Our Dermatol Online. 2014; 5(1e): e1
Date of submission: 08.01.2014 / acceptance: 15.01.2014
Conflicts of interest: None
In anticipation of the biopsy. Tumor on the leg
Ahmad Abdulaziz1, Jacek Andruszkiewicz2, Piotr Brzezinski3
1Department of General Surgery, District Hospital, Iława, Poland
2Prof. Francis Łukaszczyk Oncology Center, Clinical Department of Surgical Oncology, Bydgoszcz, Poland
3Department of Dermatology, 6th Military Support Unit, Ustka, Poland
Case Report
We reported 56 years-old woman with skin lesion on the leg since 1,5 years (Fig. 1). This is hard lesion but are bleeding periods and exudation. Occurs big itch of skin lesion and her surroundings.
Point biopsy is not entirely diagnostic (Figure 2 – 4). CK AE1/AE3 (-), S-100 (-), VIM (+) (Fig. 5), CD 68 (+/-).
Initial diagnosis: atypical fibro-xanthoma.
The skin lesion has been cut-out in its entirety. For a full diagnosis is needed full thickness excision with adequate margins.
Suggestions diagnosis: Malignant fibroxystiocytoma, pleomorphic dermal sarcoma.
 Figure 1. Clinical image.
|
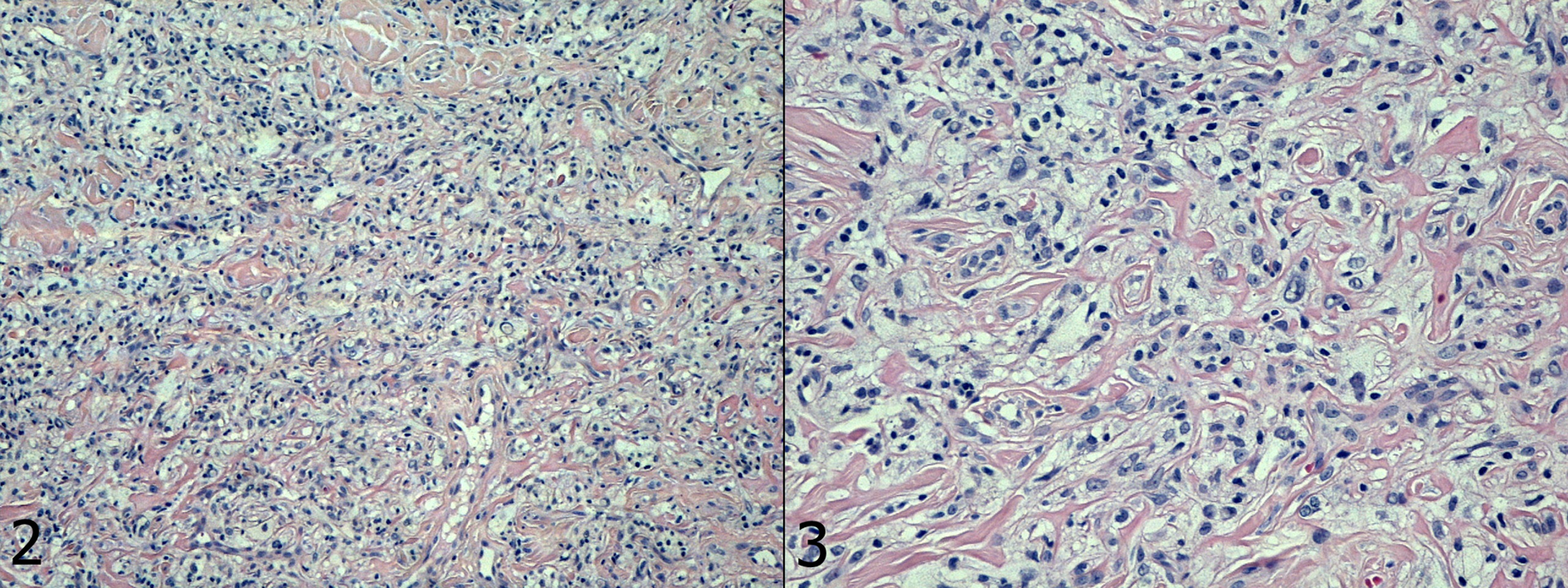 Figures 2, 3. Histopathological image.
|
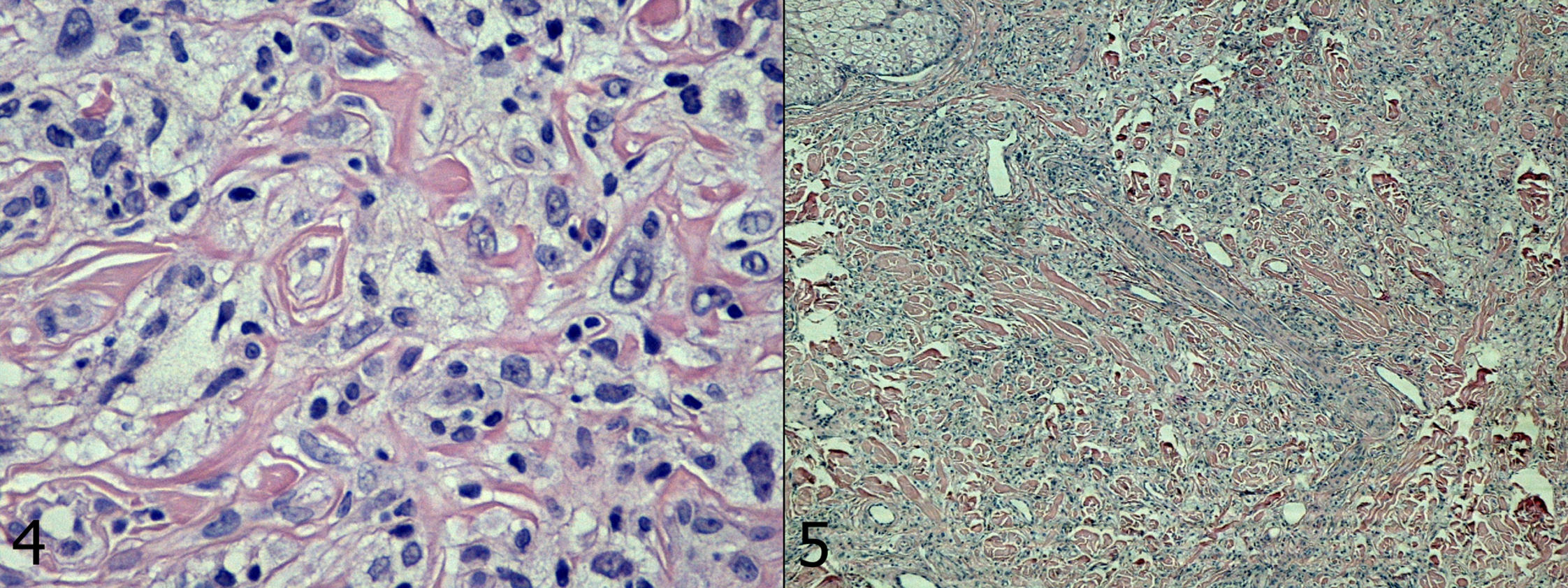 Figures 4, 5. Histopathological image.
|
Discussion
Nonmelanoma skin cancer (NMSC) is the most common form of malignancy in humans. The incidence of NMSC continues to increase despite increased awareness. If neglected or mismanaged, NMSC can cause significant morbidity and even death. The most common forms of NMSC on the head and neck include basal cell carcinoma, squamous cell carcinoma, sebaceous carcinoma, eccrine porocarcinoma, Merkel cell carcinoma, atypical fibroxanthoma, and microcystic adnexal carcinoma. Surgery is the mainstay of treatment (standard excision, Mohs micrographic surgery, curettage); however, other modalities exist, including radiation, topical immunomodulators, photodynamic therapy, and new systemic medications [1-3]. This case emphasises the importance of a diagnostic biopsy.
Atypical fibroxanthoma
Atypical fibroxanthoma (AFX) is an uncommon skin tumour occurring primarily in the head and neck [4]. A panel of immunohistochemical markers is essential to make the correct diagnosis of AFX and distinguish it from malignant fibrohistiocytoma and non-keratin expressing squamous cell carcinoma. It usually follows a benign course, but can occasionally demonstrate aggressive local recurrence as well as distant metastasis. Invasion beyond the dermis and a rapid rate of recurrence are suggestive of a more aggressive clinical course. Weng et al reported of atypical fibrous histiocytoma (AFH) in 24 cases [5]. The tumor occurred in the extremities (number = 14), trunk (number = 8) or head and neck region (number = 2). Apart from one case, all were located in the dermis. The clinical appearance was similar to those of classic fibrous histiocytoma. Histologically, the tumor was characterized by various number of hyperchromatic bizarre cells scattered in the background. Mitotic figures including atypical ones were noted, especially in the more cellular areas. Immunohistochemical study showed that the tumor cells expressed vimentin. Atypical fibrous histiocytoma represents a pleomorphic variant of fibrous histiocytoma. Although the tumor exhibits worrisome features, it usually pursuits a relatively benign course. Nevertheless, rare cases may recur, especially after incomplete excision. AFH is sometimes mistaken as atypical fibroxanthoma. A distinction between the two entities is warranted as they represent two different entities. Authors from USA described an 18-year-old woman with Li- Fraumeni syndrome who developed an atypical fibroxanthoma (AFX) on her left arm [6]. This tumor was based in the dermis, sparsely cellular and had ill-defined borders. It was composed predominantly of medium-sized spindled-shaped cells, but many large cells with pleomorphic nuclei were also present. Immunohistochemical stains showed that the tumor cells lacked expression of keratin, S-100 protein, desmin and CD34. This represents one of a few reports of a cutaneous tumor in a patient with LFS and a rare example of an AFX occurring at a young age.
Pleomorphic dermal sarcoma
The behavior of atypical fibroxanthoma is benign, if strict diagnostic criteria are applied. Tumors with similar pathologic features but deep subcutaneous invasion, necrosis, and/ or lymphovascular or perineural invasion are thought to be associated with adverse outcome and are better regarded as pleomorphic dermal sarcoma or undifferentiated pleomorphic sarcoma of skin. This tumor group is not well documented in the literature, and its characteristics are only poorly defined. The tumors are large (median: 25 mm) and exclusively present on sun-damaged skin with a strong predilection for the head. Typically, elderly men were affected (median age: 81 y). Histologically, these often ulcerated tumors are poorly marginated, asymmetrical, and deeply invasive into deep subcutaneous, muscular, and/or fascial tissues. The tumors are cellular and composed of pleomorphic epithelioid cells, atypical spindle cells, and multinucleated tumor giant cells in varying proportions. The majority of tumors show a predominance of atypical spindle cells in a fascicular arrangement [7]. Atypical fibroxanthoma and pleomorphic dermal sarcoma (DS) may be difficult to separate from cutaneous angiosarcoma. Atypical fibroxanthomas are nodular and confined to the dermis. Thum, et al described AFX and DS [8]. All tumors were composed of pleomorphic epithelioid and spindle cells showing blood-filled spaces and intratumoral hemorrhage. Intracytoplasmic vacuoles (n = 4), hemosiderin deposition (n = 2), and keloidal stromal change (n = 1) were also noted. Immunohistochemically, CD31 was expressed in 43% of cases, FLI1 in 79% and smooth muscle actin in 50%. Staining for CD34, ERG, S100, HMB-45, desmin, p63 and cytokeratins was negative. Follow up (median, 43.1 months; range 1-100), available for 10 patients, showed no adverse outcome. Pseudoangiomatous features and aberrant expression of CD31 and FLI1 in atypical fibroxanthoma and pleomorphic dermal sarcoma may lead to an erroneous diagnosis of cutaneous angiosarcoma. Negativity for CD34 and ERG, in particular, is a reliable differentiating feature in this setting.
Malignant fibrohistiocytoma
Malignant fibrohistiocytoma (MFH) is an infrequent neoplasm that may arise in any body region, though it is generally found in the limbs (particularly the legs) and abdomen (retroperitoneum). MFH tends to develop in the skin in the form of small, slow-growing nodules, though its behaviour is more aggressive when the lesions are located in deep-lying tissues. While the histological origin is unclear, it has been postulated that the tumor derives from histiocytes that morphologically [9]. Yamamoto et al described a case a 77-year-old male with swelling of his right leg [10]. Physical examination revealed an ill-defined mass at RLQ. Computed tomography (CT) and 3 dimensional CT showed an 8-cm tumor on the IVC, partially replacing iliac vessels and invading the psoas muscle. A diagnosis of malignant fibrohistiocytoma was made by pathological examination of biopsied specimens at exploratory laparotomy. The term ‚fibrohistiocytic’ tumour is a descriptive designation without histogenetic connotation for a group of heterogeneous lesions that share morphological features of histiocytes and fibroblasts on light microscopy. However, over the years it has become apparent that many so-called ‚fibrohistiocytic’ tumours are largely composed of relatively undifferentiated mesenchymal cells, but can also show areas of myofibroblastic differentiation [10].
Acknowledgement
Prof Bostjan Luzar MD, PhD
Institute of Pathology, Medical Faculty University of Ljubljana,
Korytkova 2, 1000 Ljubljana, Sloveniaa
References
1. Dubas LE, Ingraffea A. Nonmelanoma skin cancer. Facial Plast Surg Clin North Am. 2013;21:43-53.
2. Hassan I, Dorjay K, Sami A, Anwar P. Sunscreens and Antioxidants as Photo-protective Measures: An update. Our Dermatol Online. 2013;4:369-74.
3. Orsaria M, Mariuzzi L. Recurrent eccrine hidradenoma of the breast in a male patient: problems in differential diagnosis. Our Dermatol Online 2013; 4(2): 215-217.
4. Rathore D, Mohyudin MN, Mehta P, Ahluwalia HS. Atypical fibroxanthoma of the medial canthus: a rare presentation. Orbit. 2013;32:194-6.
5. Weng WW, Yang J, Wang J. [Atypical fibrous histiocytoma: a clinicopathologic analysis of 24 cases]. Zhonghua Bing Li Xue Za Zhi. 2013;42:316-20.
6. Lee SM, Zhang W, Fernandez MP. Atypical fibroxanthoma arising in a young patient with Li-Fraumeni syndrome. J Cutan Pathol. 2013 Dec 2.
7. Luzar B, Calonje E. Cutaneous fibrohistiocytic tumours – an update. Histopathology. 2010;56:148-65.
8. Thum C, Husain EA, Mulholland K, Hornick JL, Brenn T. Atypical fibroxanthoma with pseudoangiomatous features: a histological and immunohistochemical mimic of cutaneous angiosarcoma. Ann Diagn Pathol. 2013;17:502-7.
9. Miller K, Goodlad JR, Brenn T. Pleomorphic dermal sarcoma: adverse histologic features predict aggressive behavior and allow distinction from atypical fibroxanthoma. Am J Surg Pathol. 2012;36:1317-26.
10. Yamamoto Y, Goto M, Okamoto T, Tomita I, Murayama A, Sawa M, et al. [Chemotherapy-naïve advanced malignant fibrohistiocytoma presenting IVC syndrome case report]. Gan To Kagaku Ryoho. 2010;37:355-7.
Comments are closed.