Staphylococcal scalded skin syndrome: A case report
Leila Bouhajja 1, Anissa Zaouak1, Ehsen Ben Brahim2, Selima Ben Jannet1, Houda Hammami1, Samy Fenniche1
1, Anissa Zaouak1, Ehsen Ben Brahim2, Selima Ben Jannet1, Houda Hammami1, Samy Fenniche1
1Department of Dermatology, Habib Thameur Hospital, Tunis, Tunisia; 2Department of Pathology, Habib Thameur Hospital, Tunis, Tunisia
Corresponding author: Dr. Leila Bouhajja, E-mail: bouhaja.leila@gmail.com
Submission: 13.09.2018; Acceptance: 01.12.2018
DOI: 10.7241/ourd.20193.11
Cite this article: Bouhajja L, Zaouak A, Brahim EB, Jannet SB, Hammami H, Fenniche S. Staphylococcal scalded skin syndrome: A case report. Our Dermatol Online. 2019;10(3):270-271.
Citation tools:
BibTex | CSV | RIS | refer/BiblX | Endnote XML | Wikipedia Citation Templates
Copyright information
© Our Dermatology Online 2019. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Staphylococcal Scalded Skin Syndrome (SSSS) is an extensive and exfoliative skin disease which is caused by staphylococcal epidermolytic toxin produced by Staphylococcus aureus. A 20-month-old female infant presented with a desquamating rash with flaccid blisters and fever. Skin biopsy revealed superficial intraepidermal cleavage under the stratum corneum. The diagnosis of scalded skin syndrome was assessed and the patient was treated with antistaphylococcal antibiotics with a complete recovery of her skin lesions. SSSS is a pediatric emergency, representing a fatal condition in neonates and a challenge in diagnostic and treatment. Therefore, early diagnosis, prompt treatment, and following strict hygiene measures are imperative and can prevent mortality.
Key words:Scalded skin syndrome, Desquamation, Staphylococcus aureus, Exfoliative toxins
INTRODUCTION
Staphylococcal Scalded Skin Syndrome (SSSS) is an extensive and exfoliative skin disease which is caused by Staphylococcal epidermolytic toxin produced by Staphylococcus aureus. It occurs in newborns, children less than 5 years of life, and adults with various comorbidities [1,2]. We report a new case of SSSS in a 20- month-old female infant.
CASE REPORT
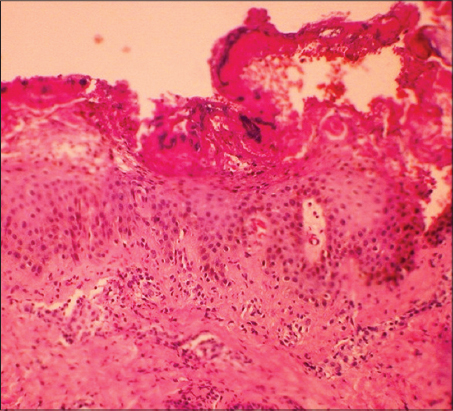
A 20-month-old female infant presented with fever and a generalized rash since 4 days. There was no family history of similar skin lesions. On physical examination, skin was tender with diffuse erythema and she had superficial erosions and peeling on her trunk (Fig. 1). The superficial erosions started on the axillary region extending to the trunk and limbs with sparing of the mucosa. There were flaccid blisters that ruptured leading to superficial erosions with exfoliation. Nikolsky’s sign was positive on the trunk. Other body system examinations were normal. A skin biopsy was performed on her trunk showing superficial intraepidermal split into the granular layer associated with little inflammatory infiltrate in the superficial dermal layer (Fig. 2). Hence, the diagnosis of SSSS was assessed and the patient was treated with antistaphylococcal antibiotics, administred intravenously 100 mg/kg/day for 10 days with a complete recovery of her skin rash.
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure.
DISCUSSION
Staphylococcal scalded skin syndrome (SSSS), also known as Ritter’s disease, is a rare skin infection seen in neonatal period and early childhood as in our patient. It is a potentially life-threatening skin disorder caused by certain strains of staphylococcus aureus that release serine protease exfoliate toxins, exotoxin A (ETA), the most produced one, and the exotoxin B(ETB). These two exfoliative toxins have an affinity to the glycoprotein, desmoglein-1, present on desmosomes located in the zona granulosa layer of the skin, so they cleave desmosomal cadherins, destroy adhesion between the keratinocytes, leading to epidermolysis and bulla formation [1,2]. Moreover, the lack of protective antibodies to exfoliative toxins and immature renal function, explain the higher risk of SSSS in neonates and children. The diagnosis of SSSS is mainly clinical. It usually presents as generalized erythematous extensive skin lesions associated with the formation of large fragile roofed superficial blisters leading to extended areas of eroded skin, bullae, and desquamation with a scalded appearance especially in friction zones, periorificial crusting, and positive Nikolsky sign [3]. This disease may resemble toxic epidermal necrosis which is a life threatening skin disorder. However, in SSSS there is absence of mucosal involvement as well as superficial epidermal peeling with absence of necrotic keratinocytes characteristic of toxic epidermal necrosis. It could also resemble pemphigus foliaceous and bullous impetigo (BI) but in BI, the skin lesions are smaller and there is pronounced inflammatory cell infiltrate consisting mostly in neutrophils and the skin [1,3,4]. A prompt administration of intravenous antibiotics mainly antistaphylococcal penicillins generally allows a favorable outcome [5]. Recovery is achieved after 6 to 12 days without scarring. Prognosis is mostly favorable if treatment is begun promptly, and the mortality rate is 4%, due to serious complications like pneumonia, septic arthritis, hypothermia, dehydration, and secondary infections [4].
CONCLUSION
SSSS is a rare cause of skin infection caused by staphylococcus aureus. It is a pediatric emergency, representing a fatal condition in neonate and a challenge in diagnostic and treatment. Therefore, early diagnosis, prompt treatment, and following strict hygiene measures are imperative and can prevent the mortality.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles. Written informed consent was obtained from the child’s parents for publication of this article.
REFERENCES
1. Handler MZ, Schwartz RA, Staphylococcal scalded skin syndrome: diagnosis and management in children and adultsJ Eur Acad Dermatol Venereol 2014; 28: 1418-23.
2. Meshram GG, Kaur N, Hura KS, Staphylococcal scalded skin syndrome: A pediatric dermatology case reportAGE Open Med Case Rep 2018; 6: 2050313X17750890-
3. Kouakou K, Dainguy ME, Kassi K, Staphylococcal Scalded Skin Syndrome in NeonateCase Rep Dermatol Med 2015; 2015: 901968-
4. Oliveira AR, Aires S, Faria C, Santos E, Staphylococcal scalded skin syndromeBMJ Case Rep 2013 2013; pii: bcr2013009478
5. Jindal S, Bhobhe M, Jerajani H, An infant with skin rashIndian Pediatr 2012; 49: 853-4.
Notes
Source of Support: Nil
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-2062-2256 http://orcid.org/0000-0003-2062-2256
|



Comments are closed.