Congenital hemangioma « PICH » in a young adult: A case report
Asmae Rasso , Sara Elloudi, Hanane Baybay, Sara Dahoki, Zakia Douhi, Fatima Zahra Mernissi
, Sara Elloudi, Hanane Baybay, Sara Dahoki, Zakia Douhi, Fatima Zahra Mernissi
Department of Dermatology CHU Hassan II, Fez, Morocco
Corresponding author: Dr. Asmae Rasso
Submission: 12.06.2020; Acceptance: 20.06.2020
DOI: 10.7241/ourd.2020e.106
Cite this article: Rasso A, Elloudi S, Baybay H, Dahoki S, Douhi Z, Mernissi FZ. Congenital hemangioma « PICH » in a young adult: A case report. Our Dermatol Online. 2020;11(e):e106.1-e106.3.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Congenital hemangiomas are fully formed vascular tumors at birth, they have been divided into 3 major subtypes based on clinical behavior: rapidly involuting congenital hemangioma (RICH), Partially evolving congenital hemangioma (PICH) and non-involuting congenital hemangioma (NICH). We describe a33 years -old men, consulted for management of lesion in the lateral-thoracic level, had been presented since birth, with notion of increasing in size. Dermatological examination showed an angiomatous plaque of 19 cm on the left later-thoracic level, with a scarred fibre-adipal center. Doppler echography, and histology have concluded to Partially evolving congenital hemangioma PICH.
Key words: Congenital hemangioma; Histology; Partially evolving congenital hemangioma
INTRODUCTION
Congenital hemangiomas are vascular tumors arise and proliferate in utero. In contrast to infantile hemangiomas, which typically enlarge after birth and then involute. The Congenital hemangiomas are rare and have a variable course. They are divided into 3 subgroups including rapidly evolving congenital hemangioma (RICH), and non-invasive congenital hemangioma (NICH), and recently the partially evolving congenital hemangioma (PICH), they are based on the clinical features and clinical presentation [1]. We report the case of a 33-year-old male presented with a congenital hemangioma of the PICH type.
CASE REPORT
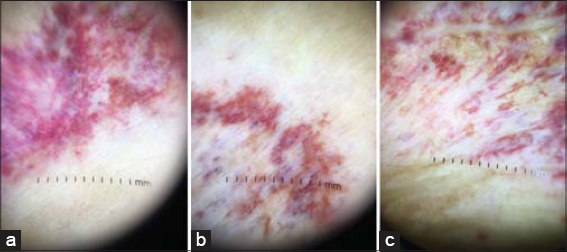
A 33 years old man, without any notable pathological antecedent, was consulting in the dermatology department for the management of lesion at the lateral thoracic level which has been bleeding spontaneously for more than 2 months, without any notion of pain or other associated signs. The patient reported that the lesion had been present since birth with a notion of increase in size up to the age of 14 years and then involution. Dermatological examination showed an angiomatous plaque of 19 cm on the left later-thoracic level, with a scarred fibre-adipal centre, no trillium, no heat, no murmur on auscultation, with a satellite 3 cm plaque of the same aspect. Blanching or a halo-like effect seen surrounding the lesion (Figs. 1a – 1c). The palpation had found two mobile subcutaneous nodules in both planes of approximately 15 mm with the presence of hemorrhagic crusts. Dermoscopy objectified diffuse vascular lagoons with telangiectasias (Figs. 2a – 2c). Doppler ultrasonography had shown a hypoechogenic subcutaneous tissue nodule with an arterio-venous vascular pedicle, compatible with an angiomatosis component, measuring 15 mm, and exploration of the rest of the lesional range showed subcutaneous fat replacement by hyperechogenic scarring tissue.
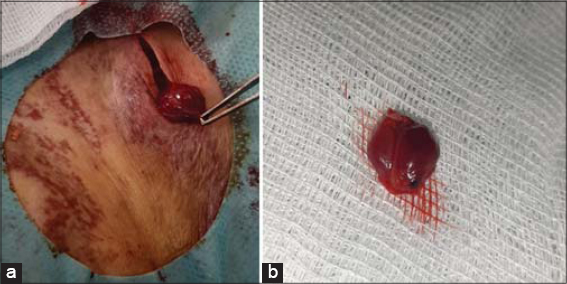
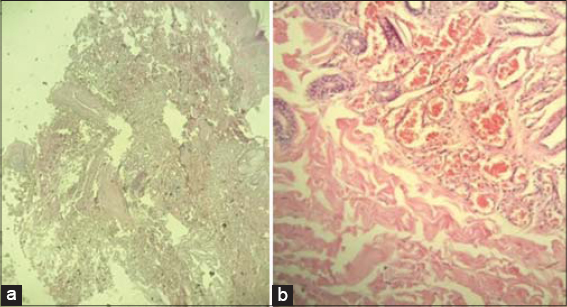
Two skin biopsies were done, one at the level of the subcutaneous nodule (Figs. 3a and 3b), and histologically the nodule was well limited made of several capillary vascular structures arranged in lobules separated by fibrous septa. These vascular structures are bordered by regular endothelial cells and sometimes gorged with red blood cells. There is no sederophagus, no calcification, no endothelial turgidity, no endothelial turgidity and no extra-medullary hematopoiesis within the limit of the fragment. The second skin biopsy at the level of the angiomatous plaque showed an epidermis slightly acanthotic and regular. The dermis and hypodermis are dissociated by vascular proliferation made up of medium sized structures bordered by regular endothelial cells. These cells are congestive with no sign of malignancy (Figs. 4a and 4b). Glucose transporter1 not made by lack in our hospital. After confirmation of the absence of clinical and histological malignancy and stabilization of the lesion, the patient was reassured and recommended for surveillance.
DISCUSSION
Infantile hemangioma is the most common vascular tumor and presents as an endothelial cellular proliferation that develops within days after birth. Congenital hemangiomas are fully developed at birth and are classified as RICHs, PICHs, and NICHs according to their clinical outcome [1,2]. Congenital hemangiomas have an almost equal distribution among the sexes, are usually solitary, and are mainly located in the head or near a joint in the limbs. common features include red-purple color with multiple tiny or coarse telangiectasias, often a surrounding pale halo, and sometimes a central ulceration, linear scar, or central nodularity. RICH involutes in the 6-14 months of life, leaving a residual patch of thin skin with prominent veins and a normal blood ow, with little, if any, subcutaneous fat. In a smaller proportion of patients, involution may be incomplete, leaving a vascular plaque with coarse telangiectasia on the surface and a peripheral bluish white border, resulting in a lesion are now as PICH. NICHs persist and grow in proportion with the patient [3]. On Doppler ultrasound imaging, RICH, PICH and NICH are usually confined to the subcutaneous fat and appear heterogeneous, with occasional calcifications and multiple arteries and veins exhibiting high-velocity blood flow. NICH contains vascular shunts more frequently than RICH [4]. Histopathological, RICH and NICH also demonstrate overlapping features, although certain findings may help distinguish them. RICH is characterized fewer lobules in the center of the lesion as it is the first area to undergo involution. The blood vessels possess a thin basement membrane and plump endothelial cells in the early stages. Later, the basement membrane appears thickened and lobules are surrounded by fibrous tissue, and dystrophic calcification, thrombosis, hemosiderin deposition, and extramedullary hematopoiesis may be seen [5]. NICH is characterized by large lobules of capillaries that may appear more dilated, larger, and thicker walled than those seen in RICH. When the histology of PICH is not well described in the literature often compatible with congenital hemangioma and indistinguishable from RICH or NICH [5,6].
CONCLUSION
PICH is a rare vascular tumor that generally presents a good prognosis. whose diagnosis is difficult based on several chronological, radiological and histological clinical arguments to retain it. Further studies are necessary to identify this entity for a accurate diagnosis allows, an adequate treatment and an appropriate parent counseling.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
REFERENCES
1. Inakanti Y, Narsimha Rao TV. Infantile Haemangioma –An unusual location. Our Dermatol Online. 2015;6:343-6.
2. Doulla M, Bako H, Salissou L, Ouédraogo MM, Hassane I, Abdoulaye M, Moumouni H. Management of hemangiomas by propranolol:Epidemiological, clinical and therapeutic aspects:retrospective study about 15 cases. Our Dermatol Online. 2018;9:7-10.
3. Lee PW, Frieden IJ, Streicher JL, McCalmont T, Haggstrom AN. Characteristics of noninvoluting congenital hemangioma:a retro-spective review. J Am Acad Dermatol. 2014;70:899-903.
4. Jaiprakash P, Pai K, Monappa V. Hémangiome épithélioïde cutanéimitant la tuberculose de Montgomery infectée. Notre Dermatol Lig. 2018;9:422-4.
5. Nasseri E, Piram M, McCuaig CC, Kokta V, Dubois J, Powell J. Partially involuting congenital hemangiomas:a report of 8 cases and review of the literature. J Am Acad Dermatol. 2014;70:75-79.
6. Nasseri E, Piram M, McCuaig CC, Kokta V, Dubois J, Powell J. Partially involuting congenital hemangiomas:a report of 8 cases and review of the literature. J Am Acad Dermatol. 2014;70:75-9.
7. Cossio ML, Dubois J, McCuaig CC, Coulombe J, Hatami A, Marcoux D, et al. Non- involuting congenital hemangiomas (NICH) with postnatal atypical growth:A case series. Pediatr Dermatol. 2019;36:466–70.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/000-0003-3455-3810 http://orcid.org/000-0003-3455-3810 |




Comments are closed.