliary osteoma of the face. Hautarzt. 1993; 44: 245-247. 8. Ward M, Viraben R: Cas pour diagnostic. Ann Dermatol Venereol. 1993; 120: 713-714. 9. Levell NJ, Lawrence CM: Multiple papules on the face. Arch Dermatol. 1994; 130: 373-374. 10. Ratnavel RC, Burrows NP, Pye RJ: Osteoma cutis as a sequel of acne. J R Soc Med. 1994; 87: 107-109. 11. Altman JF, Nehal KS, Busam KJ, Halpern AC: Treatment of primary miliary osteoma cutis with incision, curettage and primary closure. J Am Acad Dermatol. 2001; 44: 96-99. 12. Bowman PH, Lesher JL: Primary multiple miliary osteoma cutis and exogeneous ochronosis. Cutis. 2001; 68: 103-106. 13. Cohen AD, Chetov T, Cagnano E, Naimer S, Vardy DA: Treatment of multiple miliary osteoma cutis of the face with local application of tretinoin: a case report and review of the literature. J Dermatol Treat. 2001; 12: 171-173. 14. Stockel S, Eppinger S, Stein A, Meurer M: Multiple miliary osteomas of the face. Hautarzt. 2002; 53: 37-41. 15. Bergonse FN, Nico MM, Kavamura MI, Sotto MN: Miliary osteoma of the face: a report of 4 cases and review of the literature. Cutis. 2002; 69: 383-386. 16. Stanke S, Wessling-Assmann K, Metze D: Multiple miliary osteomas of the face. J Dtsch Dermatol Ges. 2003; 1: 131-133. 17. Thielen AM, Stucki L, Braun RP, Masouyé I, Germanier L, Harms M, et al: Multiple cutaneous osteomas of the face associated with chronic inflammatory acne. J Eur Acad Dermatol Venereol. 2006; 20: 321-326. 18. Ayaviri NA, Nahas FX, Barbosa MV, Farah AB, De Arimatéia Mendes J, Ferreira LM: Isolated primary osteoma cutis of the head: Case report. Can J Plast Surg. 2006; 14: 33-36. 19. Baskan EB, Turan H, Tunali S, Toker SC, Adim SB, Bolca N: Miliary osteoma cutis of the face: treatment with the needle microincision-extirpation method. J Dermatolog Treat. 2007; 18: 252-254. 20. Haro R, Revelles JM, Angulo J, Farina Mdel C, Martin L, Requena L: Plaque-like osteoma cutis with transepidermal elimination. J Clin Pathol. 2009; 36: 591- 593. 21. Montgomery H: Dermatopathology, p1131. New York, Paul B. Hoeber, 1967. 22. Burgdorf W, Nasemann T: Cutaneous osteomas: a clinical and histopathologic review. Arch Fur Dermatol Forschung. 1977; 260: 121-135. 23. Ochsendorf FR, Kaufmann R: Erbium: YAG laserassociated treatment of miliary osteoma cutis. Br J dermatol. 1998; 138: 371-372. 24. Smith CG, Glaser DA: Treatment of multiple miliary osteoma cutis with retinoin gel. J Am Acad Dermatol. 1999; 1: 500. 25. Fulton JE: Dermabrasion-loop-punch-excision technique for the treatment of acne-induced osteoma cutis. J Dermatol Surg Oncol. 1987; 13: 655-659. 26. Baginski D, Arpey C: Management of multiple miliary osteoma cutis. Dermatol Surg. 1999; 25: 233-235.
Comments are closed.