Clinical and dermoscopy of atypical sclerosing basal cell carcinoma
Aida Oulehri , Sara Elloudi, Hanane Baybay, Zakia Douhi, Fatima Zahra Mernissi
, Sara Elloudi, Hanane Baybay, Zakia Douhi, Fatima Zahra Mernissi
Department of Dermatology, University Hospital Hassan II, Fez, Morocco
Corresponding author: Aida Oulehri, MD
Submission: 13.08.2020; Acceptance: 02.11.2020
DOI: 10.7241/ourd.2020e.143
Cite this article: Oulehri A, Elloudi S, Baybay H, Douhi Z, Mernissi FZ. Clinical and dermoscopy of atypical sclerosing basal cell carcinoma. Our Dermatol Online. 2020;11(e):e143.1-e143.2.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Basal cell carcinoma (BCC) is the most common malignancy. Exposure to sunlight is the most important risk factor. The main clinical subtypes of BCC are nodular, superficial, and morphea form. Combinations of the latter two types with nodular BCC may occur1. Morpheaform BCC accounts for a low proportion of cases, estimated at 5 to 10 percent. It is called sclerosing due its clinical resemblance to a localized scleroderma [1]. Also known as infiltrating BCC, morpheaform BCC is usually more aggressive than nodular and superficial BCC as it tends to exhibit subclinical spread with the potential for extensive local destruction [2].
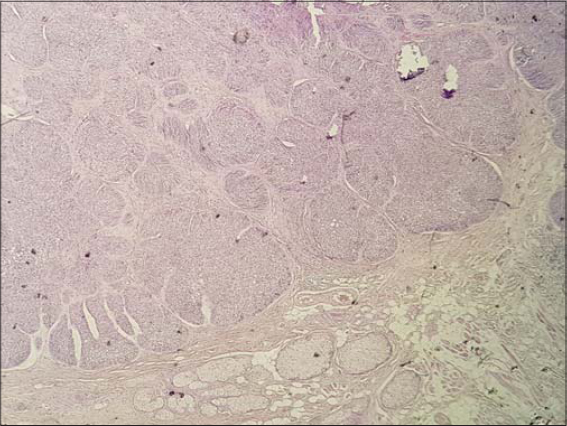
The patient is seventy years old and is hospitalized for the management of a large right orbital squamous cell carcinoma. On clinical examination, we find a pink-to-ivory-white, shiny, smooth, scar-like, indurated plaque with ill-defined borders on the posterior side of the left ear pinna (Fig. 1). Dermoscopy reveals telangiectasia without a tree trunk and rounded yellowish structures (Fig. 2). The lesion is completely asymptomatic and the patient has never been aware of its presence. Removal of the lesion was performed during surgery for his squamous cell carcinoma and the result was in favour of nodular histopathological subtype of basal cell carcinoma with large nests of basaloid cells in the dermis accompanied by peritumoral retraction from the stroma and peripheral palisading (Fig. 3).
Our patient’s case had a complete discordance between the clinic and histology. It was non-aggressive as it had been evolving for several years and did not increase in size. We were able to explain the good prognosis of the lesion by the absence of a morpheiform contingent in histology.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
REFERENCES
1. Scrivener Y, Grosshans E, Cribier B. Variations of basal cell carcinomas according to gender, age, location and histopathological subtype. Br J Dermatol. 2002;147:41-7.
2. Marzuka AG, Book SE. Basal cell carcinoma:pathogenesis, epidemiology, clinical features, diagnosis, histopathology, and management. Yale J Biol Med. 2015;88:167-79.
Notes
Source of Support: Nil.
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/000-0003-3455-3810 http://orcid.org/000-0003-3455-3810 |





Comments are closed.