A pinkish nodule on the vertex: What’s your diagnosis?
Mohamed Ben Rejeb 1, Yosra Soua1, Nouha Abdejlil2, Monia Youssef1
1, Yosra Soua1, Nouha Abdejlil2, Monia Youssef1
1Department of Dermatology, Fattouma Bourguiba University Hospital, Monastir-Tunisia; 2Department of Anapathology, Fattouma Bourguiba University Hospital, Monastir-Tunisia
Corresponding author: Dr. Mohamed Ben Rejeb, E-mail: med.benrejeb@gmail.com
Submission: 29.12.2019; Acceptance: 10.01.2020
DOI: 10.7241/ourd.2020e.5
Cite this article: Rejeb MB, Soua Y, Abdejlil N, Youssef M. A pinkish nodule on the vertex: What’s your diagnosis? Our Dermatol Online. 2020;11(e):e5.1-e5.2.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
CASE REPORT
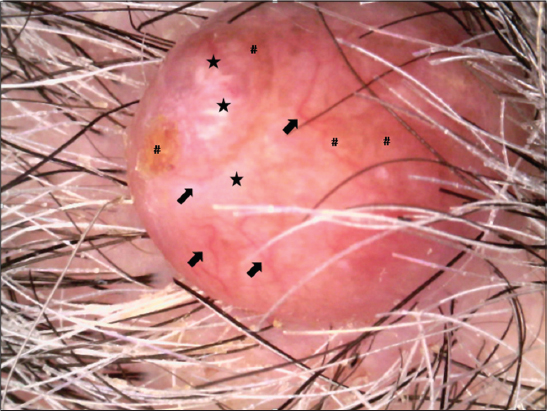
A 71-year-old man presented to our dermatology department with a slightly painful nodular lesion over the scalp for 1 year. The size of the nodule had gradually increased recently. He had no personal or family history of skin disease or other systemic disorders. Cutaneous examination showed well-circumscribed and tender sessile pinkish nodule measuring 2 cm over the vertex of the scalp (Fig. 1). It was firm in consistency and we noticed an infiltrated area surrounding the lesion. Dermoscopic examination showed a well-defined nodule composed of white structures, pinkish and yellowish homogeneous areas, linear irregular vessels and arborizing telangiectasias (Figs. 2 and 3). The lesion was completely excised.
HISTOLPATHOLOGY
Histopathological examination showed well-circumscribed intradermal tumor with a lobular arrangement of uniform and clear cells, ductal structures, and cystic spaces (Figs. 4 and 5).
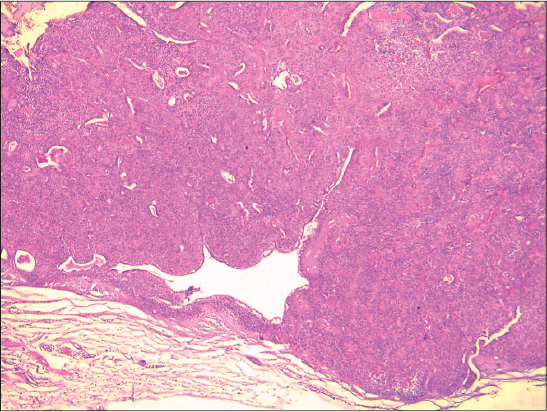 |
Figure 4. Low-power view of a circumscribed dermal tumor nodule Hex40. |
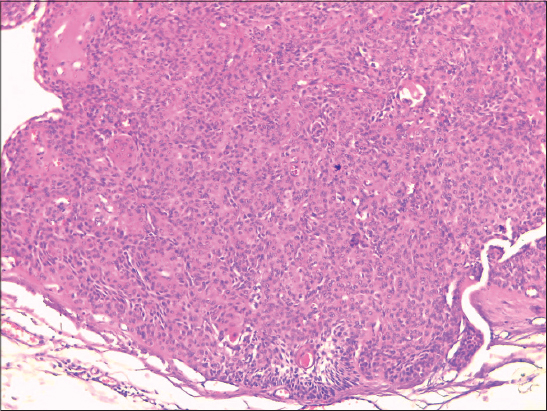 |
Figure 5. High-power view showing uniform cells with eosinophilic cytoplasm admixed with few clear cells HEx100. |
WHAT’S YOUR DIAGNOSIS?
Answer: Nodular Hidradenoma
Nodular Hidradenoma (NH) is a rare benign adnexal neoplasm of either eccrine or apocrine differentiation from sweat glands that is commoner in adults than in children [1,2]. It’s a challenging diagnosis because of clinical heterogeneity. NH is more commonly seen in women with an average age of 30 to 40 years. The most common site is the head [3]. Clinically, NH usually presents as a solitary slow-growing pinkish nodule which is well-circumscribed, firm, non-tender and involving the scalp, neck, trunk, and extremities [4]. Dermoscopy can be useful. Dermoscopic features include pinkish or bluish homogeneous areas with vascular and white structures [5]. Histological examination confirmed the diagnosis by showing a circumscribed but unencapsulated tumor composed of lobulated and cystic masses of cells mainly located in the upper or mid dermis [3]. The best treatment for NH is surgical excision. Although NH is a benign skin lesion, long term follow-up of patients is required to detect possible recurrence that may be transformed to malignant NH [6].
References
1. Juan Carlos RM, Sylvia Aide MC, Alejandra VM, Ana Sof?a AC, Ivette MM, et al. Nodular hidradenoma: Dermoscopic presentation. J Am Acad Dermatol. 2017;76:S46-8.
2. Nasit JG, Dhruva G. Nodular hidradenoma of the scalp: A cytomorphologicalevaluation on fine needle aspiration cytology. Indian J Dermatol Venereol Leprol. 2014;80:569-72.
3. Abdulla AB, Suresh SR and Maragaret AR. Malignant nodular hidradenoma of the eyelid: a rare sweat gland tumor. Middle East Afr J Ophthalmol. 2010;17:374–6.
4. Kataria SP, Singh G, Batra A, Kumar S, Kumar V, Singh P. Nodular hidradenoma: aseries of five cases in male subjects and review of literature. Adv Cytol Pathol. 2018;3:46-7.
5. Patricia S, Aimilios L, Luis Javier DP, Isil K, Carolina M, et al. Dermoscopy of nodular hidradenoma, a great masquerader: a morphologicalstudy of 28 cases. Dermatology. 2016;232:78-82.
6. Nhuan N, Michiro S, Takahiro N, Yo K, Chiaki S, et al. Malignant transformation of nodular hidradenoma in the lower leg. Case Rep Oncol. 2018;11:298-304.
Notes
Source of Support: Nil
Conflict of Interest: None
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|





Comments are closed.