Scabetic leukocytoclastic vasculitis: A case report
Nadia Ghariani1, Yosra Soua 1, Hayet Akkari1, Manel Njima2, Hichem Belhadjali1, Monia Youssef1, Jameleddine Zili1
1, Hayet Akkari1, Manel Njima2, Hichem Belhadjali1, Monia Youssef1, Jameleddine Zili1
1Department of Dermatology, Fattouma Bourguiba University Hospital, Monastir, Tunisia, 2Department of Anapathology, Fattouma Bourguiba University Hospital, Monastir, Tunisia
Corresponding author: Dr. Yosra Soua
Submission: 25.01.2020; Acceptance: 30.03.2020
DOI: 10.7241/ourd.2020e.57
Cite this article: Ghariani N, Soua Y, Akkari H, Njima M, Belhadjali H, Youssef M, Zili J. Scabetic leukocytoclastic vasculitis: A case report. Our Dermatol Online. 2020;11(e):e57.1-e57.3.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Scabies is a common contagious ectoparasitosis. The most specific lesions are burrows. Vascular purpura has rarely been described. We report a new case of scabetic leukocytoclastic vasculitis. A 49-year-old woman, presented with a 2-week history of painful necrotic purpura on her legs. Physical examination revealed concomitant scabies infection. Histologic examination of a purpuric lesion revealed dermic necrosis, leukocytoclasia, and thrombotic vessels. Hematologic, blood chemical, viral serologic and immunologic studies were normal or negative. Treatment with topical benzyl benzoate lotion resolved the itchiness and led to the rapid disappearance of purpuric lesions within a few days. The association of scabies and leukocytoclastic vasculitis is uncommon. A few cases of leukocytoclastic vasculitis have been reported previously. Although histologic examination has not identified the scabies mite into the lesion of purpura, we could argue that the leukocytoclastic vasculitis is associated to the scabies infection, since purpuric lesions disappeared rapidly after applying the treatment of scabies in the absence of any other specific therapeutics.
Key words: Scabies; Leukocytoclastic vasculitis; Vascular purpura.
INTRODUCTION
Scabies is a common contagious ectoparasitosis, caused by Sarcoptes scabiei variation hominis. Its most specific lesions are burrows and scabietic nodules. Crusts, eczematous changes, folliculitis or impetigo are secondary features that may make the diagnosis less easy [1]. Leukocytoclastic vasculitis (LCV) has been reported in a few cases [2].
CASE REPORT
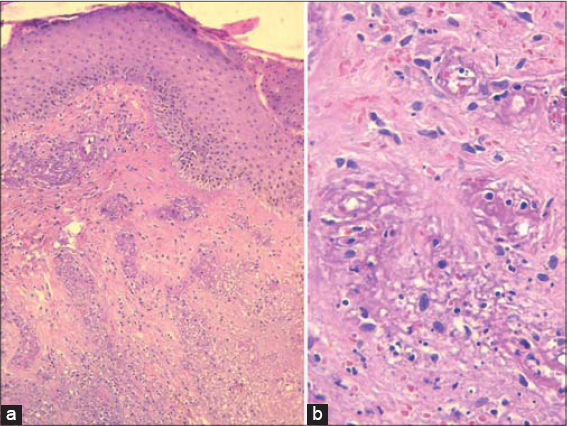
A 49-year-old woman presented with a 2-week history of painful necrotic purpura on her legs preceded by a 3-month history of a generalized, intensely pruritic eruption. She had no recent drug intake. Physical examination revealed palpable purpura with bullous and necrotic centers on both legs (Fig. 1). There were multiple erythematous papules, eczematous plaques, and excoriations on her arms, breasts, buttocks, legs and abdomen (Fig. 2). Burrows were found on the interdigital webs of her hands. A scabies mite was isolated from one of the burrows on the hand, by skin scraping. A biopsy specimen of a purpuric lesion was obtained from the leg. Histologic examination showed an inflammatory cell infiltrate, composed of neutrophils, eosinophils and lymphocytes, within and around vessel walls. Epidermic and dermic necrosis, leukocytoclasia and thrombotic vessels were also observed (Fig. 3). Platelet count was normal. Serological and virological tests were negative for (HIV, HBs Ag, anti-HCV, CMV, EBV, parvovirus B19, Chlamydia pneumoniae). Screening for antinuclear antibodies (ANA), anti-neutrophilic cytoplasmic antibodies (ANCA) and cryoglobulin was negative. Electrophoresis of serum proteins and complement fragments was normal. No proteinuria was seen. The patient was treated with topical benzyl benzoate lotion. Complete regression of itchiness and purpuric lesions had occurred within a few days. No additional skin lesions developed.
DISCUSSION
Leukocytoclastic vasculitis is an inflammation of small vessels, characterized by an inflammatory infiltrate associated with a leukocytoclasia and fibrinoid necrosis in the postcapillary venules of small vessels [3,4].
It is the most common cutaneous vasculitis [5]. VLC often manifests clinically by palpable purpura on the lower limbs. It is considered to be a hypersensitivity reaction mediated by immune complexes [6,7]. Its causes include infections, medications, and systemic diseases [7].
In our patient, the etiological investigation was negative. On the other hand, the diagnosis of the gale was confirmed by microscopic examination of the parasitology sample. Although histologic examination has not identified the scabies mite into the lesion of purpura, we could argue that the LCV is caused by the scabies infection, since The purpura improved immediately after scabies treatment, without any specific treatment for the vasculitis. [6,8].
Common histopathological findings of scabies include epidermic spongiosis, perivascular dermal infiltrate with numerous eosinophils, and mites or eggs in the stratum corneum.
The association of scabies and leukocytoclastic vasculitis is rare but not exceptional, as twelve cases have been reported until now [9]. A recent review including 25 biopsies in patients with scabies infection, identified leukocytoclastic vasculitis in 4% of cases [10].
Most of the patients were immunocompetent. Two cases were associated with focal glomerulonephritis [6], and a third case was described in an HIV-seropositive man [5].
The pathogeny of scabietic vasculitis is not well elucited. An humeral hypersensitivity reaction involving the formation of circulating antigen-antibody immune complexes was suggested [10]. Excoriations led to the penetration of antigenic debris into the bloodstream. That’s why some authors suggested that older scabies lesions are more likely to develop vasculitis [11]. Authors hypothesized that the persistence of mites and their products caused by a delay in the diagnosis, inducing sensitization, could result in the development of the LCV [10,11]. The case of our patient sustains this report, since she developed LCV after a 3-month history of scabies.
CONCLUSION
The diagnosis of scabies must be considered among the etiologies of leukocytoclastic vasculitis. Practitioners should start antiscabeitic treatment and avoid further investigations.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
REFERENCES
1. Hicks MI, Elston DM. Scabies. Dermatol Ther. 2009;22:279-92.
2. Clevy C, Brajon D, Combes E, Benzaquen M, Dales JP, Koeppel MC, Berbis P. Scabietic vasculitis:Report of 2 cases. Ann Dermatol Venereol. 2017;144:349-55.
3. Goeser MR, Laniosz V, Wetter DA. A practical approach to the diagnosis, evaluation, and management of cutaneous small-vessel vasculitis. Am J Clin Dermatol. 2014;15:299-306.
4. Sunderkötter C, Sindrilaru A. Clinical classification of vasculitis. Eur J Dermatol. 2006;16:114-24.
5. Valks R, Buezo GF, Dauden E. Scabies and leukocytoclastic vasculitis in an HIV-seropositive man. Int J Dermatol. 1996;35:605-6.
6. MennéT, Christophersen J, Gram N, Bjerrehus T. Scabietic leucocytoclastic vasculitis with focal glomerulonephritis. Acta DermVenereol (Stockh). 1984;64:445-7.
7. Jarrett P, Snow J. Scabies presenting as a necrotizing vasculitis in the presence of lupus anticoagulant. Br J Dermatol. 1998;139:701-3.
8. Stinco G, Governatori G, Interstimone D, Frattasio A, Patrone P. Scabetic leukocytoclastic vasculitis. Eur J Dermatol. 2008;18:479-81.
9. Nishihara K, Shiraishi K, Sayama K. Leukocytoclastic vasculitis associated with crusted scabies. Eur J Dermatol. 2018;28:242-3.
10. Elwood H, Berry RS, Gardner JM, Shalin SC. Superficial fibrin thrombi….and other findings:A review of the histopathology of human scabetic infections. J CutanPathol. 2015;42:346-52.
11. Liu HN, Sheu WJ, Chu TL. Scabietic nodules:a dermatopathologic and immunofluorescent study. J Cutan Pathol. 1992;19:124-7.
Notes
Source of Support: Nil.
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|





Comments are closed.