Adult-onset xanthogranuloma
Rhizlane Chaoui 1, Hanane Baybay1, Selma El Kadiri1, Zakia Douhi1, Sara Elloudi1, Fatima Zahra Mernissi1, Amal Mouaddine2, Layla Tahiri Elousrouti2, Nawal Hammas2, Laila Chbani2, Hinde Elfatemi2
1, Hanane Baybay1, Selma El Kadiri1, Zakia Douhi1, Sara Elloudi1, Fatima Zahra Mernissi1, Amal Mouaddine2, Layla Tahiri Elousrouti2, Nawal Hammas2, Laila Chbani2, Hinde Elfatemi2
1Department of Dermatology, University Hospital Hassan II, Fez, Morocco, 2Laboratory of Pathology, University Hospital Hassan II, Fez, Morocco
Corresponding author: Dr. Rhizlane Chaoui, E-mail: chaoui.rhizlane@gmail.com
Submission: 26.01.2020; Acceptance: 15.02.2020
DOI: 10.7241/ourd.2020e.17
Cite this article: Chaoui R, Baybay H, El Kadiri S, Douhi Z, Elloudi S, Mernissi FZ, Mouaddine A, Elousrouti LT, Hammas N, Chbani L, Elfatemi H. Adult-onset xanthogranuloma. Our Dermatol Online. 2020;11(e):e17.1-e17.3.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
A 34-year-old male with 4 years medical history of asthma for which he was prescibed salbutamol and fluticasone propionate/salmeterol.He presented an asymptomatic erythematous lesion on the chin for 5 months following repeated trauma from shaving.The lesion is gradually increasing in size.
Dermatological examination revealed a well-defined erythematous nodule, 10mm in diameter, with a firm consistency and smooth surface, located on the chin (Fig. 1a and b). No palpable lymphadenopathy was noted.The rest of the physical examination was normal.
 |
Figure 1. (a and b) Well-defined erythematous nodule, 10mm in diameter, with a smooth surface, located on the chin. |
On dermoscopy, we observed a yellow center with erythematous halo, characterizing the “setting sun” pattern (Fig. 2).
 |
Figure 2. Dermoscopy showing a Yellow center with erythematous halo. |
The lesion was excised under local anesthesia. Histopathological examination revealed a dense infiltrate of foamy histiocytes in the dermis admixed with many Touton giant cells (Fig. 3).
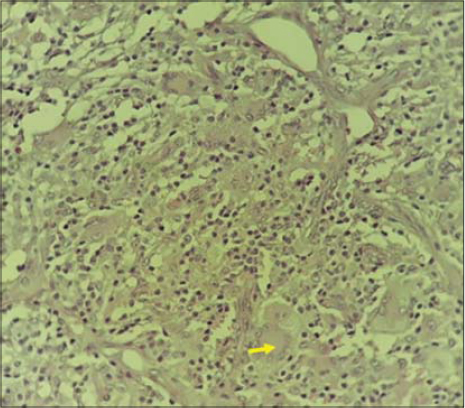 |
Figure 3. High-power magnification (40×) shows a dense infiltrate of foamy histiocytes in the dermis admixed with many Touton giant cells (Yellow arrow). |
Immunohistochemical stains were positive for anti-CD68 (Fig. 4).
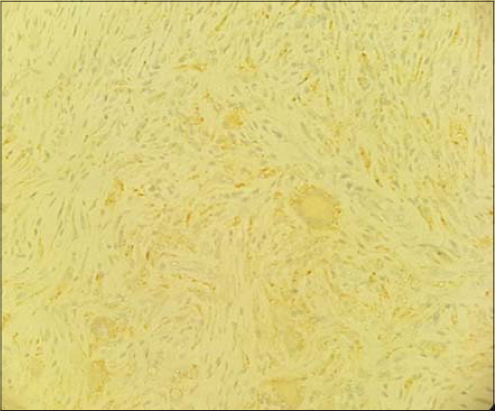 |
Figure 4. Dense infiltrate of foamy histiocytes in the dermis admixed with Touton giant cells which is strongly positive for CD68(immunohistochimy). |
These findings, in correlation with clinical and dermoscopic features were suggestive of adult xanthogranuloma.
Histiocytic disorders are classified into 3 groups based on their component cells that accumulate in the affected tissue or organ: Langerhans cell disease (class I), nonLangerhans cell histiocytic disease (class II), and malignant histiocytic disorders (class III).
The Histiocyte Society, reviewing the classification of histiocytoses, proposes the division into five groups: (1) Langerhans-related, (2) cutaneous and mucocutaneous, (3) malignant histiocytoses, (4) Rosai-Dorfman disease, and (5) hemophagocytic lymphohistiocytosis and macrophage activation syndrome [1].
Adult xanthogranuloma (AXG) or “juvenile xanthogranuloma in an adult” is a type of non-Langerhans cell histiocytic disorders. AXG usually occurs in men, at a ratio of 1.6:1,adult cases can occur, especially in patients between 20 and 30 years of age and still uncommon.Clinically, AXG is characterized by a single, dome-shaped, yellow to reddish papule or nodule with firm consistency which usually persistent. The most commonly reported site for AXG was the head and neck, followed by the trunk [2].
Dermoscopy is a non invasive tool that can help with diagnosis of adult xanthogranuloma and will show different features including discrete pigment network, whitish streaks,linear telangiectasias and fine, branched vessels, but the characteristic dermoscopic feature that has been described is “ sun dermoscopic pattern ” defined by a yellow-orange background surrounded by erythematous border [3].
Characteristic histologic findings in AXG are: foamy histiocytes in the dermis, variable presence of Touton giant cells, which are multinucleated, with homogeneous eosinophilic cytoplasmic center and xanthomatization in the periphery [4]. Immunohistochemical stains are typically positive for anti-CD68, factor XIIIa, and often anti-CD14. Langerin, CD1a, and S-100 protein immunoreactivity is typically absent [5,6].
Considering the low risk of spontaneous resolution of xanthogranuloma in adult, the treatment of choice remains surgical excision [7].
The case is being reported on account of the rarity of xanthogranuloma in adult.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
REFERENCES
1. Emile JF, Abla O, Fraitag S, Horne A, Haroche J, Donadieu J, et al. Revised classification of histiocytoses and neoplasms of the macrophage-dendritic cell lineages. Blood. 2016;127:2672-81.
2. Pajaziti L, Hapçiu S, Pajaziti A. Juvenile xanthogranuloma:a case report and review of the literature. BMC Research Notes. 2014;7:174.
3. Oliveira TE de, TarléRG, Mesquita LA de F. Dermoscopy in the diagnosis of juvenile xanthogranuloma. An Bras Dermatol. 2018;93:138–40.
4. Hollins C, Weyant G, Gibbs M, Seiverling E. An eruption of yellow-red papules on the trunk, arms, and legs of an adult. Dermatol Pract Concept. 2018;8:177–9.
5. Zelger B, Cerio R, Orchard G, Wilson-Jones E. Juvenile and adult xanthogranuloma. A histological and immunohistochemical comparison. Am J Surg Pathol. 1994;18:126-35.
6. Sonoda T, Hashimoto H, Enjoji M. Juvenile xanthogranuloma. Clinicopathologic analysis and immunohistochemical study of 57 patients. Cancer. 1985;56:2280-6.
7. Worden BF, Barrera JE, Most SP. Adult xanthogranuloma causing nasal obstruction. Arch Otolaryngol–Head Neck Surg. 2010;136:509.
Notes
Source of Support: Nil
Conflict of Interest: None
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/000-0003-3455-3810 http://orcid.org/000-0003-3455-3810 |



Comments are closed.