A rare case of atrophoderma with papules
Yeşim Akpinar1, Evren Sarifakioiglu2
1Department of Dermatology, Ufuk University, Ankara, Turkey, 2Private Dermatology Clinic, Ankara, Turkey
Corresponding author: Dr Yeşim Akpinar, E-mail: yesim_akpinar@yahoo.com
Submission: 16.06.2017; Acceptance: 29.06.2017
DOI: 10.7241/ourd.2017e.10
How to cite this article: Akpinar Y, Sarifakioglu E. A rare case of atrophoderma with papules. Our Dermatol Online. 2017;8(2e):e1.
ABSTRACT
Atrophoderma of Pasini and Pierini (APP) is a rare and etiologically unknown form of dermal atrophy. Generally they were characterized as ovally or round shaped, sharply demarcated, hyperpigmented patches (i.e., the "cliff-drop" borders). These patches are usually located in the trunk in addition to upper and lower extremities. It commonly occurs in second or third decades of life, with women more than men. In this study, we discussed about a case who had the nonclassical form of APP with the initial lesions as papules.
Key words: Atrophoderma Pasini and Pierini, inflamation, lineer atrophoderma of Moulin
INTRODUCTION
Atrophoderma of Pasini and Pierini (APP) is a rare dermatosis characterized by well-defined atrophic plaques [1]. It is more common in young adults and women [2]. Linear atrophoderma of Moulin (LAM) is an acquired unilateral, depressed plaque following the lines of Blaschko. It affects usually children or adolescents. Baumann et al.considered LAM is a variant of progressive idiopathic atrophoderma of Pasini and Pierini [3]. Herein,we present a case of atrophoderma which started with papules.
CASE REPORT
Twenty-nine-year-old female patient was admitted to our clinic due to resident brown-gray spots on the buttock and both thighs. It was learned from the story that her complaints started as small, numerous bumps without tips in her buttock about 8 months ago, that these bumps were also occured for the first time on her nipple 2 days ago, then they were healed with hyperpimentation and she did not receive any medical treatment in the past. There was no history of trauma, infection, or insect bites before.
Complete blood count, erythrocyte sedimentation rate, liver and kidney function tests, ANA and Anti-DNA were within normal limits in laboratory tests. The Borrelia Burgdorferi antibody was negative (-).
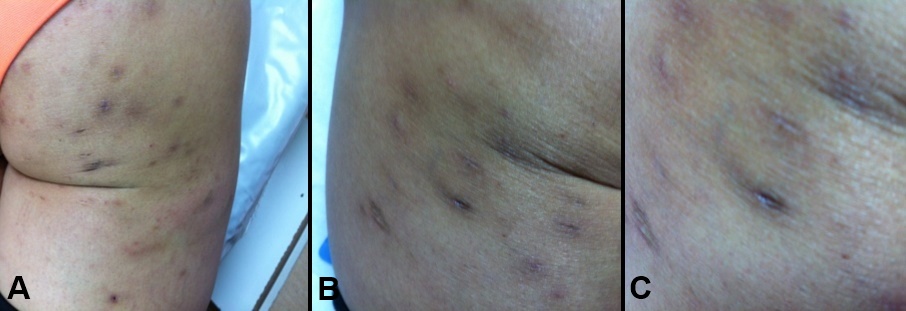
On dermatological examination, bilateral and erythematous papules on the buttock and thigh region and numerous, round, sharp, limited depressed plaques were detected. The lesions were brown-gray color and the central atrophic appearance of the plaques. No induration or sclerosis was detected in the lesions (Figs. 1a – 1c).
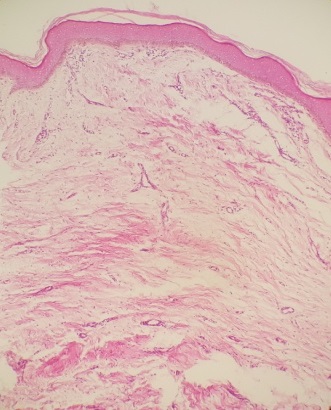
Histopathological examination of atrophic pigmented plaques showed that thickening of the basal layer and increased melanin pigmentation, flattening of dermal papillae and mild perivascular lymphocytic infiltration (Fig. 2).
The patient was diagnosed with 'Atrophoderma of Pasini and Pierini' consideration with clinical and pathological findings. Local corticosteroid cream therapy was initiated for the atrophic plaques on the buttock and thighs with 100 mg doxycycline/daily for the cause of inflammatory papules. There was no regression in the papules at the end of two weeks of antibiotic treatment. Corticosteroid cream therapy was stopped at the end of two months due to no changes.
DISCUSSION
The Atrophoderma of Pasini and Pierini (APP) was first described by Pasini in 1923 [4]. Pierini and Vivoli suggested that in 1936 it may be associated with morphea, Yokoyama and colleagues suggested that the atrophy is different from the classical morphea of skin glycosaminoglycans [5]. Sharply and well shaped (cliff-drop), brown-gray depressed plaques are typical for Atrophoderma [6]. Lesions are symmetrically located in the body, usually in the back and lumbosacral region. Hand, foot and upper extremity involvement is very rare [1]. In some patients, zosteriform distribution was reported in parallel to the skin folds. It is thought that the general course of the disease lasts for as long as 10-20 years and there is no involution [1].
The etiopathogenesis is not known [5]. Previous studies have reported that genetic, neurogenic factors as well as defects in dermatan sulfate metabolism may cause this disease [2]. Direct immunofluorescence studies have focused on immunologic factors due to accumulation of IgM and C3 in small blood vessels and the detection of T lymphocytes and macrophages between the perivascular region and collagen fibers in the electron microscope [7].
It is thought that the disease does not have a current effective treatment.Antibiotic therapy has been recommended in cases of Borrelia antibody titer positive [8,9]. Treatment with systemic steroids, antimalarials, calcitriol and phototherapy have been tried in sclerotic cases [10]. In current treatment approaches, Q-switched lasers for hyperpigmentation treatment are used in patients with cosmetic concern [2,3].
Histopathology is usually not diagnostic [5]. Early lesions have moderate chronic inflammatory cells. This finding is not seen in the late period. Pigment enhancement can be seen in the basal layer [5]. Skin attachments are usually protected.
Based on clinical and histopathological findings in the present case, it is thought to be compatible with Atrofodermia Pasini and Pierini. The initial complaints of our case are inflammatory features such as papules which are not compatible with the classical Atrophoderma clinic. For this reason, inflammatory lesions such as dermatitis cruris pustulosa et artophicans and keratosis folicularis decalvans, and other atrophic diseases are considered to be distinctive. However, the lesions in dermatitis cruris pustulosa are usually found in the form of pustules and in the lower extremity region, in the keratosis folicularis decalvans, as clinical findings that start with more erythematous papules and result in hairy deep cicatricial alopecia [11,12]. The other two diseases were excluded with clinical and histopathological findings.
In the differential diagnosis, two Moulin's atrophodema (LAM) cases were encountered, starting with inflammatory papules defined by Browne and Fisher [10]. The authors suggested that this disease has inflammatory and non-inflammatory variants. Pasini and Pierini stated that there may be variants of the same disease due to the clinical and histopathological similarity of LAM with atrophoderma. In another case report of Moulin’s lineer atrophy, pigmentation and atrophy with 20 mg / week methotrexate were reported to decrease successfully for 6 months. Because of the efficacy of methotrexate, LAM, APP, and linear scleroderma are thought to be other variants of the same disease. There are hyperpigmented atrophic plaques in the LAM, just as in APP, which are usually located on the trunk and extremities. But these plaques are parallel to the Blaschko lines in LAM. The age of onset is between 5 and 20[9]. As in the case of LAM, which started in the literature as inflammatory papules, but developed by atrophic plaques following Blaschko lines, we think of LAM in our patient which first started with inflammation. However, we did not consider this diagnosis because the age of onset was advanced with respect to LAM and the location of the lesions did not match the Blaschko lines. We also think that it is a different type of APP which initiated with inflammatory lesions and it is transitional forms of LAM and APP.
CONCLUSION
When we review the literature, there are no cases of Atrophoderma of Pasini and Pierini starting with papules and nodules, as in our case, although there are case reports of zosteriform, linear and morpha-related or paraneoplastic Atrophoderma.
REFERENCES
2. Zhang RZ, Zhu WY. Two uncommon cases of idiopathic atrophoderma of pasini and pierini:multiple and giant. Indian J Dermatol Venereol Leprol. 2011;77:402
3. Tukenmez Demirci G, Altunay IK, Mertoglu E, Kucukunal A, Sak?z D. Linear atrophoderma Of Moulin on the neck. J Dermatol Case Rep. 2011;5:47-9.
4. Avancini J, Valente NY, Romiti R. Generalized lenticuler atrophoderma of Pasini and Pierini. Pediatr Dermatol. 2015;32:389-91.
5. Garg A, Kumar P. Atrophoderma of Pasini and Pierini. Indian Dermatol Online J. 2011;2:126-8.
6. Ravic-Nicolic A, Djurdjevic P, Mitrovic S, Milicic V, Petrovic D. Atrophoderma of Pasini and Pierini associated with extramedullary plasmacytoma. Clin Exp Dermatol. 2016;41:837-9
7. Yan W, Wang S, Liu HJ, Wang L, Li W, Ran YP, Zhang M. Linear atrophoderma of Moulin:a disease related to immunity or a kind of connective tissue disease? Australas J Dermatol. 2016 Jun 10.
8. Buechner SA, Rufli T. Atrophoderma of Pasini and Pierini.Clinical and histopathologic findings and antibodies to Borrelia burgdorferi in thirty-four patients. J Am Acad Dermatol. 1994;30:441-6.
9. Tan SK, Tay YK. Linear atrophoderma of Moulin. JAAD Case Rep. 2016;2:10-2.
10. Zahedi Niaki O, Sissons W, Nguyen VH, Zargham R, Jafarian F. Linear atrophoderma of Moulin:underrecognized entity. Pediatr Rheumatol Online J. 2015;13:39.
11. Bens G, Franck F, Diatto G, Preney L, Darie H, Geniaux M. Dermatitis cruris pustulosa et atrophicans a frequent but poorly understood tropical skin condition- case report from Burkina Faso. Int J Dermatol. 2008;47:473-5.
12. Verma R, Bhatnagar A, Vasudevan B, Kumar S. Keratosis follicularis spinulosa decalvans. Indian J Dermatol Venereol Leprol. 2016;82:214-6.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Comments are closed.