The role of general practitioners in the prevention and screening of skin cancer: a cross-sectional study in Morocco
Aida Oulehri 1, Hanane BayBay1, Angéla Filankembo Kava2, Zakia Douhi1, Sara Elloudi1, Samira El Fakir1, Fatima Zahra Mernissi1
1, Hanane BayBay1, Angéla Filankembo Kava2, Zakia Douhi1, Sara Elloudi1, Samira El Fakir1, Fatima Zahra Mernissi1
1Dermatology Department of the University Hospital Center Hassan II, Fez, Morocco, 2Laboratory of Epidemiology, Clinical Research and Community Health- Faculty of Medicine and Pharmacy of Fez, Fez, Morocco
Corresponding author: Aida Oulehri, MD
Submission: 04.08.2020; Acceptance: 04.11.2020
DOI: 10.7241/ourd.2020e.134
Cite this article: Oulehri A, BayBay H, Filankembo Kava A, Douhi Z, Elloudi S, El Fakir S, Mernissi FZ. The role of general practitioners in the prevention and screening of skin cancer: a cross-sectional study in Morocco. Our Dermatol Online. 2020;11(e):e134.1-e134.9.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Given the high incidence of skin cancer (SC) in several countries around the world, general practitioners (GPs) are playing an increasingly important role in the prevention and early detection of this disease. The main objective of our study was to evaluate the current role of GP’s in the prevention and early detection of skin cancer. The secondary objectives were to determine the GP’s level of knowledge, their lack of information and their need for education on skin cancer.
Methods: We realized a cross-sectional descriptive survey by means of a questionnaire among GPs practicing in the private and public sector in the city of Fes.
Results: 158 general practitioners issued a completed and usable questionnaire. The average age was 45.91 years, sex ratio M/F =1.05. The number of years of exercise varied between one year and 39 years with the predominance of the bracket; between 10 and 20 years of experience. 47.5% estimated that their dermatological activity represented less than 10% of their overall activity. The majority of physicians surveyed stated that they rarely or never carry out all practices related to skin cancer prevention and screening, the main obstacle being the difficulty in recognizing suspicious lesions. 60.8% of physicians stated that they never gave photoprotection advice to their patients. 1.3% had participated in a specific training course on skin cancer screening; 92.9% selected “lack of proposal” as their reasons for non-participation in such a course. Among the general practitioners in the study, 91.1% considered that it was essential to reinforce their knowledge, particularly in terms of training in the recognition of suspicious lesions (88.6%). The evaluation of knowledge about skin cancer showed a good level of knowledge among 54.7% of the doctors questioned and an insufficient level among 43.1%.
Conclusion: Most GPs are willing to take part in SC prevention and screening in their daily practice. However, our results demonstrate a high need for additional education and training.
Key words: General practitioners; Prevention; Screening; Skin cancer
INTRODUCTION
At present, one in three of the world’s diagnosed cancers is skin cancer. Several recent studies indicate that their incidence has increased significantly in recent years in many countries in the world [1–3].
In Morocco, skin cancer is generally underestimated. Skin cancer is not currently a public health priority, yet there are strong arguments in favor of promoting the early detection and the prevention of skin cancer in our country. Indeed we live in a country with high rate sunshine exposure [4]. Several national studies have found a high sunshine exposure on our population , moreover, our country is experiencing a change in the demographic profile of our aging population gradually becoming similar to what is in Europe [5].
The early detection of skin cancers makes it possible to obtain considerable reduction of morbidity and especially the reduction of mortality for some aggressive skin tumors like melanoma and squamous cell carcinoma. The treatment of a skin tumor detected at its early stage is much simpler for the patient than at an advanced stage. However, factors such as low density of dermatologists and limited access of patients to specialized consultations for skin examinations are a major problem that has been observed in all countries, even in the most developed ones [6] and Morocco is no exception to this rule [7]. Given this finding coupled with the dramatic increase in the incidence of skin cancer, it seems inevitable that GPs will play a greater role in the screening for skin cancer [8].
However, the GP has not necessarily received the sufficient training in the diagnosis of these tumors or in identification of patients at risk of developing SC. Indeed there are concerns about the diagnostic capabilities of GP’s regarding skin lesions suspected of malignancy [9]. This is why we sought to determine if cutaneous cancer screening was carried out regularly and readily in the daily practice of GP’s, while assessing their knowledge and the need for further training in this specific domain.
MATERIALS AND METHODS
Study Design
This was a cross-sectional study, spread over a period of 4 month, between October 2018- December 2018 in the city of Fez in Morocco.
Sampling
We included in our study all GP’s practicing in the public and private sectors in the city of Fez.
We obtained the list of the GP’s in the city of Fez from the regional Ministry of health for public sector, and from the office of the registrar of the medical council for the private sector.
The city of Fez is hosting 42 health centres and 132 general practitioners in the public sector. The number was reduced after applying the criteria for non-inclusion to 112 doctors. For the doctors in the liberal sector, the medical council communicated to us a list of 128 doctors in private practice with a total of 240 general practitioners included in the study. We excluded from our study general practitioners assigned to specialized structures performing specific tasks and whose patients are selected such as addictology centres, childbirth centres, CDTMR (centre for the diagnosis of tuberculosis and respiratory diseases), hemodialysis centres, SAMU (emergency medical services), school hygiene, as well as general practitioners who only provide emergency care..
Data Collection
The data were collected by an anonymous self-administered questionnaire completed by GPs after their informed consent. We visited all of the physicians included in the study in their workplaces and hand-delivered the questionnaire to them who completed it and handed it to us directly. Investigators were volunteers from the medical staff of the department of dermatology of the Hospital Hassan II of Fez.
Collection Tool: The Questionnaire
After a bibliographical research on the subject, we established a questionnaire composed of four parts responding to the different objectives we had fixed ourselves.
Our questionnaire consisted of 116 questions, including 5 numerical questions, 38 dichotomous qualitative questions (closed-ended question for which the respondent’s choice is limited to two possibilities: female/male, private/public, yes/no, true/false …), 39 multichotomous single-answer qualitative questions, 28 multiple-choice qualitative questions and 6 ordinal questions with the five-point Likert scale (range: never to always) as a measurement scale.
This questionnaire was validated in a multidisciplinary meeting, including experts in Dermatology, Clinical epidemiology and scientific research.
The questions were then tested and validated on a sample of the population before the survey was conducted.
The first part covered socio-demographic variables such as age (year), sex (male/female), sector of activity (private/public), original training and additional training, followed by quantitative variables relating to practice such as number of years of practice, average number of total consultations/day, and average number of dermatological consultations/day. The age of the GP’s was represented into 3 classes: between 25 and 40 years, between 41 and 50 years and above 50 years. The initial training was divided into Moroccan medical training and others. The complementary training was divided into dermatology or others. The duration of GP’s practice in years was calculated from the year graduation and it was divided into less than 10 years, between 10 and 20 years and above 20 years. The dermatological activity was divided in 3 parts: <10 %, between 10 and 20% and > 20%.
The second part concerned the evaluation of daily prevention and screening practices in skin cancerology. This part enabled us to study the general practitioner’s opinion on his role on the topic, his daily practice habits in terms of research into skin cancer risk factors, the systematic performance of clinical dermatological examinations and the place of photoprotection advice in his educational arsenal, the options to each question was divided into never, rarely (<10%), sometimes (10-39%), often (40-69%) and always (>70%). We also assessed in this part of the questionnaire the frequency and nature of the difficulties encountered by practitioners in the practice of skin cancer screening.
The third part concerned the evaluation of the training needs of general practitioners on the topic. In this part, we analyzed the degree of participation of general practitioners in continuing medical education in general and in dermatology or onco-dermatology training in particular, the reasons which prevent them from participating in these training courses, the need to complete their training on the subject and the content of this training which seems most useful and relevant to them.
The fourth part enabled us to test the knowledge of general practitioners on skin cancer. First of all, we wanted to know what general practitioners thought about the frequency of skin cancers in our region, so we asked them to choose between four propositions: Rare, infrequent, frequent, don’t know. Then to assess GPs’ knowledge of risk factors for skin cancer, we created a table containing 16 proposals and asked doctors to tick one of the following four options for each proposal; risk factor, protective factor, not related, don’t know. All of the proposals were risk factors.
In order to evaluate the ability of GPs to determine the phototype of their patients, which will considerably help them to identify subjects at risk, three color photographs were attached to the questionnaire; for each photograph the doctor had to tick one of the 6 phototypes or tick the 7th box; don’t know.
There are several precancerous lesions that GPs need to be aware of and which the presence in a patient should alert them to, requiring vigilance on their part and regular monitoring to look for the slightest sign of transformation. Two tables have been designed for this purpose. The first contained four proposals, including eight precancerous lesions and six lesions that do not present a risk of degeneration. For each proposal, the doctor had to choose between three possible answers; risk of degeneration, no risk of degeneration and don’t know. In the following table, we have tried to present some frequent clinical situations that the general practitioner could be confronted with in his daily practice in order to evaluate his reasoning and conduct; five clinical situations have been presented to the doctor with for each one three possible answers; i suspect a malignant process, i do not suspect a malignant process and don’t know.
There are several common misconceptions about skin cancers, including their prognosis, location and age of onset. We have tested through a table made of eight dichotomous true/false questions the state of knowledge of general practitioners concerning these points. Finally, we wanted to know what kind of photoprotection advice GPs are used to giving. To this end, we proposed the main rules of photoprotection in three categories: behavioral photoprotection, clothing photoprotection and external photoprotection, and we asked them to tick off for each category the photoprotection advice they usually give to their patients. A total of twenty-five photoprotection tips have been suggested to the doctors. Parts of the questionnaire concerning knowledge assessment were included in Table 1.
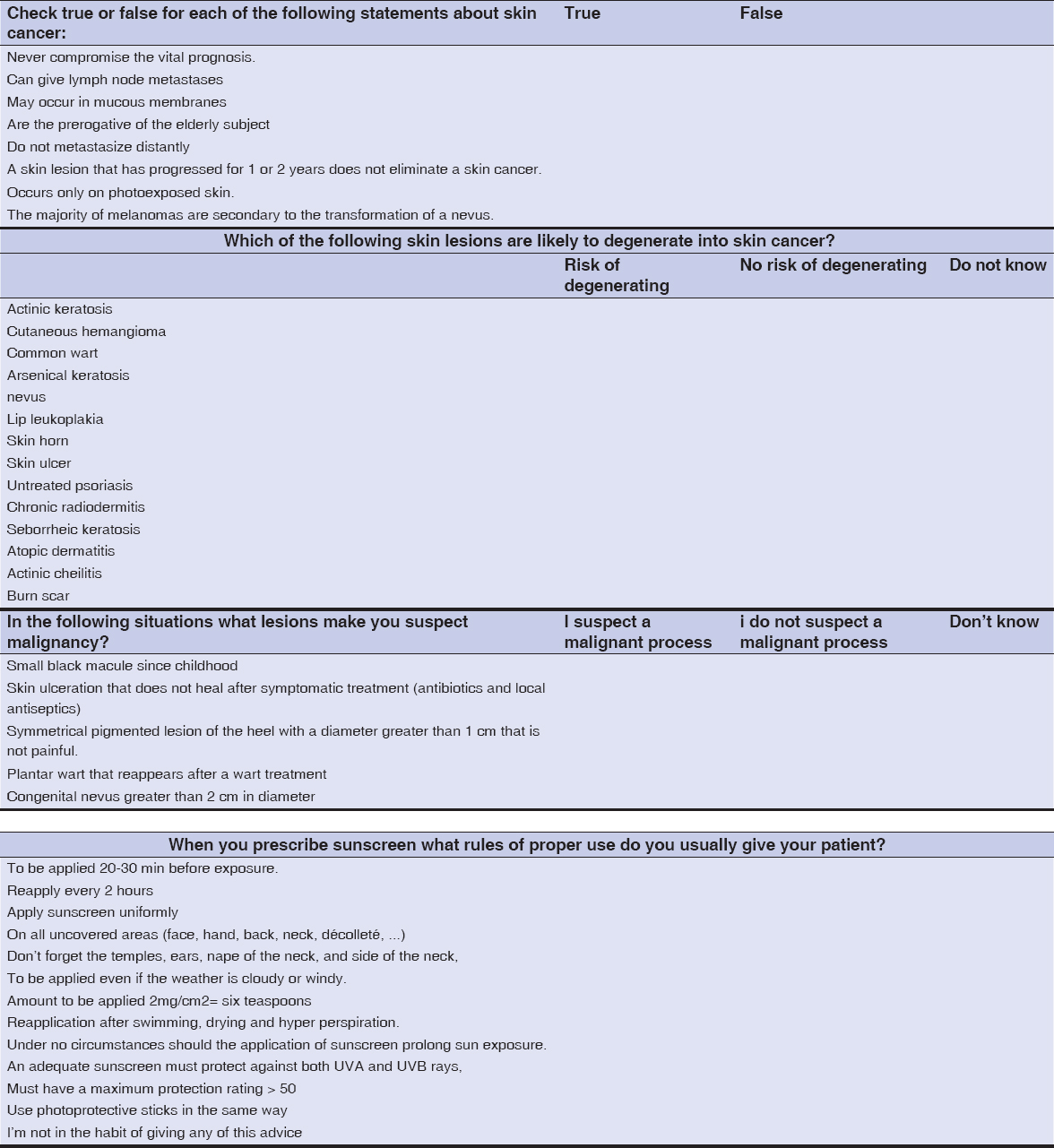 |
Table 1: Parts of the questionnaire concerning the assessment of the knowledge of GPs in skin cancer |
At the end of this chapter we wanted to correlate our results with the many variables studied in our survey. To do this we have developed a level of knowledge in cooperation with the medical epidemiology staff, taking the median as the threshold, so that we could divide our population into two groups: Good level of knowledge for doctors who gave more than 23 correct answers, insufficient level of knowledge for physicians who gave less than 23 correct answers.
Statistical Analysis
A descriptive, univariate and multivariate analysis using the SPSS 21 software were performed. In the descriptive analysis, quantitative variables were expressed by means ± standard deviation and qualitative variables by percentages. The “Chi-square” test was used to compare percentages in order to determine the factors associated with the practice and the knowledge level. A p value less than 0.05 was considered statistically significant.
Ethics Statement
Ethical approval was obtained from the ethics committees at Hospital Center University Hassan II in Fez, Morocco. All the doctors were informed of the conditions related to the study and gave their written informed consent for the study and for publication.
RESULTS
At the end of this survey, we were able to collect 158 completed and usable questionnaires. We remind you that our target population consisted of 240 general practitioners, i.e. a response rate of 65.83%. Our sample is thus representative of the general practitioners of the city of Fez.
The rest of the doctors are represented by doctors on leave (sickness, maternity, administrative leave, etc.) which numbered 42, the doctors having refused to fill in the questionnaire: the main reason given by these doctors was lack of time (13), the questionnaires filled in incompletely (16) and finally the doctors in the private sector having changed activity (resident, doctor on call in a clinic, etc.) or having moved outside the city of Fez (11).
Socio-demographic Characteristics
The mean of age of the GP’s was 45.91 ± 10.28 years (26-66 years). The most frequent age range of our GP’s were those between 41 and 50 years and that of those above 50 years with the same percentage of 34.2%. The male GP’s represented 51.3% representing sex ratio of 1.05. The majority of the GP’s obtained their medical degree in Morocco (89.1%). 44.3% had between 10 to 20 years of working experience.
A majority of our doctors practiced in the private sector, they represented 56%. The dermatological activity in practice was in majority (47.5%) less than 10%.
Prevention and Screening Practices
Almost all the GP’s representing 96.2% affirmed that the prevention and screening of skin cancer falls under the role of the general practitioner. In practice, 51.2% of GP’s do not search for risk factors of skin cancer. In their routine practice 15.2% of GP’s perform skin examinations, 16.5 % conduct inspection of mucous membranes of the mouth, and genitals. 12% of GP’s conduct inspection of the scalp, hair and nails. The systematic search for suspicious skin lesions wasn’t done in 61.4% of cases. In risk factor patients, only 22.8% followed patients to monitor the development of cancer. 39.2% of GP’s usually advice on photoprotection in their practice.
Over a period of one year (2018) 65.8% of general practitioners referred less than 10 patients to the dermatologist for suspected skin lesions. Out of these GP’s, 43.6% of them acknowledged having difficulties in screening skin cancer and the main reasons mentioned were the inability to identify suspicious lesions as well as the lack of consultation time per patient (50% of them).
97.5% of the GP’s responded that they had not participated in a skin cancer screening campaign. Only 4 doctors representing 2.5% had participated in such an event before.
Needs Assessment for Further Training
Only 5.1% of GP’s participated in dermatology training throughout 2018, 92.9% of them responded that they had never been offered this kind of training. Doctors wishing to complete their training in skin cancer screening felt that certain elements were essential to its content, in particular training in the recognition of suspicious lesions (88.6%), training in the various methods of photoprotection (82.3%) and training in the means of educating patients at risk (80.4%).
Knowledge on Skin Cancer
More than half of GP’s responded that skin cancer is uncommon and rare in the city of Fez (69.6%), 10.8% thought that it’s a frequent cancer and 19.6% did not know. Table 2 summarizes the percentage of correct responses for each risk factor. All GP’s recognized that chronic sun exposure is a risk factor, followed by personal history of skin cancer and high number of nevus. Other risk factors have been recognized by far fewer physicians such as smoking, organ transplant patients and PUVA therapy. A very important finding was that 20.6% of GPs declared that there was no link between skin cancer and sun exposure in childhood, 6.3% of doctors even stated that it was a protective factor against skin cancer.
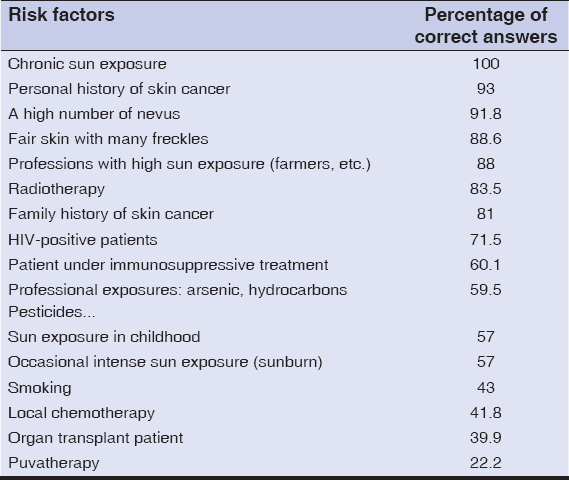 |
Table 2: Ranking in decreasing order of risk factors according to the percentage of correct answers from GPs |
89.9% of the doctors replied that they did not know how to determine the phototype of their patients. For pre-cancerous lesions; actinic keratosis (47.5%), arsenical keratosis (51.9%), skin ulcer (58.9%) and burn scarring (47.5%) were only recognized as such by about half of the doctors questioned. Higher rates of good response were obtained for Nevus (86.7%), lip leukoplakia (79.7%) and chronic radiodermatitis (79.7%). A low percentage of good response was noted for cutaneous horn (28.5%) and actinic cheilitis (13.9%).
For the proposed clinical cases, 70% of the doctors were able to recognize the suspicious nature of the two proposed situations (skin ulcer that does not heal and asymmetrical black heel patch) (Table 1). The results were more inhomogeneous for the benign clinical situations; 75.3% of the doctors were able to recognize the small black macule evolving since childhood as not suspicious of malignancy. On the other hand only 34.2% and 45.6% of the doctors recognized respectively the recurrent plantar wart and the congenital nevus as not suspicious.
Table 3 summarizes the percentages of correct answers given by GPs in relation to the main common believes about skin cancers in our context. A response rate of over 80% was observed for the first five proposals concerning the prognosis, extent and site of skin cancers. Lower rates were observed for the 6th and 7th proposals concerning the age of onset and progression. And a low percentage of correct answers for the last proposal on the melanoma – nevus relationship.
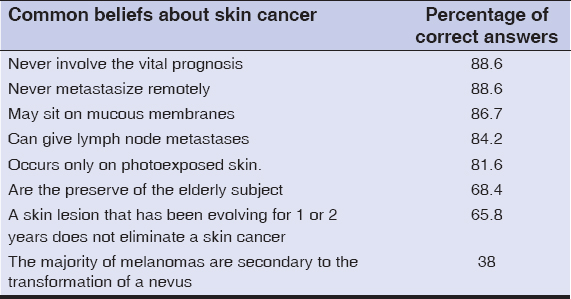 |
Table 3: Percentage of correct answers for each proposal on general skin cancer knowledge |
Concerning the knowledge of photoprotection modalities, it should be recalled that the section on the evaluation of knowledge on photoprotection measures was only completed by the 39.2% of the doctors questioned who certified that they regularly give photoprotection advice to their patients. Apart from avoiding sun exposure between noon and 4 p.m. and avoiding intense and prolonged exposure, all the other rules of photoprotection are known by less than half of these doctors with percentages ranging from 47.5% (Reapply every 2 hours), and 44.3% (Ensure eye protection with sunglasses) to 2.5% (quantity 2mg/cm2) and 1.3% (Use photoprotective sticks for lips).
The average mark for good responses to our questionnaire was scored at 28.01 (out of 46) with a standard deviation of 6.01. This represents a minimum of 13 correct answers and a maximum of 40 correct answers. Regarding the level of knowledge, we divide our population into two groups: 54.7% of the GP’s had a good level of knowledge on skin cancer, 43.1%of them had insufficient knowledge on skin cancer.
Statistical analysis using the Chi 2 test showed the existence of a significant difference in practice in terms of skin cancer risk factor research between the private and public sectors, with more frequent practice in the private sector and the existence of a significant difference in practice in terms of complete skin examination according to age, with predominance of the over-50 age group. The existence of a significant difference in the level of knowledge according to age, with a better level of knowledge among 25-50 year olds compared to over 50 year olds, and according to whether or not they participate in continuing medical education, with a better level of knowledge among the participants.
DISCUSSION
In our neighboring country France, dermatological consultations represent about 5% of the reasons for consulting a general practitioner [10]. Another French study had found a dermatological activity of general practitioners between 0 and 15% of their overall activity for 85% of them [11]. The results of our study are close to those of the literature with a dermatological activity between 0 and 10% of their overall activity for 47.5% of the doctors and between 10 and 20% for 36.1% of them. On a national level, to our knowledge, there was no study allowing us to compare our results with those of other towns or regions of the kingdom. In view of these data, it could therefore be considered that the dermatological activity of the doctors in our study was not negligible.
An overwhelming majority of physicians surveyed are willing to play a greater role in the prevention and screening of skin cancers; however, our results demonstrate a high need for additional education and training.
One of the most important early detection strategies relies on a complete skin examination of the patient’s body [12]. The majority of GPs in the city of Fez do not screen for skin cancers either in terms of searching for risk factors during interrogation, complete clinical examination, and systematic research for suspicious skin lesions. Similar results have also been found in a broad literature encompassing several different countries [13–16]. This lack of practice has been strongly implicated in the lack of awareness of skin cancer by GPs [17–19]. However; several studies have shown that the awareness-raising actions of health professionals have been followed by a significant increase in the rate of complete skin examination [20].
This lack of screening was also illustrated by the very low number of patients referred by the GPs of the study to a dermatologist for a suspicious skin lesion during one year, especially when we compared our figures with those of the literature [11].
The main obstacle in detecting skin cancers found in our study has been the difficulty of recognizing suspicious skin lesions, we also noticed after a review of the literature that this is a universal obstacle faced by GPs in all countries where this has been studied [2,12,21,22]. This can be explained by the wide fields of practice for GP’s who is required to perform in many areas. However, the level of experience and training of a physician increases his diagnostic performance. This suggests the need to strengthen the training of general practitioners in recognizing the main suspicious skin lesions to optimize early detection.
The correlation of GP screening practices to the different variables of our study, has allowed us to note that the older generation, that is GP’s over 50 years are the ones who perform the most detection of skin cancers by interrogation and clinical examination. (p significant for complete skin examination). We must therefore insist on young doctors; including medical students; on the central role of the general practitioner in cutaneous cancer screening, as well as the importance of the interrogation and the physical examination before considering any complementary examination as sophisticated as it may be. The second finding was the existence of a significant difference in practice in terms of skin cancer screening between the private and public sectors, with more frequent practice in the private sector. This result is easily explained by the workload of public sector physicians. This leads us to propose solutions such as the establishment of a specialized consultation in cancer screening, or the organization of regular screening campaigns for skin cancers in the general population or individuals at risk. For this last point we noted in our study that almost all the doctors in our study never participated in a skin cancer screening campaign.
The vast majority of GPs had never participated in medical training to prevent and screen skin cancers. The main reason given was the lack of proposals for such trainings. This suggests that these GP’s will be willing to participate in such trainings. For the success of such a program, close collaboration between the different training structures and learned societies is necessary. In addition, the GPs of the city of Fez are aware of their role to play in the prevention and screening of skin cancers and have expressed their wish for continuing medical education on this subject.
Our study showed an underestimation of GPs on the frequency of skin cancer in their region , While at the national level the Fez region is recording the highest frequency since it is the only region where skin cancers are in second place after digestive cancers out of all cancers recorded between 2004 and 2010 [23]. This suggests that information on the epidemiological data on skin cancer will be a very good motivator to optimize prevention and screening practices. In terms of prevention, our survey revealed a lack of knowledge of general practitioners on the measures on photoprotection and the importance of preventing skin cancer in children. While sun exposure during childhood is widely blamed in the literature for the genesis of skin cancer since it accounts for 50 to 80% of skin damage incurred over the whole of life [24]. Childhood is thus a crucial age for the future risk of skin cancer [25]. Specific strategies to protect the child population should be encouraged to reduce the future incidence of skin cancer.
In our survey, GPs are not used to advising their patients on photoprotection measures. While several studies have indicated that the photoprotection advice provided by general practitioners is more effective than that provided by impersonal means of communication [26,27]. There are few studies available on solar radiation exposure in Morocco despite the important issues related to this subject. Awareness and prevention campaigns on the dangers of exposure to the sun are not very common on the radio, television or other media scenes.
During our survey, we found that the questionnaire itself helped to draw the attention of general practitioners in the city of Fez to the value of preventing and screening for skin cancers. This study is not without limitations, especially the geographical limitation of the sample
CONCLUSION
The general practitioner represents the cornerstone in the primary and secondary prevention of skin cancers. Our results demonstrate a high need for additional education and training, which justifies the establishment of continuing medical education programs on the subject as well as the organization of sensitization and screening campaigns for skin cancers involving general practitioners in collaboration with dermatologists.
ACKNOWLEDGEMENTS
We are indebted to all doctors who participated in this study and gave their consent. We thank all department of Dermatology and clinical epidemiology for their enormous help.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Flohil SC, de Vries E, Neumann HAM, Coebergh J-WW, Nijsten T. Incidence, prevalence and future trends of primary basal cell carcinoma in the Netherlands. Acta Derm Venereol. 2011;91:24-30.
2. Grange F. Epidémiologie du mélanome cutané:données descriptives en France et en Europe [Epidemiology of cutaneous melanoma:descriptive data in France and Europe]. Ann Dermatol Venereol. 2005 Dec;132:975-82.
3. Remontet L, Estève J, Bouvier AM, Grosclaude P, Launoy G, Menegoz F, et al. Cancer incidence and mortality in France over the period 1978-2000. Rev Epidemiol Sante Publique. 2003;51:3-30.
4. Bankable solar data for better decisions. Accessed August 4, 2020. https://solargis.com/
5. PNPCC – VOL 1 – Axe épidémiologie- études des facteurs de risques. [epidemiology and risk factor studies axis] Accessed August 4, 2020. http://www.contrelecancer.ma/fr/documents/pnpcc-axe-epidemiologie-etudes-des-facteurs-de-ris/
6. Rat C, Houd S, Gaultier A, Grimault C, Quereux G, Mercier A, et al. General practitioner management related to skin cancer prevention and screening during standard medical encounters:A French cross-sectional study based on the International Classification of Primary Care. BMJ Open. 2017;7:e013033.
7. Le PNPCC. Accessed August 4, 2020. http://www.contrelecancer.ma/fr/le_pnpcc
8. van Rijsingen MCJ, van Bon B, van der Wilt GJ, Lagro-Janssen ALM, Gerritsen MJP. The current and future role of general practitioners in skin cancer care:an assessment of 268 general practitioners. Br J Dermatol. 2014;170:1366-8.
9. Offidani A, Simonetti O, Bernardini M, Alpagut A, Cellini A, Bossi G. General Practitioners’Accuracy in Diagnosing Skin Cancers. Dermatology (Basel, Switzerland). 2002;205:127-30.
10. Shieh Y, Eklund M, Sawaya GF, Black WC, Kramer BS, Esserman LJ. Population-based screening for cancer:hope and hype. Nat Rev Clin Oncol. 2016;13:550-65.
11. YAICHE T, TIBI (Mélanie) Y. Early Cutaneous Cancer Screening:Evaluation of Practices in General Medicine and Analysis of the Needs of General Practitioners in Val de Marne. Thesis, University Paris Est Creteil, 2012.
12. Durbec F, Vitry F, Granel-Brocard F, Lipsker D, Aubin F, Hédelin G, et al. the role of circumstances of diagnosis and access to dermatological care in early diagnosis of cutaneous melanoma:a population-based study in France. Arch Dermatol. 2010;146:240-6.
13. Duarte AF, da Costa-Pereira A, Del-Marmol V, Correia O. Are General Physicians Prepared for Struggling Skin Cancer?-Cross-Sectional Study. J Cancer Educ. 2018;33:321-4.
14. Janda M, Elwood M, Ring IT, Firman DW, Lowe JB, Youl PH, et al. Prevalence of skin screening by general practitioners in regional Queensland. Med J Aust. 2004;180:10-5.
15. Walter FM, Humphrys E, Tso S, Johnson M, Cohn S. Patient understanding of moles and skin cancer, and factors influencing presentation in primary care:a qualitative study. BMC Family Practice. 2010;11:62.
16. Ahmadi K, Prickaerts E, Smeets JGE, Joosten VHMJ, Kelleners-Smeets NWJ, Dinant GJ. Current approach of skin lesions suspected of malignancy in general practice in the Netherlands:a quantitative overview. J Eur Acad Dermatol Venereol. 2018;32:236-41.
17. Geller AC, O’Riordan DL, Oliveria SA, Valvo S, Teich M, Halpern AC. Overcoming obstacles to skin cancer examinations and prevention counseling for high-risk patients:results of a national survey of primary care physicians. J Am Board Fam Pract. 2004;17:416-23.
18. Garrido AQ, Wainstein AJA, Brandão MPA, de Vasconcellos Santos FA, Bittencourt FV, Ledsham C, et al. Diagnosis of Cutaneous Melanoma:the Gap Between the Knowledge of General Practitioners and Dermatologists in a Brazilian Population. J Cancer Educ. 2020;35:819-25.
19. Rodrigues M. Skin Cancer Risk (Nonmelanoma Skin Cancers/Melanoma) in Vitiligo Patients. Dermatologic Clinics. 2017;35:129-34.
20. Henrikson NB, Morrison CC, Blasi PR, Nguyen M, Shibuya KC, Patnode CD. Behavioral Counseling for Skin Cancer Prevention:A Systematic Evidence Review for the U.S. Preventive Services Task Force. Agency for Healthcare Research and Quality (US);2018. Accessed October 25, 2020. http://www.ncbi.nlm.nih.gov/books/NBK493693/
21. Johansson M, Brodersen J, Gøtzsche PC, Jørgensen KJ. Screening for reducing morbidity and mortality in malignant melanoma. Cochrane Database Syst Rev. 2019;6:CD012352.
22. Weinstock MA. Cutaneous melanoma:public health approach to early detection. Dermatol Ther. 2006;19:26-31.
23. Hospital Cancer Registry Preliminary results from the Pathological Anatomy Department chu Hassan II Fez (About 5532 cases). Published October 20, 2012. Accessed August 4, 2020. http://www.chu-fes.ma/registre-hospitalier-des-cancers-resultats-preliminaires-du-service-danatomie-pathologique-chu-hassan-ii-fes-a-propos-de-5532-cas/
24. Gupta M. Assessment of knowledge, attitudes and practices about sun exposure and sunscreen usage in outpatients attending a Dermatology Clinic in North India. Our Dermatology Online. 2019;10:34-7.
25. Bebe FN, Hu S, Brown TL, Tulp OL. Metastatic melanoma in Florida, 1996-2010:Racial, demographic, occupational and tumor characteristics, and burden of metastasis. Our Dermatol Online. 2018;9:369-79.
26. Krensel M, Schäfer I, Zander N, Augustin M. [Primary prevention in the context of skin cancer screening]. Hautarzt. 2019;70:432-7.
27. Vuong K, Trevena L, Bonevski B, Armstrong BK. Feasibility of a GP delivered skin cancer prevention intervention in Australia. BMC Fam Pract. 2014;15:137.
Notes
Source of Support: Nil.
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/000-0003-3455-3810 http://orcid.org/000-0003-3455-3810 |



Comments are closed.