Chronic solitary plaque of the scalp: what’s your diagnosis?
Safa Idoudi 1, Yosra Soua1, Nouha Ben Abdeljelil2, Jameleddine Zili1
1, Yosra Soua1, Nouha Ben Abdeljelil2, Jameleddine Zili1
1Department of Dermatology, Fattouma Bourguiba University Hospital, Monastir, Tunisia; 2Departement of Anapathology, Fattouma Bourguiba University hospital, Monastir, Tunisia
Corresponding author: Dr. Safa Idoudi
Submission: 22.05.2020; Acceptance: 28.06.2020
DOI: 10.7241/ourd.2020e.82
Cite this article: Idoudi S, Soua Y, Abdeljelil NB, Zili J. Chronic solitary plaque of the scalp: what’s your diagnosis? Our Dermatol Online. 2020;11(e):e82.1-e82.2.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
CASE REPORT
A 60-year-old man with a history of type 2 diabetes mellitus and dyslipidemia consulted for a scalp lesion evolving for a year. The examination found an erythematous plaque of the vertex surrounded by telangiectasia and associated with perifollicular hyperkeratosis and tufted hair, without alopecia (Fig. 1). Previous local infections treated by oral antibiotherapy was reported.
 |
Figure 1: Erythematous plaque of the vertex surrounded by telangiectasia and associated with perifollicular hyperkeratosis and tufted hair, without alopecia. |
Dermoscopic examination revealed decreased of follicular ostia with perifollicular hyperkeratosis and telangiectasia (Fig. 2).
 |
Figure 2: Dermoscopic photograph showing a decrease in the number of follicular ostia with perifollicular hyperkeratosis and telangiectasia (*50, Dino-lite pro-polariser USB dermoscope). |
Besides, the rest of the somatic examination was without abnormalities.
HISTOPATHOLOGY
Histopathological examination (hematoxylin and eosin stain) showed at higher magnification (*100) a lymphocytic lichenoid infitrat including the hair follicule with Civatte bodies (Fig. 3). The overlying epidermis was normal.
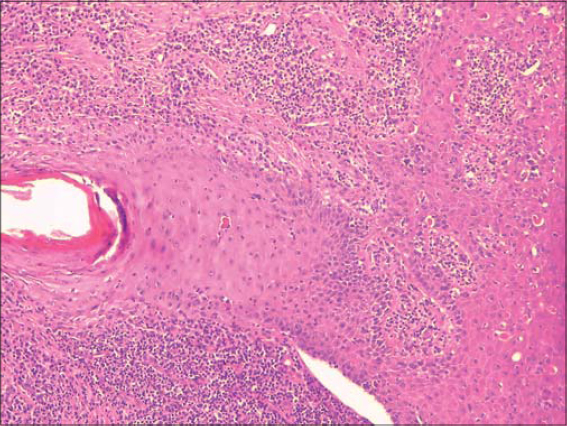 |
Figure 3: Histological aspect showing a lymphocytic infiltrate involving the isthmus and infundibulum of the hair follicle with Civatte bodies (HE*100). |
WHAT’S YOUR DIAGNOSIS?
Answer: Lichen planopilaris (LPP).
DISCUSSION
Lichen planopilaris is an uncommon cutaneous disorder characterized by chronic lymphocytic inflammation. It is classically presenting as follicular keratotic plugs and/or perifollicular scaling with perifollicular erythema leading to scarring alopecia [1]. The absence of alopecia is uncommon and could be seen at an early stage of the disease. Dermoscopy can contribute to the diagnosis of LPP and even assess its activity by showing in the center of the bald areas a lack of follicular orifices and on the margin, a pink perifollicular inflammation with keratin scale surrounding and extending along the proximal part of the hair shaft [2]. These findings histologically correspond to perifollicular hyperkeratosis and vacuolar changes with the presence of necrotic keratinocytes in the basal layer of the hair follicle [3]. Other aspects may be found such as white dots or patches, pigment network or blue-grey pattern around white dots and follicles realizing a target pattern [4].
LPP is associated with cutaneous or mucosal lesions of lichen planus in about 30% of cases [5]. Management often involves topical or intralesional steroids as a first-line treatment in limited forms otherwise hydroxychloroquine, acitretin and mycophenolate mofetil can be used. As cicatricial alopecia, the main goal of therapy is to prevent the progression of the lesions.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
REFERENCES
1. Assouly P, Reygagne P. Lichen planopilaris:uptade on diagnosis and treatment. Semin Cutan Med Surg. 2009;28:3-10.
2. Lajevardi V, Mahmoudi H, Moghanlou S, Ansari M, Teimourpour A, Daneshpazhooh M. Assessing the correlation between trichoscopic features in lichen planopilaris and lichen planopilaris activity index. Australas J Dermatol. 2019;60:214–8.
3. Soares VC, Mulinari-Brenner F, Souza TE. Lichen planopilaris epidemiology:a retrospective study of 80 cases. An Bras Dermatol. 2015;90:666–70.
4. Rakowska A, Slowinska M, Kowalska-Oledzka E, Warszawik O, Czuwara J, Olszewska M, et al. Trichoscopy of cicatricial alopecia. J Drugs Dermatol. 2012;11:753-8.
5. Weston G, Payette M. Update on lichen planus and its clinical variants. Int J Womens Dermatol. 2015;1:140–9.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|



Comments are closed.