Systemic follicular lymphoma with cutaneous involvement
Rhizlane Chaoui 1, Sara Elloudi1, Selma El Kadiri1, Soukaina Chhiti1, Zakia Douhi1, Hanane Baybay1, Fatima Zahra Mernissi1, Mouna Rimani2
1, Sara Elloudi1, Selma El Kadiri1, Soukaina Chhiti1, Zakia Douhi1, Hanane Baybay1, Fatima Zahra Mernissi1, Mouna Rimani2
1Department of Dermatology, University Hospital Hassan II, Fez, Morocco; 2Laboratory of Pathology Hassan Rabat, Morocco
Corresponding author: Dr. Rhizlane Chaoui
Submission: 11.03.2020; Acceptance: 20.05.2020
DOI: 10.7241/ourd.2020e.43
Cite this article: Chaoui R, Elloudi S, El Kadiri S, Chhiti S, Douhi Z, Baybay H, Mernissi FZ, Rimani M. Systemic follicular lymphoma with cutaneous involvement. 2020;11(e):e43.1-e43.4.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Follicular lymphoma is an indolent, mature B-cell neoplasm which present with slowly progressive lymphadenopathy. Skin involvement is not rare and it is mandatory to distinguish between primary cutaneous follicle center lymphoma (PCFCL) andsystemic/nodal follicular lymphoma secondarily involving the skin. We report a case of Systemic follicular lymphoma with cutaneous involvement. Complete staging is mandatory in cutaneous B lymphomas to discriminate a primary cutaneous follicle center lymphoma (PCFCL) from systemic/nodal follicular lymphoma secondarily involving the skin.
Key words: Primary cutaneous follicular center B-cell lymphoma; Systemic follicular lymphoma; skin involvement
INTRODUCTION
Follicular lymphoma (FL) is an indolent, mature B-cell neoplasm which present with slowly progressive lymphadenopathy. Skin involvement is not rare and it is mandatory to distinguish between primary cutaneous follicle center lymphoma (PCFCL) and systemic/nodal follicular lymphoma secondarily involving the skin.
We report a case of Systemic follicular lymphoma with cutaneous involvement.
CASE REPORT
A 40-year-old man, presented with a 2-year history of a painless, itchy erythematous lesion on the back that was rapidly increasing in size.1 year later the patient reported similar lesions at the periphery of the initial lesion. The patient was in otherwise good health without any significant past medical history.
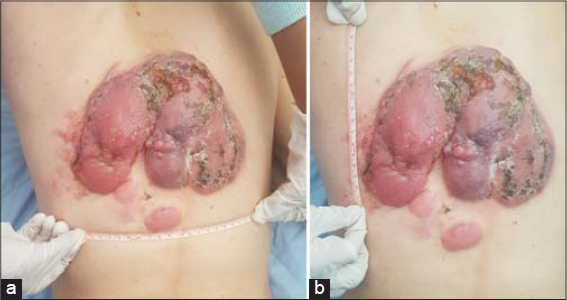
Dermatological examination revealed three well demarcated tumors, erythematous in color,hard in consistency with an irregular contours and smooth surface involving the back (Fig. 1). The greatest tumor was adhered to the deep plans, mersuring 18*16 cms, ulcerated, bleeding on contact with hemorrhagic crusts (Figs. 2 and 2b).
Multiple erythematous plaques and papules,varying in size were noted at the periphery of the tumor described above (Fig. 3).
 |
Figure 3: Multiple erythematous plaques and papules of varying size at the periphery of the greatest tumor. |
Dermoscopy of the tumor showed fine short linear vessel, curved linear vessel in a spermatozoa-like arrangement,telangiectasias with arborizing vessels (Figs. 4a and 4b).
 |
Figure 4: Dermoscopy showing a: Telangiectasias with arborizing vessels. b: Fine short linear vessel, curved linear vessel in a spermatozoa-like arrangement. |
Axillary examination showed multiple lenticular bilateral axillary lymph nodes.However the abdomen was soft and no hepatosplenomegaly was noted.
In front of this clinical presentation we thought about many diagnosis such us darrier ferrand dermatofibrosarcoma,anaplastic large cell lymphoma and aggressive B cell lymphoma.
A skin biopsy was performed and histopathological examination revealed a dense dermal lymphoid infiltrate consisting of enlarged centrocytes with cleaved nuclei and centroblasts with larger, rounder nuclei and several peripheral nucleoli admixed with few histiocytes and small lymphocytes (Figs. 5a and 5b).
 |
Figure 5: a and b: Dense dermal and hypodermal lymphoid infiltrate consisting of enlarged centrocytes (HES G x 200). |
Immunohistochemistry revealed positivity of the large lymphoid cell for CD20, Bcl-6 and negativity for CD10, CD3, CD5, CD23 and Bcl-2.Moreover, neoplastic B cells showed both a high proliferation rate (Ki-67) (Figs. 6a – 6e).
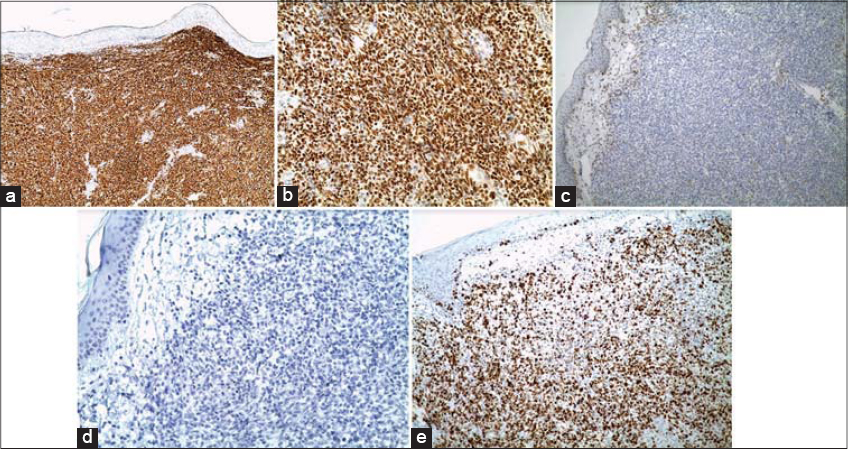 |
Figure 6: Immunohistochemistry revealed positivity of the large lymphoid cell for CD20 (a), Bcl-6 (b) and negativity for Bcl-2 (c) and CD10 (d) with a high proliferation rate of Ki 67 (e). |
Diagnosis of cutaneous follicle center cell lymphoma was made.
Complete staging was performed to assess systemic disease. Laboratory tests including lactate dehydrogenase, beta 2-microglobulin and protein electrophoresis were unremarkable.Lymph node ultrasound revealed a malignant lymphadenopathy at the left axillary measuring 1.5 cm. An excision was performed showing a lymph node location of follicle center cell lymphoma.Computed tomography scan of the neck,chest, abdomen, and pelvis was normal.
The patient was treated with RCHOP (Rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone) regimen to a total of eight sessions (Rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone) with complete remission of the skin lesions. The patient has been followed without signs of relapsing.
DISCUSSION
Primary cutaneous B-cell lymphomas comprise approximately 20% of cutaneous lymphomas. These lymphomas typically occur on the head or neck of adults with a median age of 60 years and have a slight male predominance [1].
The World Health Organization (WHO) has categorized primary CBCLs into 4 subtypes: primary cutaneous marginal zone lymphoma (pc-MZL), primary cutaneous follicle center lymphoma (pc-FCL), and primary cutaneous diffuse large B-cell lymphoma (DLBCL) leg type and other [2].
Primary cutaneous follicle center lymphoma (PCFCL) is a lymphoma of follicle center B cells without evidence of systemic/nodal involvement at the time of diagnosis [3].
Systemic/nodal follicular lymphomas can involve the skin and are identical in morphological appearance from PCFCL that was characterised by an indolent natural history than the secondary form of the disease, with good prognosis [4].
While the primary cutaneous involvement of lymphoma is well reported [5] only a few publications on secondary types are available [6].
Clinically, patients with systemic/nodal follicular lymphoma involving the skin present with lymphadenopathy, B symptoms, or other evidence of systemic or nodal disease [7]. However, cutaneous manifestation can be solitary or multiples localized, erythematous papules, plaques, and/or tumors on the scalp/forehead or trunk [8].
PCFCL and secondary cutaneous FL are diagnostically challenging for the pathologists since the pathologic features are often identical.However,some characteristics can help suggest skin involvement by FL.
Strong CD10 and BCL2 expression is not frequently identified in PCFCL and suggests a cutaneous involvement by FL [9].
Complete staging and work-up for B cutaneous lymphoma includes an accurate physical examination, laboratory studies (complete blood counts with lactate dehydrogenase), imaging studies (positron emission tomography/contrast-enhanced computed tomography [PET/CT] scan or computed tomography [CT] scan of chest, abdomen, or pelvis), and bone marrow aspirate and biopsy [10].
The treatment of choice for systemic follicular lymphoma is polychemotherapy and rituximab.
CONCLUSION
Complete staging is mandatory in cutaneous B lymphomas to discriminate a primary cutaneous follicle center lymphoma (PCFCL) from systemic/nodal follicular lymphoma secondarily involving the skin, to make the correct choice of treatment and to evaluate prognosis.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
REFERENCES
1. Zackheim HS, Vonderheid EC, Ramsay DL, LeBoit PE, Rothfleisch J, et al. Relative frequency of various forms of primary cutaneous lymphomas. J Am Acad Dermatol. 2000;43:793-6.
2. Steven HS, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127:2375-90.
3. Zinzani PL, Quaqlino P, Pimpinelli N, Berti E, Baliva G, Rupoli S, et al. Prognostic factors in primary cutaneous B-cell lymphoma:the Italian Study Group for Cutaneous Lymphomas. J Clin Oncol. 2006;24:1376-82.
4. Falini B, Pileri S, Zinzani PL, Carbone A, Zagonel V, Wolf-Peeters C, et al. ALK+lymphoma:clinico-pathological findings and outcome. Blood. 1999;93:2697-706.
5. Oluwole OO, Zic JA, Douds JJ, Ann Thompson M, Greer JP. Cutaneous manifestations and management of hematologic neoplasms. Semin Oncol. 2016;43:370–83.
6. Rickaby RW, Calonje E. Cutaneous involvement from systemic lymphoma. Br J Dermatol. 2015;173:12–3.
7. Senff NJ, Kluin-Nelemans HC, Willemze R. Results of bone marrow examination in 275 patients with histological features that suggest an indolent type of cutaneous B-cell lymphoma. Br J Haematol. 2008;142:52–6.
8. Skala SL, Hristov B, Hristov AC. Primary Cutaneous Follicle Center Lymphoma. Arch Pathol Lab Med. 2018;142:1313–21.
9. Swerdlow SH, Campo E, Harris NL, Stein H, Siebert R, Advani R, et al. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. Revised 4th ed. Lyon, France:IARC Press;2017. World Health Organization Classification of Tumours;vol 2.
10. Kheterpal MK, Dai J, Geller S, Pulitzer M, Ni A, Myskowski PL, et al. Role of imaging in low grade cutaneous B-cell lymphoma presenting in the skin. J Am Acad Dermatol. 2019;81:970-6.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/000-0003-3455-3810 http://orcid.org/000-0003-3455-3810 |




Comments are closed.