Epstein–Barr virus-positive mucocutaneous ulcer in a child, a rare immunoblastic B lymphoma
Siham Belmourida , Hind Palamino, Meriame Meziane, Nadia Ismaili, Laila Benzekri, Karima Senouci
, Hind Palamino, Meriame Meziane, Nadia Ismaili, Laila Benzekri, Karima Senouci
Department of Dermatology and Venereology, Ibn Sina Hospital, Rabat Morocco
Corresponding author: Dr. Siham Belmourida
Submission: 14.02.2020; Acceptance: 19.04.2020
DOI: 10.7241/ourd.2020e.124
Cite this article: Belmourida S, Palamino H, Meziane M, Ismaili N, Benzekri L, Senouci K. Epstein–Barr virus-positive mucocutaneous ulcer in a child, a rare immunoblastic B lymphoma. Our Dermatol Online. 2020;11(e):e124.1-e124.3.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Epstein–Barr virus-positive mucocutaneous ulcer (EBV+, MCU) is a temporary entity, recently included in the 2016 World Health Organization (WHO) classification of haemopathies malignancies [1]. We report an interesting clinical case that highlights this new entity in a 13-year-old child.
A 13-year-old girl, with no history, presenting chronic mucocutaneous nasal ulcerations, the clinical examination finds, a girl in good general condition with centro-facial ulcerations, (Figs. 1 and 2) without associated lymphadenopathy and the rest of the somatic examination was no abnormality. The biological and radiological exploration did not show any specific anomaly, the biopsy objectifying a polymorphic dermal infiltrate with sternbergoide type B cells, EBV + expressing the antigens CD15, CD30, CD20, (Figs. 3 and 3) MUM1 with reactive T lymphocyte pax positive. The extension assessment did not show any anomaly. The immunoglobulin weight assay showed no immunodeficiency.
 |
Figure 1 Mutilating centrofacial ulcerations. |
 |
Figure 2 Destruction of the nasal septum. |
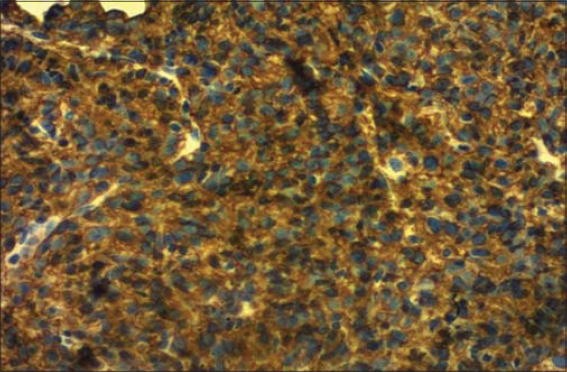 |
Figure 3 Diffuse labeling of lymphoma cells by CD20. |
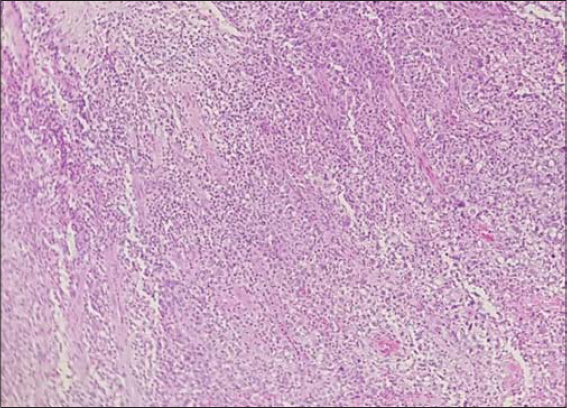 |
Figure 4 Biopsy of the nasal mucosa at low magnification. |
The diagnosis of EBV-positive skin and mucosal ulcer of the WHO 2016 classification ofhaemopathies was retained and a treatment with poly chemotherapy (Rituximab, Vincristine, Cyclophosphamide and Doxorubicin) was initiated with excellent progress and a decline of 11 months without recurrence (Fig. 5).
 |
Figure 5 Improvement under chemotherapy. |
(EBV+, MCU) presents with a chronic ulcer of the oropharynx, skin, gastrointestinal tract or rarely the genital mucosa. Histologically, (EBV+, MCU) is made of a polymorphic infiltrate with large sternbergoide B cells that express the EBV transcript, the CD15, CD30 and CD20 antigens, with reactive T cells [2]. The diagnosis with certainty is sometimes difficult, but generally the indolent clinical character without systemic involvement, with the possibility of spontaneous regression [2–5]. The presence of CD15 + and EBER + lymphoma cells without angiocentrism as well as the absence of B clonality are compatible with this diagnosis [6].
The treatment of this new entity is not yet well defined, the few cases reported in the literature have been treated either by standard chemotherapy, CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone), or by rituximab and bendamustine, others responded well to radiotherapy alone [7].
EBV+, MCU a difficult diagnostic entity, is important to identify the diagnostic criteria, the factors that determine its evolution and the need for treatment in order to provide an adequate diagnosis and better management.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
REFERENCES
1. Swerdlow SH, Campo E, Pileri SA. The updated WHO classification of hematological malignancies. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127:2375-91.
2. Dojcinov S, Venkataraman G, Raffeld M, Pittaluga S, Jaffe ES. EBV positive mucocutaneous ulcer—a study of 26 cases associated with various sources of immunosuppression. Am J Surg Pathol. 2010;34:405–17.
3. Steven SH, Quintanilla-Martinez L, Willemze R, Kinney MC. Cutaneous B-cell lymphoproliferative disorders:report of the 2011 Society for Hematopathology/European Association for Haemato pathology Workshop. Am J Clin Pathol. 2013;139:515-35.
4. Nelson AA, Harrington AM, Kroft S, Dahar MA, Hamadani M, Dhakal B. Presentation and management of post-allogeneic transplantation EBV-positive mucocutaneous ulcer. Bone Marrow Transplant. 2016;51:300-2.
5. Katzenstein AL, Doxtader E, Narendra S. Lymphomatoid granulomatosis:in- sights gaine dover 4 decades. Am J Surg Pathol. 2010;34:e35–e48.
6. Pittaluga S, WilsonWH, Jaffe ES. Lymphomatoid granulomatosis. Lyon, France:International Agencyfor Research on Cancer;2008.
7. Filliatre L, Ortonne N, Delaunay C, Thomas J, Chetouani A, Marcon N, et al. EBV skin-mucous ulcer, a morphologically disturbing entity contrasting with an excellent prognosis:about a case. Ann Dermatol. 2014;34:407-8.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-2795-9161 http://orcid.org/0000-0002-2795-9161 |



Comments are closed.