A slow-growing glistening tumor on a female patient’s face: what is your diagnosis?
Nadia Nabli 1, Rima Gammoudi1, Najet Ghariani1, Badreddine Sriha2, Lobna Boussofara1, Mohamed Denguezli1
1, Rima Gammoudi1, Najet Ghariani1, Badreddine Sriha2, Lobna Boussofara1, Mohamed Denguezli1
1Department of Dermatology, Farhat Hached University hospital, Sousse, Tunisia, 2Department of Anatomopathology, Farhat Hached University hospital, Sousse, Tunisia
Corresponding author: Dr. Nadia Nabli
Submission: 15.07.2020; Acceptance: 17.09.2020
DOI: 10.7241/ourd.2020e.123
Cite this article: Nabli N, Gammoudi R, Ghariani N, Sriha B, Boussofara L, Denguezli M. A slow-growing glistening tumor on a female patient’s face: what is your diagnosis? Our Dermatol Online. 2020;11(e):e123.1-e123.2.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
CASE REPORT
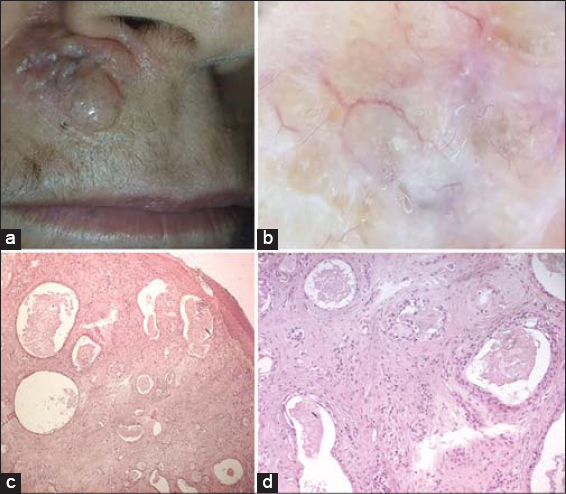
A 59-year-old woman presented with a 5-year history of an asymptomatic slow-growing nodule on the upper lip. The physical examination revealed a well-defined, 15 × 30 mm diameter, dome-shaped and firm nodule, with an irregular, telangiectatic and glistening surface (Fig. 1a). Dermoscopic assessment revealed a dense whitish-brown structureless area with central fine linear branched blood vessels, pigmented ovoid nests and white peripheral clods of variable diameter (Fig. 1b). Histopathological examination of an excisional biopsy, performed using an elliptical excision, revealed dermal invasion with malignant tumor cells arranged in lobules. Severe nuclear atypia was seen in the cells (Fig. 1c). On higher magnification, the tumor was composed of small keratin-filled cysts and islands of basaloid keratinocytes. Some of the lobules showed duct-like structures extending into the deeper dermis and surrounded by a sclerotic stroma (Fig. 1d).
ANSWER
Microcystic adnexal carcinoma
DISCUSSION
Microcystic adnexal carcinoma (MAC) is a rare, slow-growing, malignant cutaneous neoplasm with pilar and eccrine gland differentiation [1,2]. Clinically, MAC manifests as asymptomatic, slowly growing, and firm nodule, plaque, or cyst-like tumor with well-defined borders and a soft telangiectatic surface, most commonly located on the head and neck [3]. A search of the literature has discovered few published dermatoscopy images of MAC. The most common dermatoscopic features of the tumor are the dense central whitish-brown structureless area with linear arborizing vessels and the peripheral white-yellowish clods of variable diameter [1,3–5]. The diagnosis is based on histopathological examination of a full thickness biopsy that shows small keratin-filled cysts with nests and cords which resemble ductal structures [2]. Radical excision of the tumor is the most recommended therapy with two options including wide local excision with postoperative margin evaluation and Mohs micrographic surgery [2]. Although MAC rarely metastasizes, a long term follow-up is preconized given the high potential for local aggressivity and recurrence [1,2].
REFERENCES
1. Inskip M, Magee J. Microcystic adnexal carcinoma of the cheek :a case report with dermatoscopy and dermatopathology. Dermatol Pract Concept. 2015;5:7.
2. Aslam, A. Microcystic Adnexal Carcinoma and a Summary of Other Rare Malignant Adnexal Tumours. Curr Treat Options in Oncol. 2017;18:49.
3. Calderón-Castrat X, Román-Curto C, Santos-Briz A, Fernández-López E. Microcystic adnexal carcinoma mimicking basal cell carcinoma. JAAD Case Reports. 2017;3:492–4.
4. Rie S, Shin-ichi A, Azusa O, Hidenori M, Hidehisa S, Masaru T. Dermoscopic findings of microcystic adnexal carcinoma. Eur J Dermatol. 2015;25:516-8.
5. Astorino S, Carelli G, Dattola A, Pasquini P. Microcystic adnexal carcinoma of the skin in atypical site (pubic region):clinical and dermatoscopic features. G Ital Dermatol Venereol. 2020;155:231-2.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-1367-1423 http://orcid.org/0000-0002-1367-1423 |



Comments are closed.