Annular lesions: What is your diagnosis?
Rhizlane Chaoui 1, Zakia Douhi1, Boularbah Siham1, Sara Elloudi1, Hanane Baybay1, Fatima Zahra Mernissi1, Mouna Rimani2
1, Zakia Douhi1, Boularbah Siham1, Sara Elloudi1, Hanane Baybay1, Fatima Zahra Mernissi1, Mouna Rimani2
1Department of Dermatology, University Hospital Hassan II, Fez, Morocco, 2Laboratory of Pathology Hassan Rabat, University Hospital Hassan II, Fez, Morocco
Corresponding author: Dr. Rhizlane Chaoui, E-mail: chaoui.rhizlane@gmail.com
Submission: 11.02.2020; Acceptance: 05.03.2020
DOI: 10.7241/ourd.2020e.26
Cite this article: Chaoui R, Douhi Z, Siham B, Elloudi S, Baybay H, Mernissi FZ, Rimani M. Annular lesions: What is your diagnosis? Our Dermatol Online. 2020;11(e):e26.1-e26.3.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
CASE REPORT
A 41-year-old man, he had noticed erythematous itchy lesions on his hands and neck about 5 years previously, he had puted under undocumented treatment with marked improvement. The patient reported a photosensitivity without other systemic signs and no history of drug intake.
Two months ago, Other similar lesions gradually appeared on the face, neck, the upper part of the trunk showing an annular distribution.
Clinical examination revealed an annular erythematous patch of variable size with a central clear area and crusted border involving the neck, upper back and the two arms (Figs. 1a and 1c), with a well demarcated erythematous plaques on the nose and periorbital (Fig. 2).
Dermoscopy of the lesions showed an Erythematous center with linear vessels and crust at the periphery (Fig. 3).
 |
Figure 3: Dermoscopy showed an erythematous center with linear vessels and crust at the periphery. |
Complete blood cell counts were normal. C3 and C4 complement levels were normal. Urinary protein was normal. Autoantibodies including anti-DNA, and anti-La (SS-B) were not detected.Anti-Ro (SS-A), anti-nuclear antibodies were positives.
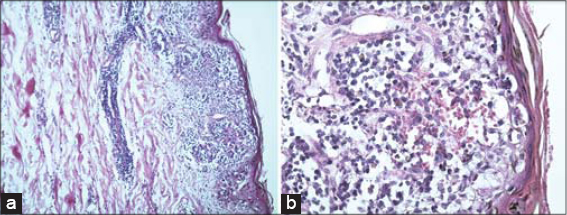
Histopathological examination of biopsy specimens from annular erythematous plaques on his neck showed an atrophic epidermis, vacuolar degeneration of the basal layer of the epidermis with formation of cytoid bodies, perifollicular and perivascular lymphocytic infiltrations in the dermis, slight mucin deposition in the superficial dermis. The histological features are those of an interface dermatitis, consistent with the clinicopathological diagnosis of subacute cutaneous lupus erythematosus (Figs. 4a and 4b).
The patient was treated with hydroxychloroquine at a dose of 200 mg twice daily (6.5 mg/kg), topical steroids in the lesion, and measures of sunscreen with good improvement.
DISCUSSION
Cutaneous lupus erythematosus (CLE) can present in three forms: acute cutaneous lupus erythematosus (ACLE,subacute cutaneous lupus erythematosus (SCLE), and chronic cutaneous lupus erythematosus (CCLE)[1].
Subacute cutaneous lupus is a non-scarring variant of lupus erythematosus which presents on the sun-exposed areas of the body. It was first described by Sontheimer in 1979 [2]. SCLE occurs primarily in young to middle aged (typically in the second to fifth decades) caucasien women and has two morphologic variants: the more common annular and the rarer papulosquamous (psoriasiform) variants.
Clinically, annular variant present as a scaly annular erythematous plaques that tend to coalesce, on the sun-exposed areas including the upper thorax and back and the extensor surfaces of the arms and forearms. It was reported that few patients with SCLE progress to SLE, but, they are likely to develop only mild systemic symptoms like Raynaud’s phenomenon and benign visceral involvement [3].
Several drugs have been reported to induce SCLE including terbinafine, TNF antagonist, anti-epileptics, proton pump inhibitor(PPI) and calcium channesl blockers (CaCB) [4].
Immunological features of SCLE include presence of anti-nuclear antibodies in patient serum and, in particular, the finding of the anti-Ro (SSA) antibody. Furthermore, few cases report the possible association between SCLE and Sjögren syndrome.
Histopathologic features include dermal edema and mucin, as well as a perivascular infiltrate by mononuclear cells. Vacuolar degeneration of the dermoepidermal junction is seen, along with epidermal atrophy [5,6]. Direct immunofluorescence may demonstrate a granular IgG pattern in SCLE [7].
Treatment options include sun avoidance measures, sun protective clothing and broad-spectrum sunscreens.
Pharmacological management includes topical or systemic steroid, hydroxychloroquine and immunosuppressants. However, systemic involvement is only observed in 20% of cases of SCLE, meaning that immunosuppressive treatment is not immediately required in most instances [8].
Good prognosis for the majority of patients with SCLE has been linked to low risk to develop systemic lupus erythematosus.
The case is being reported on account of the rarity of annular variant of lupus and its occurrence in male.
CONCLUSION
Subacute cutaneous lupus erythematosus is an uncommun variant of lupus which diagnosis is based on the clinical aspect of lesions, topography, histological finding, evolution and immunological profile of the patient.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
REFERENCES
1. Hsu S, Le EH, Khoshevis MR. Differential diagnosis of annular lesions. Am Fam Physician. 2001;64:289-96.
2. Sontheimer RD, Thomas JR, Gilliam JN. Subacute cutaneous lupus erythematosus:a cutaneous marker for a distinct lupus erythematosus subset. Arch Dermatol. 1979;115:1409-15.
3. Wieczorek IT, Propert KJ, Okawa J, Werth VP. Systemic symptoms in the progression of cutaneous to systemic lupus erythematosus. JAMA Dermatology. 2014;150:291–6.
4. Skovmøller KB, Bygum A. [When drugs induce cutaneous lupus erythematosus]. Ugeskr. Laeg. 2018;180:pii:V04180277.
5. Stavropouos PG, Goules AV, Avgerinou G, Katsambas AD. Pathogenesis of subacute cutaneous lupus erythematosus. J Eur Acad Dermatol Venereol. 2008;22:1281-9.
6. Marzano AV, Facchetti M, Alessi E. Poikilodermatous subacute cutaneous lupus erythematosus. Dermatology. 2003;207:285-90.
7. Niebower C, Tak-Diamand Z, Vanleeuwen-Wallau HE. Dust-like particles:a specific direct immunofluorescence pattern in subacute lupus erythematosus. Br J Dermatol. 1988;118:725-9.
8. Laurinaviciene R, Sandholdt LH, Bygum A. Drug-induced cutaneous lupus erythematosus:88 new cases. Eur J Dermatol. 2017;27:28–33.
Notes
Source of Support: Nil.
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/000-0003-3455-3810 http://orcid.org/000-0003-3455-3810 |





Comments are closed.