Brown macule on the sole – What’s your diagnosis?
Catarina Soares Queirós, Miguel Duarte Reis, Paulo Leal Filipe
Dermatology and Venereology Department, Hospital de Santa Maria, Centro Hospitalar e Universitário de Lisboa Norte, Portugal
Corresponding author: Dr. Catarina Soares Queirós, E-mail: catarina.squeiros@gmail.com
Submission: 25.11.2018; Acceptance: 20.12.2018
DOI: 10.7241/ourd.2018e.7
How to cite this article: Queirós CS, Reis MD, Filipe PL. Brown macule on the sole – What’s your diagnosis? Our Dermatol Online. 2018;9(e):e7.1-e7.2.
CASE REPORT
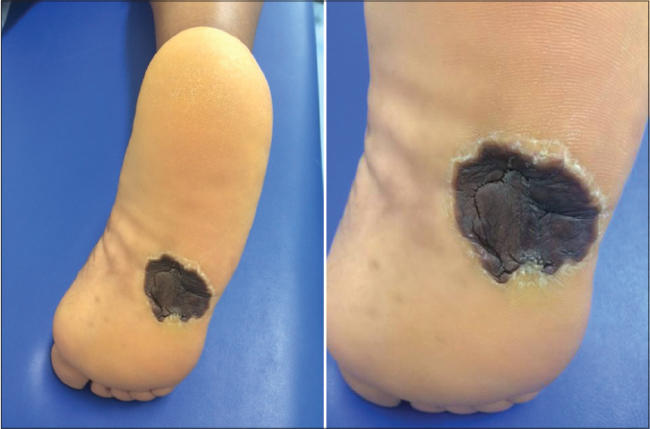
A 50-year-old African woman, Fitzpatrick skin phototype VI, presented to our outpatient clinic in July 2017 complaining of a pigmented lesion on her left sole, with progressive growth over the last few months. Physical examination revealed a dark-brown macule with different shades of tan, brown and black, a maximum diameter of 2 cm and irregular borders. The patient underwent surgical excision of the lesion, and histopathological examination confirmed the diagnosis of an acral lentiginous in situ malignant melanoma, which intercepted the surgical margin laterally. As a result, she was referred to Plastic Surgery for a wider excision with safety margins, and closure was performed with a skin graft. Three months after this surgery, the patients comes again to our outpatient clinic for a follow-up visit; she complains of pain and itching in the middle third of her left sole. Physical examination now reveals a brown, round macule, approximately 4 cm in diameter, with well-defined borders, a furrowed appearance and a hyperkeratotic border (Figs. 1a and 1b).
What’s your diagnosis?
Answer
After the first surgical excision, diagnosis of an acral lentiginous in situ malignant melanoma was made and the patient was referred to Plastic Surgery to undergo a wider excision with safety margins. Closure was performed with a skin graft from the anterior thigh, which explains the difference in colour between the patients’ sole and the graft tissue.
DISCUSSION
Acral lentiginous melanoma represents only 2-8% of melanomas in whites but is the most common type of melanoma among dark-skinned people, representing 35-60% of melanomas in this population [1,2]. This type of melanoma usually appears on the palms and soles, usually as flat, tan or brown macules with irregular borders [3]. In dark-skinned patients, the preferential location of melanoma on the palms and soles may be related to a different pattern of melanossome distribution among keratinocytes in the skin of these regions [4]. Due to the delay in diagnosis and frequent advanced state at presentation, acral lentiginous melanoma tends to have a poor prognosis [2].
Acral lentiginous melanomas are often poorly defined and multifocal, with frequent discrepancies between clinical observation and histopathologic margins. This makes local recurrences more common in this type of melanoma [3]. Therefore, surgical excision should be attempted with increased safety margins (at least 1 cm) or with narrow margins and micrographic control (e.g., Mohs’ micrographic surgery) [5]. Although immune checkpoint inhibitors and BRAF/MEK inhibitors have been responsible for a significant improvement in overall survival of patients with advanced melanoma, acral lentiginous melanoma may be less susceptible to these therapies because of the poor immune response to the tumour and infrequent BRAF mutation [6].
As for any type of melanoma, follow-up after surgical excision is of major importance. The frequency and extent of follow-up examinations will vary according to the primary tumour characteristics, but these are usually more regular during the first 5 years [5]. The goals of these follow-up examinations include identifying any tumour recurrence or disease progression at the earliest stage, as well as providing education to the patient and family about the importance of total skin examination [3]. In our patient, follow-up may be a challenge due to the graft skin tone, a fact that makes regular appointments even more important in order to identify any change as earlier as possible.
REFERENCES
1. American Cancer Society. What Are the Key Statistic About Melanoma? Detailed Guide: Skin Cancer – Melanoma. 2018.
2. Liu XK, Li J. Acral lentiginous melanoma. Lancet. 2018;391:e21.
3. Park HS, Cho KH. Acral lentiginous melanoma in situ: a diagnostic and management challenge. Cancers (Basel). 2010;2:642-52.
4. Milburn PB, Sian CS, Silvers DN. The color of the skin of the palms and soles as a possible clue to the pathogenesis of acral-lentiginous melanoma. Am J Dermatopathol. 1982;4:429-33.
5. Garbe C, Peris K, Hauschild A, Saiag P, Middleton M, Bastholt L, et al. Diagnosis and treatment of melanoma. European consensus-based interdisciplinary guideline – Update 2016. Eur J Cancer. 2016;63:201-17.
6. Nakamura Y, Fujisawa Y. Diagnosis and Management of Acral Lentiginous Melanoma. Curr Treat Options Oncol. 2018;19:42.
Notes
Source of Support: Nil
Conflict of Interest: None declared.
Comments are closed.