Histopathological examination and evaluation of serum vitamin D levels in alopecia-is it necessary?
Romita Bachaspatimayum 1, N.A. Bishurul Hafi2, Bipin Thingujam3
1, N.A. Bishurul Hafi2, Bipin Thingujam3
1Department of Dermatology, Venereology and Leprosy, RIMS, Imphal, Manipur, India, 2Department of Dermatology, Venereology and Leprosy, Iqraa International Hospital and Research Institute, Kozhikkode, Kerala, 3Consultant Pathologist, Babina Diagnostics, Imphal, Manipur, India
Corresponding author: Dr. Romita Bachaspatimayum
Submission: 11.06.2020; Acceptance: 25.08.2020
DOI: 10.7241/ourd.2020e.153
Cite this article: Bachaspatimayum R, NA Bishurul Hafi, Thingujam B. Histopathological examination and evaluation of serum vitamin D levels in alopecia-is it necessary? Our Dermatol Online. 2020;11(e):e153.1-e153.3.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Alopecia or hair loss may be of several types depending upon various etiological factors. Clinical and histopathological lapses have been encountered. Vitamin D has been found to have a role in the etiopathogenesis of alopecia. With this background, the study was undertaken to corroborate the histopathological and the clinical diagnosis and to find out the association between vitamin D levels and alopecia.
Material and Methods: All patients of alopecia, attending out-patient Department of Dermatology in a tertiary care centre who were willing to participate were included while those due to infective causes or with incomplete reports were excluded from the prospective study of two years (January 2015-December 2016). Histopathological examination of skin biopsy was done and corroborated with the clinical diagnosis along with measurement of serum vitamin D levels by electrochemiluminescense immunoassay (ECLIA). Data was analyzed by spss20v; Fischer’s Exact test was used and a p value of 0.05 was taken as significant.
Results: Out of total 50 patients, 20 (male:female=1.5:1) patients had both HPE and serum vitamin D reports and their results were analyzed. HPE and clinical diagnosis matched in only 10 patients (50%) with a significant p-value (p=0.007; p<0.05). Sufficient levels (>/= 30 ng/ml ) of serum vitamin D were found in only three (15%) with p value >0.05 (0.421) which was not significant.
Conclusion: H.P.E. finding was significantly variable compared to clinical diagnosis. Hence, we should opt for a confirmatory skin biopsy wherever feasible. Evaluation of vitamin D is suggested with studies on a larger scale.
Key words: Alopecia; Skin biopsy; Vitamin D
INTRODUCTION
Alopecia may be of several types depending upon etiological factors. Lapses between clinical and histopathological diagnosis have been encountered. Alopecia usually can be correctly and rapidly diagnosed from the presentation and course of hair loss though a biopsy may sometimes be necessary for a definitive diagnosis to be made [1,2]. The histopathological interpretation of scalp biopsy may represent a challenging task in the absence of a good, definitive clinical history, adequate tissue sampling and appropriate grossing technique [3]. Vitamin D has been found to have a role in the etiopathogenesis of alopecias. Vitamin D deficiency has been incriminated in various skin disorders including hair loss [4].
Aims and Objects
The study was undertaken taken to corroborate the histopathological examination (H.P.E) and clinical diagnosis and to find out the association between vitamin D levels and alopecia.
MATERIAL AND METHODS
All patients of alopecia, attending out-patient Department of Dermatology in a tertiary care centre, of all age groups who were willing to participate were included while those due to infective causes or with incomplete reports were excluded from the prospective study of two years (January 2015-December 2016). Informed written consent was taken from all the patients and from the guardians if the patient was below 18 years of age. Histopathological examination of skin biopsy was done and corroborated with the clinical diagnosis along with measurement of serum vitamin D levels by electrochemiluminescense immunoassay (ECLIA). Two skin biopsy samples were taken by 4mm punches for horizontal and vertical sectioning. Measurement of serum 25 OH vitamin D was done by electrochemiluminescense immunoassay (ECLIA) and was interpreted as : deficiency <30 ng/ml, sufficiency >/=30-100 ng/ml, toxicity > 100 ng/ml. Data was analyzed by spss20v; Fischer’s Exact test was used and a p value of 0.05 was taken as significant.
RESULTS
Out of total 50 patients, 20 (male:female=1.5:1) patients had both HPE and serum vitamin D reports and their results were analyzed. The most common age group was 21-30 years (n=8; 40%). Most common clinical diagnosis was alopecia areata, AA (n=12; 60%) followed by chronic telogen effluvium, CTE. HPE and clinical diagnosis matched in only 10 patients (50%) with trichotillomania, lupus profundus, actinic keratosis and non-specific findings being reported in HPE of AA (n=1 each; 5% each). H.P.E. findings were significantly variable compared to clinical diagnosis (p=0.007; p<0.05) (Table 1a and Table 1b). Sufficient levels (>/= 30 ng/ml ) of serum vitamin D were found in only three (15%) patients (2-AA;1-PHL) with p value >0.05 (0.421) which was not significant (Table 2).
 |
Table 1a: Corroboration of clinical and HPE diagnosis |
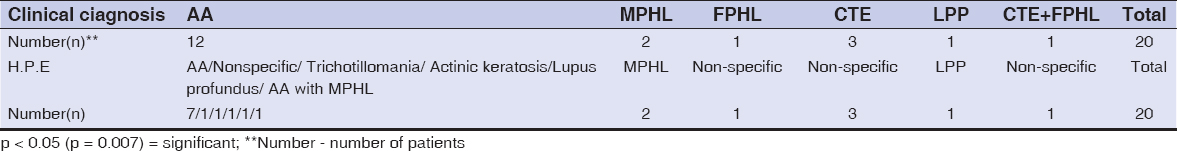 |
Table 1b. Corroboration of clinical and histopathological diagnosis |
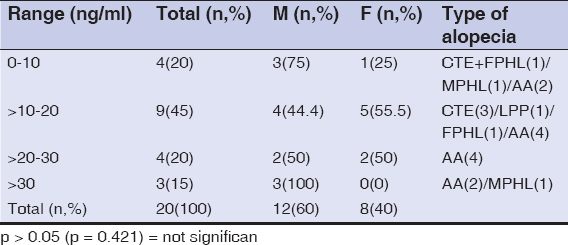 |
Table 2. 25 (OH) Vitamin D levels and alopecia |
DISCUSSION
Recognizing normal qualitative and quantitative parameters of the scalp is critical to identify pathological changes as systematic analysis of histological transverse sections can provide sufficient data for diagnosis [5]. Scalp biopsy gives actual number of hair follicles in a specified area and their stage in hair cycle can be assessed. It is diagnostic in PHL and CTE; the only technique to diagnose inflammatory alopecia with scarring and is a useful predictor of possible regrowth in long standing AA [6]. Multiple samples collected at different moments may help in distinguishing CTE and FPHL [7]. In FPHL, very early cases, atypical presentations and possible coexistence with other types of alopecia may require an HPE for its definition [8]. In MPHL, a biopsy is usually not necessary unless a FPHL, diffuse hair loss or scalp changes suggestive of cicatricial alopecia confuse the diagnosis while in FPHL, it may be sometimes necessary to exclude CTE, diffuse AA or cicatricial alopecia [9].
A single 4mm sample is not always adequately representative of the global process due to regional variation. Multiple sections are required for a correct diagnosis of the type of alopecia and the sections should always be oriented properly in a horizontal position instead of an oblique position for correct analysis of histopathology and defining ratios [6]. Key factors to enhance histopathological diagnosis include knowledge of clinical history and pattern of alopecia, adequate choice of sampling active areas, two 4mm punch biopsy specimens inclusive of subcutaneous tissue [3].
H.P.E. finding was significantly variable compared to clinical diagnosis (p=0.007;p<0.05). This may be due to different stages of evolution, site of sampling, technique used or misleading clinical presentation. Therefore a skin biopsy is advisable.
Vitamin D level was low in 85% patients with p value >0.05 (0.421). Vitamin D receptors (VDRs) are expressed in keratinocytes lining the outer root sheath of hair follicles.Loss of VDR function by inactivating mutations or bioengineered deletions leads to loss of hair follicle cycling and alopecia [10,11]. VDR is also expressed in the hair bulb keratinocytes of the hair follicle, as well as by the sebaceous gland [12]. VDR is required for and is directly involved in hair growth with DNA binding and heterodimerization being critical functions of VDR to regulate hair growth [13]. Strong correlation was found between AA and vitamin D deficiency in a study by Mahamid et al [14]. Even though association of vitamin D level with alopecia was not significant in the above study, evaluation of vitamin D is suggested with studies on a larger scale.
CONCLUSION
In the study, H.P.E. finding was significantly variable compared to clinical diagnosis. Hence, we should opt for a confirmatory skin biopsy wherever feasible. Serum vitamin D level measurement and correction of its deficiency may help in better management of alopecia. Limitations of the study were small sample size, no control group for vitamin D analysis with low level being reported among normal population worldwide.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study.
REFERENCES
1. Bernardez C. Molina-Ruiz AM, Requena L. Histologic features of alopecias-Part 1:Nonscarring alopecias. Actas Dermosifiliogr. 2015;106;158-67.
2. Gordon KA, Tosti A. Alopecia:evaluation and treatment. Clin Cosmet Investigat Dermatol. 2011;4:101-6.
3. Werner B, Mulinari-Brenner F. Clinical and histological challenge in the differential diagnosis of diffuse alopecia:female androgenetic alopecia, telogen effluvium and alopecia areata- Part 1. An Bras Dermatol. 2012;87:742-7.
4. Dhurat R, Saraogi P. Hair evaluation methods:merits and demerits. Intl J Trichol. 2009;1:108-18.
5. Werner B, Mulinari-Brenner F. Clinical and histological challenge in the differential diagnosis of diffuse alopecia:female androgenetic alopecia, telogen effluvium and alopecia areata- Part 11. An Bras Dermatol. 2012;87:884-90.
6. Stefanato CM. Histopathology of alopecia:a clinicopathological approach to diagnosis. Histopathology. 2010;56:24-38.
7. Bikle DD. Vitamin D metabolism and function in the skin. Mol Cell Endocrinol. 2011;347:80-9.
8. Ramos PM, Miot HA. Female pattern hair loss:a clinical and pathophysiological review. An Bras Dermatol. 2015;90:529-43.
9. Olsen EA, Messenger AG, Shapiro J, Bergfeld WF, Hordinsky MK, Roberts JL, et al. Evaluation and treatment of male and female Pattern hair loss. J Am Acad Dermatol. 2005;52:301-11.
10. Mostafa WZ, Hegazy RA. Vitamin D and the skin:Focus on a complex relationship:a review. J Adv Res. 2015;6:793-804.
11. Bikle DD. Vitamin D and the skin:Physiology and pathophysiology. Rev Endocr Metab Disord. 2012;13:3-19.
12. Rosen CJ, Adams JS, Bikle DD, Black DM, Demay MB, Manson JE, et al. The non skeletal effects of vitamin d:an endocrine society scientific statement. Endocr Rev. 2012;33:456–92.
13. Malloy PJ, Feldman D. The role of vitamin D receptor mutations in the development of alopecia. Mol Cell Endocrinol. 2011;347;90-6.
14. Mahamid M, Abu-Elhija O, Samamra M, Mahamid A, Nseir W. Vit D receptor strongly expressed in hair follicles. IMAJ. 2014;16:367-70.
Notes
Conflict of Interest: None declared.
Source of Support: Nil.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|



Comments are closed.