A case of congenital melanocytic nevus with Sutton’s phenomenon
Kaoutar Achehboune , Khadija Elboukhari, Zakia Douhi, Sara Elloudi, Hanane Baybay, Fatima Zahra Mernissi
, Khadija Elboukhari, Zakia Douhi, Sara Elloudi, Hanane Baybay, Fatima Zahra Mernissi
Department of Dermatology, Hassan II Hospital University, Fez. Morocco
Corresponding author: Dr. Kaoutar Achehboune
Submission: 14.10.2019; Acceptance: 27.12.2019
DOI: 10.7241/ourd.2020e.79
Cite this article: Achehboune K, Elboukhari K, Mernissi FZ, Douhi Z, Elloudi S, Baybay H. A case of congenital melanocytic nevus with Sutton’s phenomenon. Our Dermatol Online. 2020;11(e):e79.1-e79.2
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Sutton’s nevi are commonly develop in adolescents and children. They consist of a depigmented halo surrounding a benign melanocytic nevus, primary or metastatic melanomas or neurofibromas. Sutton’s phenomenon is rarely developed around congenital nevi. We rapport a case of 45-year-old woman who developed Sutton’s phenomenon around a congenital melanocytic nevus. Repeated searches for associated malignant melanoma were negative. We review the rare cases of halo congenital nevi and emphasize that depigmentation is not necessarily associated with malignant degeneration.
Key words: Congenital pigmented nevi, Halo phenomenon, Sutton, Dermoscopie
INTRODUCTION
Sutton’s nevi are commonly develop in adolescents and children. Sutton’s phenomenon is rarely developed around congenital nevi. We rapport a case of Sutton’s phenomenon around a verrucous congenital melanocytic nevus.
CASE REPORT
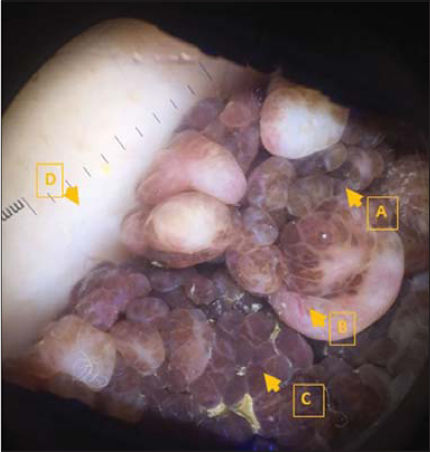
A 45-year-old woman who has a verrucous congenital lesion on her back for which she has never consulted. The appearance of a recent halo since one year has pushed her to consult. The clinical examination found a verrucous pigmented tumor of 5 cm pedicled base, well limited, non-ulcerated, not painful, surrounded by an achromic whitish macula (Fig. 1), with auto-fluorescence to the wood’s lamp. Dermoscopy had found a verrucous aspect, with homogeneous pigmentation and the presence of linear vessels without dermoscopic signs of malignancy (Fig. 2). The clinical examination of the rest of the body was normal. Given the evolution of the Sutton phenomenon for 3 years, the absence of clinical or dermoscopic signs of malignancy in the congenital pigmented nevus and the examination of the rest of body was normal; we retained; congenital pigmented nevus with a halo phenomenon. The patient chose to keep her nevi. We indicated surveillance. Otherwise the patient is in good health since 3 years.
DISCUSSION
The progression of congenital melanocytic nevi (CMN) is very varied. They may remain unaltered during the entire life of the patient, undergo malignant degeneration, present color alterations (lightening or darkening) or developing achromic peri-lesional halo with consequent involution of the nevus (halo nevus) [1] as described in this case.
A Sutton’s nevus can also be known as a halo nevus or a leukoderma acquisitum centrifugum are more commonly develop in adolescents and children [2]. They consist of a depigmented halo surrounding a benign melanocytic naevus (congenital or acquired melanocytic nevi, nevocellular nevus, blue nevus, Spitz nevus), neurofibromas and primary or metastatic melanomas [1,2]. Halo nevi develop in approximately 1% of Caucasians [3]. Congenital nevi rarely develop depigmentation, only a few cases have been reported in the literature [4,5]. Halo nevi have occurred in patients with sporadic melanoma, but also in patients with melanoma in congenital giant nevi [6,7]. Investigation of recent clinical and dermoscopic changes in the central melanocytic lesion (congenital nevi in our case) such as heterogenicity of pigmentation, ulceration, pain and increased size or bleeding should prompt biopsy at looking for melanoma. In our case the evolution of the clinical and dermoscopic signs was reassuring, so, we have opted for surveillance.
CONCLUSION
The goal of this article is to document a rare case of congenital pigmented nevus with a nevus halo, to emphasize that Sutton’s nevi does not indicate obligatory conversion to malignant melanoma. However, thorough should be performed in such cases.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Copyright by Kaoutar Achehboune, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
REFERENCES
1. Awad SS, Abdel Aziz RT, Mohammed SS. Management of resistant halo nevi. J Cosmet Laser Ther. 2019;21:118-21.
2. Burian EA, Jemec GBE. Eruptive melanocytic nevi:A review. Am J Clin Dermatol. 2019;20:669-82.
3. Nicolétis-Lombart I, Kervarrec T, Zaragoza J, Machet MC, Samimi M. Multiple “Halo Nevi“occurring during pembrolizumab treatment for metastatic melanoma. Int J Dermato. 2019;58:739-41.
4. Kopf AW, Bart RS. A congenital pigmented nevus associated with leukoderma. J Dermatol Surg Oncol. 1981;7:547-9.
5. Brownstein MH, Kazam BB, Hashimoto K. Halo congenital nevus. Arch Dermatol. 1977;113:1572-5.
6. Amico S, Jacquemin C, Boniface K, JulliéM-L, Taieb A, Seneschal J. An unusual presentation of Sutton’s phenomenon presenting as halo cherry angioma, J Eur Acad Dermatol Venereol. 2019;33:e464-e465.
7. Langford MA, Al-Ghazal SK. Halo naevus or malignant melanoma:A case report. JPRAS Open. 2018;16:98-9.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0001-7687-0158 http://orcid.org/0000-0001-7687-0158 |




Comments are closed.