A dyshidrosiform bullous pemphigoid associated with a psoriatic erythroderma: A case report
Aida Oulehri , Hanane Baybay, Zakia Douhi, Sara Elloudi, Fatima Zahra Mernissi
, Hanane Baybay, Zakia Douhi, Sara Elloudi, Fatima Zahra Mernissi
Department of Dermatology, University Hospital Hassan II, Fez, Morocco
Corresponding author: Dr. Aida Oulehri
Submission: 06.06.2020; Acceptance: 17.09.2020
DOI: 10.7241/ourd.2020e.145
Cite this article: Oulehri A, Baybay H, Douhi Z, Elloudi S, Mernissi FZ. A dyshidrosiform bullous pemphigoid associated with a psoriatic erythroderma: A case report. Our Dermatol Online. 2020;11(e):e145.1-e145.4.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Dyshidrosiform bullous pemphigoid (DP) is an unusual localized variant of bullous pemphigoid (BP). It manifests as a vesicobullous eruption, localized to the soles of the feet and/or palms of the hands. To our knowledge, the coexistence of erythrodermal psoriasis with bullous pemphigoid dyshidrosiform has never been described before. We report the case of an 80-year-old woman who presented with psoriatic erythroderma associated with palmar-plantar bullous lesions diagnosed as a dehydrosiform pemphigoid, we treated her with topical treatment with satisfactory outcome.
Key words: Dyshidrosiform; Bullous Pemphigoïde; Psoriasis; Erythroderma, Palmoplantar
INTRODUCTION
Dyshidrosiform bullous pemphigoid (DP) is an unusual localized variant of bullous pemphigoid (BP), first described by Levine et al. in 1979 [1]. It shows with a persistent and recurrent vesicobullous eruption, localized to the soles and/or palms. Since the clinical manifestations of DP are similar to those of pompholyx or bullous tinea pedis, which are more common and benign dermatologic diseases, a proper diagnosis could be delayed [2]. Erythrodermic psoriasis is an uncommon, severe form of psoriasis, accounting for about 1% of psoriatic patients. The concomitant occurrence of psoriasis and bullous pemphigoid, as two well-characterized, chronic inflammatory skin diseases was first described in the literature as early as 1929. Since then less than 100 cases were described worldwide [3]. To the best of our knowledge, coexistence of erythrodermic psoriasis with dyshidrosiform bullous pemphigoid has never been describes before. We report the case of an 80 year-old woman who had this association.
CASE REPORT
An 80-year-old diabetic and hypertensive patient had been suffering from localized psoriasis and were treated with the topical glucocorticosteroid of very strong class alone for more than 50 years. She was admitted for a diffuse pruriginous, érythémato-squamous eruption. The patient reported the appearance of scaly erythematous plaques 20 days ago after hospitalization for diabetic imbalance; she describes the lesions typical of her psoriasis in the elbows and knees, then extension to the other members and to the rest of the body.
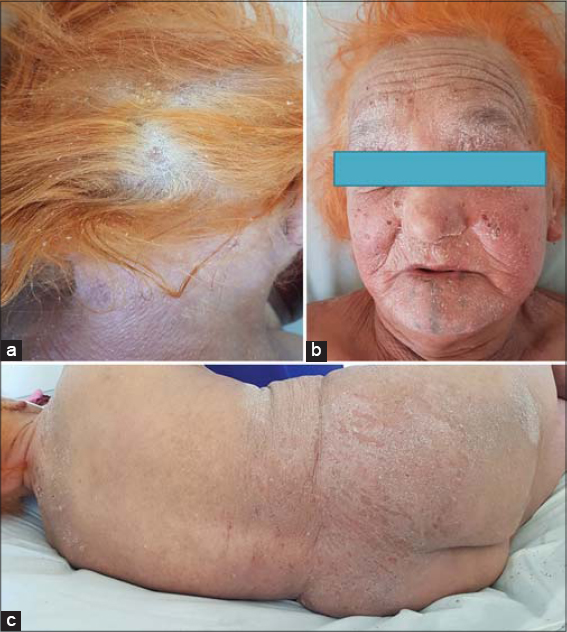
Physical examination revealed a silvery-white scaly erythema on the scalp (Fig. 1a) with a sign of Auspitz positive on dermoscopy. A generalized scaly erythema on the face, trunk and extremities (Figs. 1b, 1c and 2a), indicating erythroderma. The score on the Psoriasis Area and Severity Index (PASI) was 52/72. On examination, we also found multiple palmoplantar blisters and post-bullous erosions, the Nikolsky sign was negative. (Figs. 2a and 2b). No mucosal involvement was observed. The patient reported the application of several plants on her skin which made us first mention the diagnosis of contact dermatitis.
Biopsy specimens from the palms showed subepidermal (junctional) cleft has led to dermal-epidermal separation and a subepidermal blister with eosinophils, neutrophils and fbrin in the blister content, and dermal inflammatory infiltrate made of lymphocytes, histiocytes and eosinophils, with eosinophilic abscesses, and eosinophilic spongiosis (Figs. 3a and 3b).
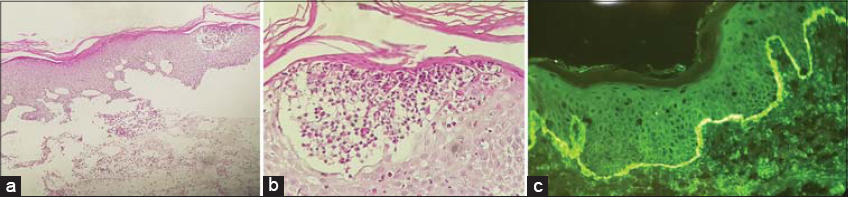 |
Figure 3: a) Subepidermal cleft has led to dermal-epidermal separation and a subepidermal blister with eosinophils, neutrophils and fbrin in the blister content, and dermal inflammatory infltrate. b) Eosinophilic abscesses, and eosinophilic spongiosis, note eosinophilic exocytosis into the epidermis. c) Direct immunofluorescence of the perilesional skin disclosed continuous linear deposits of IgG and C3 along the dermo-epidermal junction. |
Direct immunofluorescence (DIF) of the perilesional skin disclosed continuous linear deposits of IgG and C3 along the dermo-epidermal junction (Fig. 3c). Indirect immunofluorescence (IIF) revealed anti-basement membrane antibody at a titer of 1/1280.
Based on the performed tests and the clinical examination, a dyshidrosiform bullous pemphigoid associated with a psoriatic erythroderma was diagnosed. We had opted for a topical treatment because of the association with psorasis and also considering the age and the comorbidities of the patient. A majestic preparation based on a third vaseline and two thirds coricosteroids very strong class was initiated to treat the erythroderma. The palmoplantar involvement was treated with 20 g of Clobetasol Propionate a day with occlusion. This resulted in a marked clinical improvement in 15 days with no new blister formation (Figs. 4a and 4b). We then achieved a very gradual reduction in treatment, which led to a remission without recurrence for the last 8 months.
 |
Figure 4: a) Fast improvement on palmar region after 10 days of local treatment, the stitches correspond to the biopsy site. b) Good improvement on the face. |
DISCUSSION
DP is a term first used by Levine et al. in 1979 to define a rare localized form of BP, characterized by subepidermal blisters on the palmoplantar areas [1]. Rongioletti et al. [2] reported the second case of dyshidrosiform pemphigoid in a patient with a vesicular eruption of the hands. Barth et al. [3] described three patients with BP who had hemorrhagic pompholyx of the palms and soles. The diagnosis of DP may be misleading for clinicians because clinical lesions are often indistinguishable from dyshidrosiform dermatitis, pompholyx or bullous tinea pedis [4]. Only a skin biopsy revealing the typical pathologic hallmarks of BP, direct immunofluorescence, and the assays for the evaluation of circulating antibodies to BP180 and BP230 allowed a correct diagnosis [5]. As far as we know, only 32 cases of DP have been reported in the literature so far. However, since the diagnosis of DP may be misleading, the disease prevalence could have been underestimated. DP predominately affects the elderly, but sometimes appears in children under 18 years of age [4,6,7]. DP’s pathologic mechanism is currently unknown. Levine et al. [1] proposed that an inflammatory process, such as tinea pedis, could uncover antigens usually protected from antibody recognition. Interestingly, our patient had a chronic mycotic interdigital intertrigo of the feet . Hamm et al. [8] found that plantar sites were the body areas with the greatest BP antigen expression, while palms were not studied. Moreover, a case of DP associated with nickel allergy led to the hypothesis that metal sensitisation may trigger this form of localized BP [9] as already suggested for other autoimmune skin blistering diseases [10]. Therefore, further studies are needed to determine the disease’s exact pathogenesis.
Initially reported as a localized variant of BP, it has been shown that DP may precede or occur concomitantly with generalized lesions of classic BP, Consequently, a follow-up examination is mandatory. According to Caldarola et al. [6], DP can be divided into three groups; group I (vesiculobullous lesions localized in the plamoplantar region), group II (palmoplantar eruption prior to classical BP eruption on the rest of the body by weeks or months) and group III (palmoplantar lesions appeared along with generalized bullous eruption). The same author proposed that a diagnosis of DP may be applied only to Group I and II patients. Group III is defined as BP with simultaneous palmoplantar involvement, which is unexceptional.
The concomitant occurrence of psoriasis and bullous pemphigoid, was first described in the literature in 1929 by Bloom et al. Since then less than 100 cases were described worldwide. Several autoimmune bullous diseases associated with psoriasis have been reported in the literature. These include pemphigus vulgaris, pemphigus foliaceus, pemphigus herpetiformis, linear bullous dermatoses, cicatricial pemphigoid and, epidermolysis bullosa acquisita [11]. Amoung these, bullous pemphigoid is the most frequently reported condition to be associated with psoriasis. It is more common among men than women, with an average age of onset at 63 years. In most cases psoriasis preceded the development of bullous pemphigoid, with an average time interval of 20 years, between the two conditions [12]. Our patient, with an interval of 30 years was well within this range. Also, bullous pemphigoid seems to occur in patients with psoriasis at a younger age than sporadic bullous pemphigoid [13], which wasn’t the case of our patient.
The etiologic and trigger factors responsible for co-occurrence of psoriasis and bullous pemphigoïde remain unknown. A combination of chronic damage to the basal membrane mediated by neutrophilic elastases and matrix metalloproteinases, the recruitment of activated lymphocytes, and the occurrence of numerous antigen presenting cells may lead to self-antigen exposure, and prompt autoimmune mechanisms that induce autoantibody synthesis against hemidesmosomal proteins, such as BP180 and BP230 [12]. Since the coexistence was seen in patients who received a wide range of treatment for psoriasis, as well as in untreated patients, it is difficult to incriminate a single agent as a potentially causative factor in the development of bullous pemphigoid. A reduced barrier function of the psoriatic epidermis, combined with the irritant effects of therapies administered for psoriasis, such as ultraviolet light, psoralen ultraviolet A (PUVA), narrowband UVB irradiation, may precipitate blister formation [13]. Our patient was previously treated only with local corticosteroids. Recently, cases of bullous pemphigoid developing after efalizumab therapy (anti-tumor necrosis factor treatment) of psoriasis have been described [14], also case of BP possibly induced by losartan, an angiotensin II antagonist, in a patient with a severe psoriatic background [15]. Our patient was indeed polymedicated with insulin, inhibitor of the converting enzyme, a beta blocker, aspirin and statins. Several therapeutic modalities have been described for the treatment of coexisting psoriasis and bullous pemphigoid. Immunosuppressive drugs proved to be effective in both diseases; therapeutic options include acitretin, low dose methotrexate, azathioprine, cyclosporine and erythromycin in combination with etretinate or tetracycline in combination with nicotinic acid or dapsone [13,15,16].
CONCLUSION
The clinical manifestation of DP is quite similar to that of pompholyx, which can delay a proper diagnosis. Clinicians should be aware that unusually persistent or haemorrhagic dyshidrosiform dermatitis on the palms and/or soles, particularly in elderly patients, may conceal DP. Therefore, a histopathological study and immunofluorescence microscopy should be performed as soon as possible in all such cases. To the best of our knowledge, coexistence of erythrodermic psoriasis with dyshidrosiform bullous pemphigoid have never been described. Topical corticosteroids are a good therapeutic alternative for elderly and multi-tared patients.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients have given consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Levine N, Freilich A, Barland P. Localized pemphigoid simulating dyshidrosiform dermatitis. Arch Dermatol. 1979;115:320-1.
2. PerellóAlzamora JSD, San Pablo A, Palacios Álvarez I, Santos Briz A, de Unamuno Pérez P. Dyshidrosiform pemphigoid. Med Cutan. 2012;4:112-4.
3. Barth JH, Fairris GM, Wojnarowska F, White JE. Haemorrhagic pompholyx is a sign of bullous pemphigoid and an indication for low-dose prednisolone therapy. Clin Exp Dermatol. 1986;11:409-12.
4. Lupi F, Masini C, Ruffelli M, Puddu P, Cianchini G. Dyshidrosiform palmoplantar pemphigoid in a young man:response to dapsone. Acta Derm Venerol. 2010;90:80-1.
5. Michelerio A, Croci GA, Vassallo C, Brazzelli V. Hemorrhagic vesiculobullous eruption on the palms and the soles as presentation of dyshidrosiform bullous pemphigoid. JAAD Case Reports. 2018;4:61-3.
6. Caldarola G, Fania L, Cozzani E, Feliciani C, De Simone C. Dyshidrosiform pemphigoid:a well-defined clinical entity?Eur J Dermatol. 2011;21:112-3.
7. Dayal S, Sahu P, Jain VK. Dyshidrosiform pemphigoid localized on the hands in a child:a rare occurrence. An Bras Dermatol. 2017;92:714-6.
8. Abreu Velez AM, Vasquez-Hincapie DA, Howard MS. Autoimmune basement membrane and subepidermal blistering diseases. Our Dermatol Online. 2013;4(Suppl.3):647-62.
9. Al-Kamel MA. Clinical diagnosis and a short-term treatment of bullous pemphigoid in an adult Yemeni female:A case report. Our Dermatol Online. 2016;7:312-5.
10. Metal sensitization precipitates skin blistering in epidermolysis bullosa acquisita. – Abstract – Europe PMC. Accessed August 24, 2020. https://europepmc.org/article/med/20507396
11. Jordanov LC, SekulovićLK, MijuškovićZ, Zolotarevski L, ZečevićR. Coexistence of psoriasis vulgaris, bullous pemphigoid and vitiligo:a case report. J Eur Acad Dermatol Venereol. 2002;16:426-7.
12. Wilczek A, Sticherling M. Concomitant psoriasis and bullous pemphigoid:coincidence or pathogenic relationship?Int J Dermatol. 2006;45:1353-7.
13. Jordanov LC, SekulovićLK, MijuškovićŽ, Zolotarevski L, ZečevićR. Concomitant psoriasis and bullous pemphigoid –a case report. Serbian J Dermatol Venereol. 2014;6:30-8.
14. Duong TA, Buffard V, AndréC, Ortonne N, Revuz J, Bagot M, et al. Efalizumab-induced bullous pemphigoid. J Am Acad Dermatol. 2010;62:161-2.
15. Saraceno R, Citarella L, Spallone G, Chimenti S. A biological approach in a patient with psoriasis and bullous pemphigoid associated with losartan therapy. Clin Exp Dermatol. 2008;33:154-5.
16. Abbas D, Rana R, Alireza M, Sareh S, Behnam R. A case of pemphigus foliaceus and pustular psoriasis with a brief review of literature. Our Dermatol Online. 2017;8:406-9.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|
 http://orcid.org/000-0003-3455-3810 http://orcid.org/000-0003-3455-3810 |




Comments are closed.